IEC TR 62799:2013
(Main)Models for evaluation of thermal hazard in medical diagnostic ultrasonic fields
Models for evaluation of thermal hazard in medical diagnostic ultrasonic fields
IEC/TR 62799:2013(E), which is a technical report, provides background information for users of IEC 62359 to understand the relative merits of several of the potential replacements for the thermal index as described in IEC 60601-2-37 and IEC 62359. The report discusses parameters related to thermal aspects of diagnostic ultrasonic fields; and methods for the determination of an exposure parameter relating to temperature rise in theoretical tissue-equivalent models, resulting from absorption of ultrasound. The report is intended to be used:
- by those involved in the development and maintenance of IEC 62359;
- manufacturers of medical electrical equipment for risk assessment;
- and health care regulatory authorities, test houses and other organizations responsible for implementing standards for medical electrical equipment.
General Information
- Status
- Published
- Publication Date
- 16-Sep-2013
- Technical Committee
- TC 87 - Ultrasonics
- Drafting Committee
- WG 14 - TC 87/WG 14
- Current Stage
- PPUB - Publication issued
- Start Date
- 17-Sep-2013
- Completion Date
- 30-Nov-2013
Overview
IEC TR 62799:2013 - Models for evaluation of thermal hazard in medical diagnostic ultrasonic fields is a technical report that provides background and modelling guidance to support users of IEC 62359 in evaluating thermal effects from diagnostic ultrasound. The report reviews the limitations of the current Thermal Index (TI) as used in IEC 60601-2-37 and describes methods and exposure parameters for estimating temperature rise in theoretical tissue‑equivalent models due to acoustic absorption. It compares several potential replacements or refinements to the TI to improve ultrasound thermal hazard assessment.
Key topics covered
- Purpose and scope: Background information for standards developers, manufacturers and regulators on thermal exposure parameters and models.
- Thermal modelling fundamentals: Discussion of acoustic parameters such as acoustic absorption and attenuation, and how these affect tissue heating.
- Limitations of the existing TI: Identifies issues including linear display assumptions, equilibrium temperature concepts, variability of tissue parameters, transducer self‑heating and current safety limits.
- Alternative exposure metrics: Evaluation of candidate replacements or enhancements to TI, including but not limited to:
- Exponential display of TI
- Thermally Equivalent Time Index (TETI)
- Time to Threshold (TT)
- Safe Use Time (SUT)
- Thermally Equivalent Time Display (TETD)
- Methods for determination: Procedures to determine exposure parameters relating to temperature rise using theoretical tissue‑equivalent models and illustrative results for each option.
- Recommendations: Guidance for applying models in standards development and device risk assessment.
Practical applications and users
IEC TR 62799 is intended for:
- Standards committees and developers (for maintenance and evolution of IEC 62359)
- Medical device manufacturers (for thermal risk assessment, design decisions, and labelling)
- Regulatory authorities and test houses (for implementing test methods and compliance checks)
- Clinical engineers and safety assessors (to interpret TI and alternative indices in context of patient exposure)
Typical uses:
- Selecting or justifying an exposure metric for device safety documentation
- Implementing test procedures that estimate temperature rise in tissue models
- Informing software/display choices for thermal indices on ultrasound equipment
- Supporting regulatory submissions and conformity assessment for medical electrical equipment
Related standards
- IEC 62359: Field characterization - Test methods for determination of thermal and mechanical indices
- IEC 60601‑2‑37: Particular requirements for ultrasonic medical diagnostic equipment
- IEC 62127‑1 / IEC 62127‑2: Hydrophone measurements and calibration (relevant to field characterization)
Keywords: IEC TR 62799, thermal hazard, diagnostic ultrasound, thermal index, TETI, temperature rise, IEC 62359, IEC 60601‑2‑37, ultrasound safety, exposure parameter.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
IEC TR 62799:2013 is a technical report published by the International Electrotechnical Commission (IEC). Its full title is "Models for evaluation of thermal hazard in medical diagnostic ultrasonic fields". This standard covers: IEC/TR 62799:2013(E), which is a technical report, provides background information for users of IEC 62359 to understand the relative merits of several of the potential replacements for the thermal index as described in IEC 60601-2-37 and IEC 62359. The report discusses parameters related to thermal aspects of diagnostic ultrasonic fields; and methods for the determination of an exposure parameter relating to temperature rise in theoretical tissue-equivalent models, resulting from absorption of ultrasound. The report is intended to be used: - by those involved in the development and maintenance of IEC 62359; - manufacturers of medical electrical equipment for risk assessment; - and health care regulatory authorities, test houses and other organizations responsible for implementing standards for medical electrical equipment.
IEC/TR 62799:2013(E), which is a technical report, provides background information for users of IEC 62359 to understand the relative merits of several of the potential replacements for the thermal index as described in IEC 60601-2-37 and IEC 62359. The report discusses parameters related to thermal aspects of diagnostic ultrasonic fields; and methods for the determination of an exposure parameter relating to temperature rise in theoretical tissue-equivalent models, resulting from absorption of ultrasound. The report is intended to be used: - by those involved in the development and maintenance of IEC 62359; - manufacturers of medical electrical equipment for risk assessment; - and health care regulatory authorities, test houses and other organizations responsible for implementing standards for medical electrical equipment.
