IEC TR 60825-8:1999
(Main)Safety of laser products - Part 8: Guidelines for the safe use of medical laser equipment
Safety of laser products - Part 8: Guidelines for the safe use of medical laser equipment
Serves as a guide intended to give information to the employer and the user on the safe use of lasers and laser equipment classified as class 3B or class 4, for diagnostic and therapeutic applications in healthcare facilities. Explains the control measures recommended for the safety of patients, staff, maintenance personnel, and others. Engineering controls which form part of the laser equipment or the installation are also briefly described to provide an understanding of the general principles of protection.
General Information
- Status
- Published
- Publication Date
- 24-Nov-1999
- Technical Committee
- TC 76 - Optical radiation safety and laser equipment
- Drafting Committee
- WG 4 - TC 76/WG 4
- Current Stage
- DELPUB - Deleted Publication
- Start Date
- 08-Dec-2006
- Completion Date
- 14-Feb-2026
Relations
- Effective Date
- 05-Sep-2023
Overview
IEC TR 60825-8:1999 - Safety of laser products, Part 8: Guidelines for the safe use of medical laser equipment is an informative IEC technical report that provides guidance to employers, healthcare users and equipment operators on safe use of medical lasers (principally class 3B and class 4) in diagnostic and therapeutic settings. It explains hazards (eye, skin, fire, plume), recommends control measures and describes engineering and administrative protections to safeguard patients, staff, maintenance personnel and visitors. This document is guidance (technical report), not a prescriptive international standard.
Key Topics
The report covers practical safety topics essential to medical laser programs:
- Hazard assessment: eye and skin hazards (visible/near-IR retinal risks), fire/burn, fumes/plumes and collateral hazards.
- Beam delivery systems: fibre optics, handpieces, micromanipulators and implications for NOHD/NOHA and beam control.
- Administrative controls: appointment and role of the Laser Safety Officer (LSO), medical supervision/ophthalmic surveillance, incident and accident reporting, maintenance and inspection procedures.
- Training: recommended training elements for laser users and operators (see Annex D).
- Laser environment and engineering controls: design and designation of a laser controlled area, window shielding, door interlocks, wall finishes, fire protection, remote interlocks and fume extraction systems.
- Definitions and exposure concepts: MPE (Maximum Permissible Exposure), optical density (OD), nominal ocular hazard distance/area (NOHD/NOHA).
- Practical tools: checklists for installation, inspection schedules and safety-issue summaries (Annexes A–F).
Applications
IEC TR 60825-8:1999 is intended for practical application in healthcare facilities where lasers are used:
- Developing or updating a medical laser safety program and policies.
- Performing hazard assessments and establishing laser controlled areas.
- Specifying engineering controls (interlocks, shielding) and environmental controls (fume extraction, fire safety).
- Designing training curricula and maintenance/inspection schedules.
- Preparing incident/accident reporting procedures and checklists for procurement or site installation.
Who should use this guidance
- Hospital risk managers and department heads
- Laser users and laser operators (surgeons, clinicians, technologists)
- Laser Safety Officers (LSO) and biomedical engineers
- Facilities planners, clinical engineers and maintenance personnel
- Regulators and safety committees establishing institutional laser safety programs
Related standards
Relevant complementary documents referenced include IEC 60825-1, IEC 60601-2-22, IEC 60601-1 (and collateral standards) and ISO/TR 11991. These should be consulted for equipment classification, performance requirements and specific medical-device safety requirements.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
IEC TR 60825-8:1999 is a technical report published by the International Electrotechnical Commission (IEC). Its full title is "Safety of laser products - Part 8: Guidelines for the safe use of medical laser equipment". This standard covers: Serves as a guide intended to give information to the employer and the user on the safe use of lasers and laser equipment classified as class 3B or class 4, for diagnostic and therapeutic applications in healthcare facilities. Explains the control measures recommended for the safety of patients, staff, maintenance personnel, and others. Engineering controls which form part of the laser equipment or the installation are also briefly described to provide an understanding of the general principles of protection.
Serves as a guide intended to give information to the employer and the user on the safe use of lasers and laser equipment classified as class 3B or class 4, for diagnostic and therapeutic applications in healthcare facilities. Explains the control measures recommended for the safety of patients, staff, maintenance personnel, and others. Engineering controls which form part of the laser equipment or the installation are also briefly described to provide an understanding of the general principles of protection.
IEC TR 60825-8:1999 is classified under the following ICS (International Classification for Standards) categories: 11.040.99 - Other medical equipment; 31.260 - Optoelectronics. Laser equipment. The ICS classification helps identify the subject area and facilitates finding related standards.