IEC TR 62799:2013 is classified under the following ICS (International Classification for Standards) categories: 11.040.50 - Radiographic equipment; 33.200 - Telecontrol. Telemetering. The ICS classification helps identify the subject area and facilitates finding related standards.
IEC TR 62799:2013 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
IEC/TR 62799 ®
Edition 1.0 2013-09
TECHNICAL
REPORT
Models for evaluation of thermal hazard in medical diagnostic ultrasonic fields
IEC/TR 62799:2013(E)
All rights reserved. Unless otherwise specified, no part of this publication may be reproduced or utilized in any form
or by any means, electronic or mechanical, including photocopying and microfilm, without permission in writing from
either IEC or IEC's member National Committee in the country of the requester.
If you have any questions about IEC copyright or have an enquiry about obtaining additional rights to this publication,
please contact the address below or your local IEC member National Committee for further information.
IEC Central Office Tel.: +41 22 919 02 11
3, rue de Varembé Fax: +41 22 919 03 00
CH-1211 Geneva 20 info@iec.ch
Switzerland www.iec.ch
About the IEC
The International Electrotechnical Commission (IEC) is the leading global organization that prepares and publishes
International Standards for all electrical, electronic and related technologies.
About IEC publications
The technical content of IEC publications is kept under constant review by the IEC. Please make sure that you have the
latest edition, a corrigenda or an amendment might have been published.
Useful links:
IEC publications search - www.iec.ch/searchpub Electropedia - www.electropedia.org
The advanced search enables you to find IEC publications The world's leading online dictionary of electronic and
by a variety of criteria (reference number, text, technical electrical terms containing more than 30 000 terms and
committee,…). definitions in English and French, with equivalent terms in
It also gives information on projects, replaced and additional languages. Also known as the International
withdrawn publications. Electrotechnical Vocabulary (IEV) on-line.
IEC Just Published - webstore.iec.ch/justpublished Customer Service Centre - webstore.iec.ch/csc
Stay up to date on all new IEC publications. Just Published If you wish to give us your feedback on this publication
details all new publications released. Available on-line and or need further assistance, please contact the
also once a month by email. Customer Service Centre: csc@iec.ch.
IEC/TR 62799 ®
Edition 1.0 2013-09
TECHNICAL
REPORT
Models for evaluation of thermal hazard in medical diagnostic ultrasonic fields
INTERNATIONAL
ELECTROTECHNICAL
COMMISSION
PRICE CODE
X
ICS 11.040.50 ISBN 978-2-8322-1099-4
– 2 – TR 62799 © IEC:2013(E)
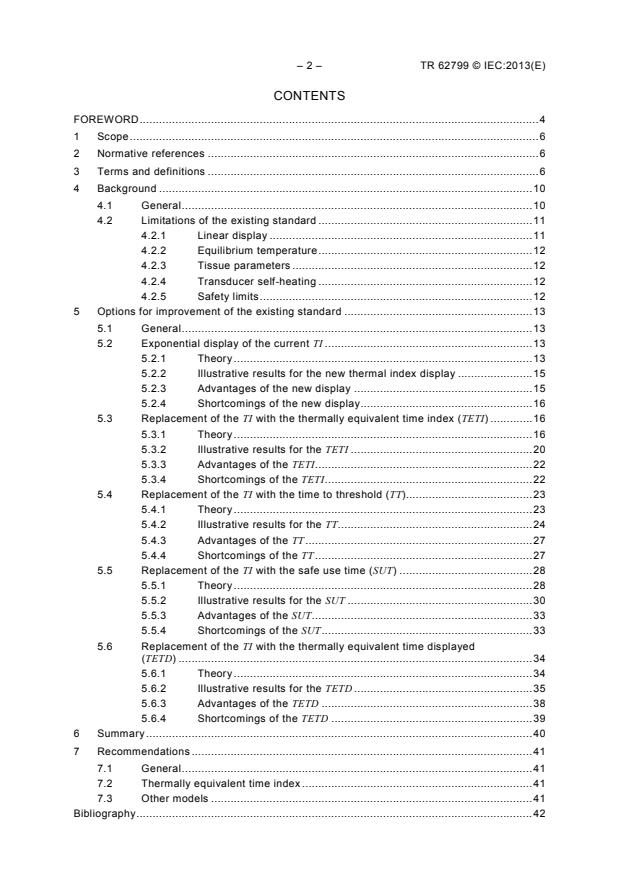
CONTENTS
FOREWORD . 4
1 Scope . 6
2 Normative references . 6
3 Terms and definitions . 6
4 Background . 10
4.1 General . 10
4.2 Limitations of the existing standard . 11
4.2.1 Linear display . 11
4.2.2 Equilibrium temperature . 12
4.2.3 Tissue parameters . 12
4.2.4 Transducer self-heating . 12
4.2.5 Safety limits . 12
5 Options for improvement of the existing standard . 13
5.1 General . 13
5.2 Exponential display of the current TI . 13
5.2.1 Theory . 13
5.2.2 Illustrative results for the new thermal index display . 15
5.2.3 Advantages of the new display . 15
5.2.4 Shortcomings of the new display . 16
5.3 Replacement of the TI with the thermally equivalent time index (TETI) . 16
5.3.1 Theory . 16
5.3.2 Illustrative results for the TETI . 20
5.3.3 Advantages of the TETI. 22
5.3.4 Shortcomings of the TETI . 22
5.4 Replacement of the TI with the time to threshold (TT). 23
5.4.1 Theory . 23
5.4.2 Illustrative results for the TT. 24
5.4.3 Advantages of the TT . 27
5.4.4 Shortcomings of the TT . 27
5.5 Replacement of the TI with the safe use time (SUT) . 28
5.5.1 Theory . 28
5.5.2 Illustrative results for the SUT . 30
5.5.3 Advantages of the SUT . 33
5.5.4 Shortcomings of the SUT . 33
5.6 Replacement of the TI with the thermally equivalent time displayed
(TETD) . 34
5.6.1 Theory . 34
5.6.2 Illustrative results for the TETD . 35
5.6.3 Advantages of the TETD . 38
5.6.4 Shortcomings of the TETD . 39
6 Summary . 40
7 Recommendations . 41
7.1 General . 41
7.2 Thermally equivalent time index . 41
7.3 Other models . 41
Bibliography . 42
TR 62799 © IEC:2013(E) – 3 –
Figure 1 – Comparison of the values of thermal index that would be displayed under
the proposed definition, TI , with that displayed currently, TI . 15
new cur
Figure 2 –Expanded view of the comparison of Figure 1 for smaller values of TI . 15
cur
Figure 3 – Thermal-equivalent core temperature elevations vs time . 18
Figure 4 – Temperature-time curve (solid line) that represents a conservative boundary
for non-foetal exposure durations, particularly for exposure durations of less than 5 s . 19
Figure 5 – Thermally equivalent time index (solid curves) vs foetal exposure duration
for TI = 1, 2, 3 and 4 . 21
Figure 6 – Temperature rise for distance (z > 3 cm) for four models as a function of
US exposure time . 25
Figure 7 – Relation between TT (time to threshold) and power parameters that give a
temperature rise of ∆T = 4 °C. 26
thr
Figure 8 – The ratio of temperature rise to acoustic absorption coefficient, ∆T/µ, vs
exposure duration for the non-scanning soft tissue model with P = 100 mW. . 27
a
Figure 9 – A typical example of temperature rise due to diagnostic ultrasound . 29
Figure 10 – Values of temperature rise as a function of insonation time . 31
Figure 11 – The thermal load as a function of time and f-number . 32
Figure 12 – A comparison of thermally equivalent times (t ) for the temperature
profiles shown in Figure 6 . 36
Figure 13 – Probability of birth defect or kidney necrosis as a function of thermally
equivalent time (t ) . 37
Figure 14 – Probabilities of kidney necrosis estimated for the thermally equivalent
times (t ) shown in Figure 12 . 38
Figure 15 – Probabilities of birth defect estimated for the thermally equivalent times
(t ) shown in Figure 12 . 39
Table 1 – Thermally equivalent time thresholds for chronic damage in various tissues,
t ; see [21]. . 20
Table 2 – Foetal exposure durations for a thermally equivalent time index value of 1 . 22
Table 3 – Non-foetal exposure durations for a thermally equivalent time index value
of 1 . 22
Table 4 – SUT values when including and ignoring the contribution of temperatures
lower than ∆T for the four exposure conditions and the corresponding values of
max
∆T . 32
max
Table 5 – Values of W, W , and ∆T for the case of SUT = 500 s. . 33
a max
Table 6 – Comparison of significant characteristics of the possible replacements for
the TI. . 40
– 4 – TR 62799 © IEC:2013(E)
INTERNATIONAL ELECTROTECHNICAL COMMISSION
____________
MODELS FOR EVALUATION OF THERMAL HAZARD
IN MEDICAL DIAGNOSTIC ULTRASONIC FIELDS
FOREWORD
1) The International Electrotechnical Commission (IEC) is a worldwide organization for standardization comprising
all national electrotechnical committees (IEC National Committees). The object of IEC is to promote
international co-operation on all questions concerning standardization in the electrical and electronic fields. To
this end and in addition to other activities, IEC publishes International Standards, Technical Specifications,
Technical Reports, Publicly Available Specifications (PAS) and Guides (hereafter referred to as “IEC
Publication(s)”). Their preparation is entrusted to technical committees; any IEC National Committee interested
in the subject dealt with may participate in this preparatory work. International, governmental and non-
governmental organizations liaising with the IEC also participate in this preparation. IEC collaborates closely
with the International Organization for Standardization (ISO) in accordance with conditions determined by
agreement between the two organizations.
2) The formal decisions or agreements of IEC on technical matters express, as nearly as possible, an international
consensus of opinion on the relevant subjects since each technical committee has representation from all
interested IEC National Committees.
3) IEC Publications have the form of recommendations for international use and are accepted by IEC National
Committees in that sense. While all reasonable efforts are made to ensure that the technical content of IEC
Publications is accurate, IEC cannot be held responsible for the way in which they are used or for any
misinterpretation by any end user.
4) In order to promote international uniformity, IEC National Committees undertake to apply IEC Publications
transparently to the maximum extent possible in their national and regional publications. Any divergence
between any IEC Publication and the corresponding national or regional publication shall be clearly indicated in
the latter.