IEC TR 60825-8:1999 has the following relationships with other standards: It is inter standard links to IEC TR 60825-8:2006. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
IEC TR 60825-8:1999 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
TECHNICAL IEC
REPORT
TR 60825-8
First edition
1999-11
Safety of laser products –
Part 8:
Guidelines for the safe use
of medical laser equipment
Sécurité des appareils à laser –
Partie 8:
Lignes directrices pour la sécurité d'utilisation
des appareils à laser médicaux
Reference number
IEC/TR 60825-8:1999(E)
Numbering
As from 1 January 1997 all IEC publications are issued with a designation in the
60000 series.
Consolidated publications
Consolidated versions of some IEC publications including amendments are
available. For example, edition numbers 1.0, 1.1 and 1.2 refer, respectively, to the
base publication, the base publication incorporating amendment 1 and the base
publication incorporating amendments 1 and 2.
Validity of this publication
The technical content of IEC publications is kept under constant review by the IEC,
thus ensuring that the content reflects current technology.
Information relating to the date of the reconfirmation of the publication is available
in the IEC catalogue.
Information on the subjects under consideration and work in progress undertaken
by the technical committee which has prepared this publication, as well as the list
of publications issued, is to be found at the following IEC sources:
• IEC web site*
•
Catalogue of IEC publications
Published yearly with regular updates
(On-line catalogue)*
• IEC Bulletin
Available both at the IEC web site* and as a printed periodical
Terminology, graphical and letter symbols
For general terminology, readers are referred to IEC 60050: International
Electrotechnical Vocabulary (IEV).
For graphical symbols, and letter symbols and signs approved by the IEC for
general use, readers are referred to publications IEC 60027: Letter symbols to be
used in electrical technology, IEC 60417: Graphical symbols for use on equipment.
Index, survey and compilation of the single sheets and IEC 60617: Graphical symbols
for diagrams.
* See web site address on title page.
TECHNICAL IEC
REPORT
TR 60825-8
First edition
1999-11
Safety of laser products –
Part 8:
Guidelines for the safe use
of medical laser equipment
Sécurité des appareils à laser –
Partie 8:
Lignes directrices pour la sécurité d'utilisation
des appareils à laser médicaux
IEC 1999 Copyright - all rights reserved
No part of this publication may be reproduced or utilized in any form or by any means, electronic or
mechanical, including photocopying and microfilm, without permission in writing from the publisher.
International Electrotechnical Commission 3, rue de Varembé Geneva, Switzerland
Telefax: +41 22 919 0300 e-mail: inmail@iec.ch IEC web site http://www.iec.ch
Commission Electrotechnique Internationale
PRICE CODE
W
International Electrotechnical Commission
For price, see current catalogue
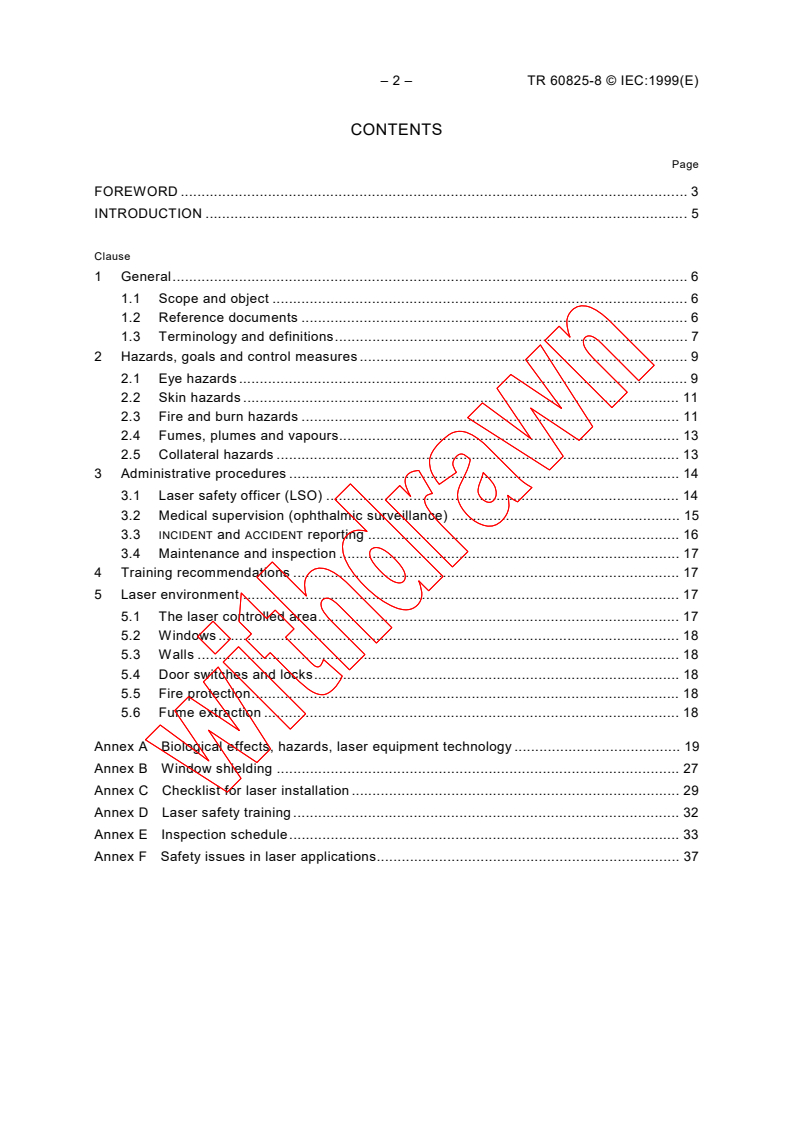
– 2 – TR 60825-8 © IEC:1999(E)
CONTENTS
Page
FOREWORD . 3
INTRODUCTION .5
Clause
1 General. 6
1.1 Scope and object . 6
1.2 Reference documents . 6
1.3 Terminology and definitions. 7
2 Hazards, goals and control measures . 9
2.1 Eye hazards . 9
2.2 Skin hazards . 11
2.3 Fire and burn hazards . 11
2.4 Fumes, plumes and vapours. 13
2.5 Collateral hazards . 13