5) IEC itself does not provide any attestation of conformity. Independent certification bodies provide conformity
assessment services and, in some areas, access to IEC marks of conformity. IEC is not responsible for any
services carried out by independent certification bodies.
6) All users should ensure that they have the latest edition of this publication.
7) No liability shall attach to IEC or its directors, employees, servants or agents including individual experts and
members of its technical committees and IEC National Committees for any personal injury, property damage or
other damage of any nature whatsoever, whether direct or indirect, or for costs (including legal fees) and
expenses arising out of the publication, use of, or reliance upon, this IEC Publication or any other IEC
Publications.
8) Attention is drawn to the Normative references cited in this publication. Use of the referenced publications is
indispensable for the correct application of this publication.
9) Attention is drawn to the possibility that some of the elements of this IEC Publication may be the subject of
patent rights. IEC shall not be held responsible for identifying any or all such patent rights.
The main task of IEC technical committees is to prepare International Standards. However, a
technical committee may propose the publication of a technical report when it has collected
data of a different kind from that which is normally published as an International Standard, for
example "state of the art".
IEC 62799, which is a technical report, has been prepared by IEC technical committee 87:
Ultrasonics.
The text of this technical report is based on the following documents:
Enquiry draft Report on voting
87/510/DTR 87/537/RVC
Full information on the voting for the approval of this technical report can be found in the
report on voting indicated in the above table.
This publication has been drafted in accordance with the ISO/IEC Directives, Part 2.
TR 62799 © IEC:2013(E) – 5 –
Terms appearing in bold print in the text are defined in Clause 3 of this technical report.
The committee has decided that the contents of this publication will remain unchanged until
the stability date indicated on the IEC web site under "http://webstore.iec.ch" in the data
related to the specific publication. At this date, the publication will be
• reconfirmed,
• withdrawn,
• replaced by a revised edition, or
• amended.
A bilingual version of this publication may be issued at a later date.
– 6 – TR 62799 © IEC:2013(E)
MODELS FOR EVALUATION OF THERMAL HAZARD
IN MEDICAL DIAGNOSTIC ULTRASONIC FIELDS
1 Scope
This technical report provides background information for users of IEC 62359 to understand
the relative merits of several of the potential replacements for the thermal index (TI) as
described in IEC 60601-2-37 and IEC 62359.
The report discusses:
– parameters related to thermal aspects of diagnostic ultrasonic fields;
– methods for the determination of an exposure parameter relating to temperature rise in
theoretical tissue-equivalent models, resulting from absorption of ultrasound.
The report is intended to be used by:
– those involved in the development and maintenance of IEC 62359;
– manufacturers of medical electrical equipment for risk assessment;
– health care regulatory authorities, test houses and other organizations responsible for
implementing standards for medical electrical equipment.
2 Normative references
The following documents, in whole or in part, are normatively referenced in this document and
are indispensable for its application. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any
amendments) applies.
IEC 60601-2-37:2007, Medical electrical equipment – Part 2-37: Particular requirements for
the basic safety and essential performance of ultrasonic medical diagnostic and monitoring
equipment
IEC 62127-1:2007, Ultrasonics – Hydrophones – Part 1: Measurement and characterization of
medical ultrasonic fields up to 40 MHz
IEC 62127-2, Ultrasonics – Hydrophones – Part 2: Calibration for ultrasonic fields up to
40 MHz
IEC 62359:2010, Ultrasonics – Field characterization – Test methods for the determination of
thermal and mechanical indices related to medical diagnostic ultrasonic fields
3 Terms and definitions
For the purposes of this technical report, the terms and definitions given in IEC 60601-2-37,
IEC 62127-1, IEC 62127-2 and IEC 62359, some of which are repeated below for
convenience, and the following terms and definitions apply.
3.1
acoustic absorption coefficient
µ
quantity intended to account for loss of ultrasonic energy to tissue at a specified point by
mechanisms other than scattering
TR 62799 © IEC:2013(E) – 7 –
-1
Note 1 to entry: Acoustic absorption coefficient is expressed in nepers per centimetre (Np cm ).
Note 2 to entry: The acoustic absorption coefficient must be less than or equal to the acoustic attenuation
coefficient.
3.2
acoustic attenuation coefficient
α
quantity intended to account for reduction of energy of an acoustic wave by all mechanisms
involving interaction of the wave and all matter between the source and a specified point
-1
Note 1 to entry: Acoustic attenuation coefficient is expressed in nepers per centimetre (Np cm ).
Note 2 to entry: The acoustic attenuation coefficient must be greater than or equal to the acoustic absorption
coefficient.
Note 3 to entry: The acoustic attenuation coefficient does not account for geometric attenuation.
3.3
acoustic working frequency
f
awf
frequency of an acoustic signal based on the observation of the output of a hydrophone
placed in an acoustic field at the position corresponding to the spatial-peak temporal-peak
acoustic pressure
Note 1 to entry: The signal is analysed using either the zero-crossing acoustic-working frequency technique or
a spectrum analysis technique. Acoustic working frequencies are defined in 3.3.1 and 3.3.2.
Note 2 to entry: In a number of cases the present definition is not very helpful or convenient, especially for
broadband transducers. In that case a full description of the frequency spectrum should be given in order to enable
any frequency-dependent correction to the signal.
Note 3 to entry: Acoustic working frequency is expressed in hertz (Hz).
SOURCE: IEC 62127-1:2007, 3.3.
3.3.1
zero-crossing acoustic working frequency
number, n, of consecutive half-cycles (irrespective of polarity) divided by twice the time
between the commencement of the first half-cycle and the end of the n-th half-cycle
Note 1 to entry: Any half-cycle in which the waveform shows evidence of phase change shall not be counted.
Note 2 to entry: The measurement should be performed at terminals in the receiver that are as close as possible
to the receiving transducer (hydrophone) and, in all cases, before rectification.
Note 3 to entry: This frequency is determined according to the procedure specified in IEC/TR 60854.
Note 4 to entry: This frequency is intended for continuous wave systems only.
3.3.2
arithmetic-mean acoustic working frequency
arithmetic mean of the most widely separated frequencies f and f , within the range of three
1 2
times f , at which the magnitude of the acoustic pressure spectrum is 3 dB below the peak
magnitude
Note 1 to entry: This frequency is intended for pulse-wave systems only.
Note 2 to entry: It is assumed that f < f .
1 2
Note 3 to entry: If f is not found within the range < 3 f , f is to be understood as the lowest frequency above this
2 1 2
range at which the spectrum magnitude is -3dB from the peak magnitude.
– 8 – TR 62799 © IEC:2013(E)
3.4
non-scanning mode
mode of operation of a system that involves a sequence of ultrasonic pulses which give rise to
ultrasonic scan lines that follow the same acoustic path
SOURCE: IEC 62127-1:2007, 3.39.4.
3.5
peak-rarefactional acoustic pressure
p p
-; r
maximum of the modulus of the negative instantaneous acoustic pressure in an acoustic field
or in a specified plane during an acoustic repetition period
Note 1 to entry: Peak-rarefactional acoustic pressure is expressed as a positive value.
Note 2 to entry: Peak-rarefactional acoustic pressure is expressed in pascal (Pa).
Note 3 to entry: The definition of peak-rarefactional acoustic pressure also applies to peak-negative acoustic
pressure, which is also in use in literature.
SOURCE: IEC 62127-1:12007, 3.44.
3.6
safe use time
SUT
maximum duration of exposure in a region at a particular output level that would be no more
hazardous than scanning at a specified threshold exposure
Note 1 to entry: Safe use time is expressed in seconds (s).
3.7
scanning mode
mode of operation of a system that involves a sequence of ultrasonic pulses which give rise to
ultrasonic scan lines that do not follow the same acoustic path
Note 1 to entry: The sequence of pulses is not necessarily made up of identical pulses. For instance, the use of
sequential multiple focal-zones is considered a scanning mode.
SOURCE: IEC 62127-1:2007, 3.39.5.
3.8
temperature rise
∆T
difference between the instantaneous temperature and the normal physiological temperature
of the subject
Note 1 to entry: Temperature rise is expressed in degrees Celsius ( °C).
Note 2 to entry: Temperature rise may be either positive or negative.
3.9
thermally equivalent time
t
at a constant temperature of 43 °C, duration of exposure required to produce the same
magnitude of a thermally induced bio-effect, i.e., an "iso-effect", as is produced by an
exposure of duration t' at a different temperature T that may vary in time
The thermally equivalent time (t ) is defined mathematically as:
t'
[T(t)−43°C] C
T
t = R dt
∫
TR 62799 © IEC:2013(E) – 9 –
where:
C = 1 °C, a constant to render the exponent dimensionless;
T
T(t) = temperature (which may vary in time) producing the bioeffect;
t = time;
t’ = time required to produce the bioeffect at temperature T;
R = thermal normalization constant, equal to 4,0 if T ≤ 43 °C;
R = thermal normalization constant, equal to 2,0 if T > 43 °C
Note 1 to entry: In the scientific and medical literature, thermally equivalent time is commonly called “thermal
dose”.
(T −T ) 1°C
2 1
t t = R
1 2
Note 2 to entry: The general expression for thermally equivalent time is , where R is the
thermal normalization constant. Because R varies with both temperature and species, as well as among different
tissues within the same species, it must be determined empirically. For simplicity, the values for R are usually fixed
at R = 2 for T > 43 °C and R = 4 for T ≤ 43 °C. More generally, T1 is a constant reference temperature, and T2 is a
function of time.
Note 3 to entry: When quantifying exposure to most forms of radiation, the general term 'dose' is usually
expressed in units of absorbed energy (in joules) or specific energy (e.g., J/ kg) rather than in units of time.
Although there is a growing preference within IEC to use the more precise term ‘thermally equivalent time’, this
new term has not yet been carefully evaluated or widely accepted.
Note 4 to entry: The SI unit of thermally equivalent time is second (s).
3.10
thermally equivalent time displayed
TETD
exposure duration required to obtain a thermally equivalent time sufficient to induce harm in
a specified fraction of exposed subjects at a specified point as estimated using a specified
model
Note 1 to entry: Thermally equivalent time displayed is expressed in seconds (s).
3.11
thermally equivalent time index
thermal dose index
TETI
ratio of the thermally equivalent time calculated assuming that T(t) = (TI + 37) × 1 °C and
R = 4 to a thermally equivalent time below which the risk of an adverse thermal effect is very
low.