3 Administrative procedures . 14
3.1 Laser safety officer (LSO) . 14
3.2 Medical supervision (ophthalmic surveillance) . 15
3.3 INCIDENT and ACCIDENT reporting . 16
3.4 Maintenance and inspection . 17
4 Training recommendations . 17
5 Laser environment . 17
5.1 The laser controlled area. 17
5.2 Windows . 18
5.3 Walls . 18
5.4 Door switches and locks. 18
5.5 Fire protection. 18
5.6 Fume extraction . 18
Annex A Biological effects, hazards, laser equipment technology . 19
Annex B Window shielding . 27
Annex C Checklist for laser installation . 29
Annex D Laser safety training . 32
Annex E Inspection schedule. 33
Annex F Safety issues in laser applications. 37
TR 60825-8 © IEC:1999(E) – 3 –
INTERNATIONAL ELECTROTECHNICAL COMMISSION
____________
SAFETY OF LASER PRODUCTS –
Part 8: Guidelines for the safe use of medical laser equipment
FOREWORD
1) The IEC (International Electrotechnical Commission) is a worldwide organization for standardization comprising
all national electrotechnical committees (IEC National Committees). The object of the IEC is to promote
international co-operation on all questions concerning standardization in the electrical and electronic fields. To
this end and in addition to other activities, the IEC publishes International Standards. Their preparation is
entrusted to technical committees; any IEC National Committee interested in the subject dealt with may
participate in this preparatory work. International, governmental and non-governmental organizations liaising
with the IEC also participate in this preparation. The IEC collaborates closely with the International Organization
for Standardization (ISO) in accordance with conditions determined by agreement between the two
organizations.
2) The formal decisions or agreements of the IEC on technical matters express, as nearly as possible, an
international consensus of opinion on the relevant subjects since each technical committee has representation
from all interested National Committees.
3) The documents produced have the form of recommendations for international use and are published in the form
of standards, technical specifications, technical reports or guides and they are accepted by the National
Committees in that sense.
4) In order to promote international unification, IEC National Committees undertake to apply IEC International
Standards transparently to the maximum extent possible in their national and regional standards. Any
divergence between the IEC Standard and the corresponding national or regional standard shall be clearly
indicated in the latter.
5) The IEC provides no marking procedure to indicate its approval and cannot be rendered responsible for any
equipment declared to be in conformity with one of its standards.
6) Attention is drawn to the possibility that some of the elements of this technical report may be the subject of
patent rights. The IEC shall not be held responsible for identifying any or all such patent rights.
The main task of IEC technical committees is to prepare International Standards. However, a
technical committee may propose the publication of a technical report when it has collected
data of a different kind from that which is normally published as an International Standard, for
example "state of the art".
Technical reports do not necessarily have to be reviewed until the data they provide are
considered to be no longer valid or useful by the maintenance team.