The simplest form of the thermally equivalent time index (TETI) is given by the following
expression:
TI
(4) ⋅ t
TETI = ,
N
where:
TI = thermal index;
t = exposure duration;
N = a normalizing factor
Note 1 to entry: The normalizing factor is the thermally equivalent time below which the risk of an adverse
thermal effect is very low.
Note 2 to entry: Thermally equivalent time index is non-dimensional.
– 10 – TR 62799 © IEC:2013(E)
3.12
thermal index
TI
ratio of attenuated acoustic power at a specified point to the attenuated acoustic power
required to raise the temperature at that point in a specific model by 1 °C
SOURCE: IEC 62359, 3.56.
3.13
thermal load
TL
Thermally equivalent time calculated assuming a constant temperature equal to the value
estimated at the safe use time, a duration equal to the safe use time, R = 4, minus the safe
use time
Note 1 to entry: Thermal load is expressed in seconds (s).
3.14
threshold exposure
exposure to ultrasound which produces a specified constant temperature rise, ∆T, that is
maintained for a specified duration, t
Note 1 to entry: A threshold exposure has a thermally equivalent time. For example, if a subject having a
normal physiologic temperature of 37 °C experiences an increase in temperature to 41 °C for 4 min, then ∆T = 4 °C
and dt = 4 min, and the thermally equivalent time is 4 min × 4 = 1 024 min = 61 440 s.
3.15
threshold temperature rise
∆T
thr
minimum temperature increase above normal physiologic level required to induce harm in the
exposed tissue
Note 1 to entry: Threshold temperature rise is expressed in degrees Celsius ( °C).
3.16
time to threshold
TT
exposure duration required to raise the temperature at a specified point by the threshold
temperature rise
Note 1 to entry: Time to threshold is expressed in seconds (s).
4 Background
4.1 General
The safety of diagnostic ultrasound is currently assessed and communicated to the user
under international standards IEC 62359 and IEC 60601-2-37, respectively. Although
originally adopted in 2005 and 2003, these standards are based on work first published in
1992 as the so-called Output Display Standard (ODS), a joint effort of the American Institute
1)
of Ultrasound in Medicine and the (US) National Electrical Manufacturers Association [1] .
Much has been learned in the intervening fifteen years, and several reviews of the relevant
literature, both general [2]-[4] and specific [5], [6] have appeared since that time. Therefore it
is considered prudent to report on such aspects of this information as relate directly to
IEC 60601-2-37.
—————————
1)
Numbers in square brackets refer to the Bibliography.
TR 62799 © IEC:2013(E) – 11 –
It is well known that there are two broad categories of mechanisms whereby ultrasound may
adversely affect biological material, nonthermal (or mechanical) and thermal. As it passes
through tissue, diagnostic ultrasound necessarily induces a mechanical strain. This strain is
highest in proximity to gas or vapour bubbles, and therefore mechanical damage is most likely
to be induced where they are located. Ultrasound is also absorbed as it propagates, and the
absorbed energy produces an increase in temperature of the tissue. Depending on the
magnitude and duration of the increase, thermal damage to the tissue (or organism) may
result. The goal of this report is to examine various means of quantifying the potential for
tissue heating to damage biological tissue, and to suggest approaches for enhancing the
safety of diagnostic ultrasound.
4.2 Limitations of the existing standard
International standard IEC 62359 quantifies the likelihood that any tissue heating produced by
diagnostic ultrasound will harm a patient by requiring the calculation of a quantity called the
thermal index (TI) and the display of this calculated value on the video screen of the
equipment console. The calculation is based on one of several simplified thermal models
described in the standard. The models currently defined include those for soft tissue (TIS),
bone at the focus (TIB) and bone near the tissue surface, as for cranial bone, hence (TIC), as
well as encompassing both scanning and non-scanning imaging modes [7]. The calculated
value will depend on factors such as transmitted energy, imaging mode, beam shape, focal
depth, waveform and duty factor, but rather than displaying a specific physical parameter, the
TI indicates combinations of output settings that are more likely than others to produce an
adverse thermal effect [8].
The general form of the TI is simply the ratio of the instantaneous value of a power parameter
defined by the standard to the value of the same parameter required to produce a steady-
state temperature rise of 1 °C in the exposed tissue. Although it is tempting to consider the
value of the TI to be the actual in situ temperature rise, this is not the case. Because the
models underlying the TI were made sufficiently simple to be implemented in real time with
the limited computational power available in 1992, the TI provides only a relative indication of
the maximum possible temperature rise at a specific point along the axis of the acoustic
beam. Thus values of the TI obtained for different imaging consoles, or even with different
transducers used with the same console, cannot be compared.
Several additional inaccuracies or limitations of the TI have been identified. Some of these
were known or suspected at the time the ODS was developed [1], although their full
significance was not always completely appreciated. A number of factors directly affecting the
computational and display algorithms for the TI are discussed in the following subclauses.
Other factors, those primarily affecting the measurement of the physical quantities required
for specific calculations, are not addressed in this report.
4.2.1 Linear display
As currently defined, the TI displayed onscreen is linearly proportional to the absorbed power
or equivalently, to the in situ intensity or temperature. In contrast, the thermally equivalent
time (also ‘thermal dose’, see Note 1 to entry of 3.9), a well known empirical relationship
between the temperature T of a biological system and the time t needed for that temperature
to induce a deleterious effect, has an exponential form. Specifically, for any two temperatures,
T and T , and the corresponding exposure times t and t , required to produce the same
1 2 1 2
(T −T ) 1°C
2 1
level of effect, this general relation holds: t t = R , where R is the thermal
1 2
normalization constant. Hence, it is experimentally determined that the rate of induction, or
risk, of a thermal effect increases exponentially with temperature. There is thus a fundamental
discrepancy between the displayed value of the TI and its stated goal of quantifying thermal
risk from exposure to diagnostic ultrasound. A potential solution to this problem is suggested
in 4.1.
– 12 – TR 62799 © IEC:2013(E)
4.2.2 Equilibrium temperature
As currently defined, the TI-value displayed onscreen is based on the steady-state
temperature rise calculated for very long duration exposures from a stationary transducer.
There are two difficulties here. First, the time needed to reach the steady state depends
strongly on exposure parameters, e.g., the width of the acoustic beam, as well as various
physiological factors, e.g., the perfusion rate. Clinical users are generally ignorant of the
acoustic field they are using and can only guess at the relevant physiology. Second, in most
clinical situations the transducer is moved frequently, and a particular imaging mode may be
used for only a few tens of seconds before a different mode is selected. The AIUM suggests
considering such motion as an additional safety margin protecting the patient [9], with the size
of the margin depending on the time needed to reach the steady-state temperature rise. Most
clinical users will not be able to estimate the magnitude of the safety margin, and in fact may
not even be aware of its existence. Potential solutions to this problem are suggested in 5.3
and 5.4.
4.2.3 Tissue parameters
The choice of the tissue acoustic attenuation and absorption coefficients are critical to
accurate modelling of the expected tissue temperature rise. The amount of heat deposited is
proportional to the product of the local time-average intensity and the absorption coefficient,
and the local intensity decreases exponentially with the product of the attenuation coefficient
and the distance from the source transducer. As currently implemented, the algorithms for the
-1 -
TI assume homogeneous tissue with the slopes of both coefficients equal to 0,3 dB cm MHz
. Of course, real tissues are not homogeneous and usually have higher values for both their
acoustic attenuation and absorption coefficients [10]. This model, homogeneous tissue
model H.3, was chosen as a reasonable worst case with regard to patient safety because it
tends to overestimate temperature rise in most cases. However, by artificially limiting
transducer output, this combination of factors may reduce the clinical utility of diagnostic
ultrasound in many cases, particularly those involving hard-to-image patients.
4.2.4 Transducer self-heating
Because the transducer elements comprising an imaging probe are not 100% efficient at
converting electrical to acoustic energy, heat is produced within the transducer itself.
Whenever the energized probe is in contact with the patient, a portion of this heat will be
conducted into the adjacent tissues. As currently implemented, the TI considers only heating
produced by absorption of the acoustic beam, i.e., it does not include a correction for
transducer self-heating. This seems reasonable for transcutaneous applications because the
temperature rise due to surface heating will be small except within a depth of tissue on the
order of the perfusion length, 3 mm to 5 mm [2]. For some intra-cavity applications, and
especially in the presence of bone, however, the perfusion length may be significantly larger,
and transducer self-heating may heat deeper tissues [11] – [13]. At present, the problem is
dealt with by restricting the maximum measured surface temperature of the transducer to a
level considered safe for patient contact, 43 °C (IEC 60601-2-37).
4.2.5 Safety limits
As currently implemented, no limit is placed on the value of the TI that may be employed in
diagnostic imaging. This may be reasonable given the nature of the computational algorithms
and the fact that almost any reasonably attainable temperature elevation can be sustained
without harm if the duration is short enough, but it leaves the clinical user without guidance as
to what should be considered “reasonable”. The options suggested in 5.3 and 5.4
automatically incorporate a solution to this problem.
TR 62799 © IEC:2013(E) – 13 –
5 Options for improvement of the existing standard
5.1 General
Potential solutions to at least some of the limitations of the TI discussed above are available
in the literature. For example, the nonlinear relation between temperature elevation and
potential risk was pointed out in [14], which suggested replacing the current linear display with
an exponential display based on the form of the thermally equivalent time. The fact that the
risk of a thermally induced adverse effect depends on both the magnitude and duration of the
increase in temperature was considered in [15], which proposed an improvement to the TI, the
thermally equivalent time index (TETI), to account for both factors. The reliance of the TI on
equilibrium temperature rise has been investigated in greater detail [8]. It was proposed to
replace the current TI with a new parameter called the time to threshold (TT), which displays
the estimated duration of imaging required for the temperature rise to reach the threshold
temperature rise for an adverse biological effect. A similar approach was investigated in [16],
which proposed a different parameter, the safe use time (SUT), to compare a simplified
estimate of the thermally equivalent time to a threshold for an adverse effect in terms of
thermally equivalent time rather than temperature rise. These four options are discussed
first, followed by a fifth that has not yet been published.
A note on nomenclature: In this document, the widely accepted term “thermal dose” is
replaced by the more descriptive term “thermally equivalent time”, except when referring to
the published literature. The definition of “thermally equivalent time” is also more precise in
that the reference temperature is fixed at 43 °C.
5.2 Exponential display of the current TI
5.2.1 Theory
It is well known that there is a relationship between an elevation above normal physiological
temperature and the time needed to induce a deleterious effect in a biological system [2], [3],
[17], [18]. Simply put, the higher the temperature rise, the shorter the time needed to produce
the effect. For any two exposures at two different temperatures, the ratio of the minimum time
t required for the lower temperature T to produce an effect, to the time t required for the
1 1 2
higher temperature T to produce the same effect increased by a constant multiple for each
degree of temperature difference [19], [20]. For example, if the temperature difference T –
T = 1 °C, then t /t = R, while if T – T = 2 °C, then t /t = R , etc., where R is the thermal
1 1 2 2 1 1 2
(T −T ) 1°C
2 1
normalization constant. In general, t t = R , and the time calculated using this
1 2
approach to quantify thermal exposures is termed the thermally equivalent time. Empirical
values of R vary among species, tissues and biological endpoints. They are also temperature-
dependent, with R ≈ 2 for T > 43 °C, increasing by a factor of 2 to 3 for T < 43 °C. For
simplicity, the values for R are usually fixed at R = 2 for T > 43 °C and R = 4 for T < 43 °C [20],
[21].
The equation for thermally equivalent time is based on a thermodynamic or “Arrhenius-type”
analysis that has been empirically validated for a number of biological endpoints [20], [22].
The underlying principle is that the thermal damage to a biological system, Ω, which occurs
regardless of the temperature of the system, may be modelled as a first-order chemical rate
equation. From the Eyring equation for reaction rates in condensed or mixed-phase materials
[23], [24], it is possible to show that [25]:
dΩ − E
a
= k = Aexp (1)
dt R T (t)
g
where A is an arbitrary constant proportional to the change in entropy, E is the activation
a
energy for the damage process, R is the gas constant, and T is the absolute temperature
g
(i.e., temperature in units of kelvin) at time t. Equation (1) assumes that the rate, k, at which
– 14 – TR 62799 © IEC:2013(E)
damage is produced in a biological system can be characterized by a single activation energy,
although this may be an oversimplification. It is further assumed that when the probability of
occurrence of an adverse event, i.e., the incidence rate, IR, for the event is small, IR is
proportional to the amount of damage that accumulates over the duration of heating t . Thus:
h
t
h
− E
a
IR = C exp dt (2)
∫
R T (t)
g
-1
where C is a constant with units of t and t is the duration of heating.
h
For a temperature rise ∆T(t) above the normal physiologic temperature T , the incidence rate
o
for an adverse event relative to the background rate for the same event IR , is given by:
b
t
h
E
a
exp dt
∫
t
h
R [T + ∆T (t)]
E ∆T (t)
IR g o 1
1 a
= = exp dt . (3)
∫
t
h
IR t R T [T + ∆T (t)]
b − E h g o o
a
exp dt
∫
R T
g o
The relative increase in the incidence rate above the normal background rate, ∆IR , due to the
temperature rise ∆T, is given by:
t
h
∆IR IR IR 1 E ∆T (t)
1 1 b a
= − = exp dt −1 . (4)
∫
IR IR IR t R T [T + ∆T (t)]
b b b h g o o
For two different temperature rises, ∆T and ∆T , both functions of time, there will be two
1 2
different increases. Since ∆T (t) [1+ ∆T (t) T ] ≈ ∆T (t), the ratio of the corresponding increases
o
in rates ∆IR and ∆IR , is:
1 2
∆T
t C
h T t
∆T
h
E C
a T 1
C
T
exp dt −1
R dt −1
∫
2
∫
t
h R T t
g o h
∆IR
0
2 0
≈ = , (5)
∆T t
∆T
1 h
∆IR 1
t C C
h T T
R dt −1
1 E C
a T ∫
exp dt −1 t
h
∫
2 0
t
R T
h
g o
where the constant C = 1 °C and the thermal normalization constant . If
R = exp[E C (R T )]
T a T g o
∆T and ∆T are constant and we let ∆T = n∆T , then:
1 2 2 1
n∆T
C
T
∆IR R −1
= . (6)
∆T
∆IR 1
C
T
R −1
Equation (6) provides a simple expression for the relative change in the rate of induction of an
effect due to a temperature rise ∆T different from an arbitrarily chosen increase ∆T .
2 1
TR 62799 © IEC:2013(E) – 15 –
5.2.2 Illustrative results for the new thermal index display
Notice that in the numerator of Equation (6), the exponent is a linear function of ∆T . As
currently defined, the TI is the ratio of the output power (or estimated intensity in situ) for a
particular machine setting to the power (or intensity) required to produce an estimated
temperature rise of 1 °C, i.e., TI is a linear function of the output power (or intensity). By
keeping the reference temperature rise as 1 °C, i.e., by setting ∆T = 1 °C, and using the
current definition of TI as the relative temperature rise, i.e., n = TI , a new definition for
cur cur
the thermal index is obtained:
TI
cur
∆IR R −1
TI = = . (7)
new
∆IR R −1
The new index TI gives the ratio A/B, where A is an estimate of the maximum rate at which
new
damage is produced by an application of diagnostic ultrasound and B is the estimated damage
rate produced by imposing a temperature rise of 1 °C. This modification provides an easily
understood display that more accu
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...