IEC 60825-8, which is a technical report, has been prepared by IEC technical committee 76:
Optical radiation safety and laser equipment.
The text of this technical report is based on the following documents:
Enquiry draft Report on voting
76/180/CDV 76/194/RVC
Full information on the voting for the approval of this technical report can be found in the report
on voting indicated in the above table.
This publication has been drafted in accordance with the ISO/IEC Directives, Part 3.
– 4 – TR 60825-8 © IEC:1999(E)
This document which is purely informative is not to be regarded as an International Standard.
Terms indicated in small capitals are defined in 1.3.
A bilingual version of this technical report may be issued at a later date.
TR 60825-8 © IEC:1999(E) – 5 –
INTRODUCTION
Lasers emit visible and/or invisible optical radiation. In some cases, this radiation is a parallel
beam with almost no divergence. This means that the inherently high IRRADIANCE (power per
unit of area irradiated) of the laser may be maintained over considerable distances. Because of
this, the beam may be focused to a very small area, which may be hazardous to the eye.
Annex A includes descriptions of laser systems and some medical applications.
Lasers may present hazards to patients and staff. Serious risks of injury, in particular to the
eye, and/or undesired effects can result from lack of protective measures, the use of faulty
laser equipment, misdirected beams or inappropriate laser control settings.
This guide is intended to give direction as to how aspects of laser safety may be incorporated
into medical laser practice. Its publication as a technical report indicates that it is not intended
to take precedence over existing or proposed national guidance. However, where none exists,
this guide should prove helpful.
Although the LASER USER has direct responsibility for safety during treatment, the employer
bears the responsibility for the setting up of a framework for the safe use of the system. This
guide strongly advocates the appointment of a LASER SAFETY OFFICER to provide expert advice
to the employer and all personnel concerned with the laser operation. This guide emphasizes
the need for appropriate laser safety training for all staff involved in providing practical
guidance on installation and maintenance.
– 6 – TR 60825-8 © IEC:1999(E)
SAFETY OF LASER PRODUCTS –
Part 8: Guidelines for the safe use of medical laser equipment
1 General
1.1 Scope and object
This technical report serves as a guide intended to give information to the employer and the
USER on the safe use of lasers and laser equipment classified as class 3B or class 4, for
diagnostic and therapeutic applications in healthcare facilities. However, particular care should
be taken in the use of class 2 and class 3A lasers where the patient’s normal aversion
response is compromised or absent.
This report explains the control measures recommended for the safety of patients, staff,
maintenance personnel and others. Engineering controls which form part of the laser
equipment or the installation are also briefly described to provide an understanding of the
general principles of protection. However, detailed specifications of laser equipment and
installation controls are not included in this report, such requirements being separately
specified in other standards, e.g. see 1.2.
The subject areas covered in this guide include
– BEAM DELIVERY SYSTEMS;
– biological effects of laser radiation;
– reporting of ACCIDENTS and dangerous situations;
– checklists.
The object of this report is to enhance the protection of persons from laser radiation and other
associated hazards by providing guidance on how to establish safety procedures, precautions
and user control measures.
1.2 Reference documents
IEC 60601-1:1988, Medical electrical equipment – Part 1: General requirements for safety
Amendment 1 (1991)
Amendment 2 (1995)
IEC 60601-1-1:1992, Medical electrical equipment – Part 1: General requirements for safety –
1. Collateral standard: Safety requirements for medical electrical systems
IEC 60601-1-2:1993, Medical electrical equipment – Part 1: General requirements for safety –
2. Collateral standard: Electromagnetic compatibility – Requirements and tests
IEC 60601-2-22:1995, Medical electrical equipment – Part 2: Particular requirements for the
safety of diagnostic and therapeutic laser equipment
IEC 60825-1:1993, Safety of laser products – Part 1: Equipment classification, requirements
and user's guide
ISO/TR 11991:1995, Guidance on airway management during laser surgery of upper airway
TR 60825-8 © IEC:1999(E) – 7 –
1.3 Terminology and definitions
For the purpose of this technical report, the following definitions apply. Reference is also made,
as indicated, to IEC 60825-1 and IEC 60601-2-22.
1.3.1
accident
INCIDENT which results in an injury
1.3.2
beam delivery system
fibre optic, handpiece, micromanipulator, scanning device, etc.
See also 2.1.106 of IEC 60601-2-22.
1.3.3
healthcare facility
any hospital, outpatient treatment centre, clinic or the like, where a laser can be used for
in vivo diagnosis, or surgical or therapeutic purposes on humans
1.3.4
high efficiency particulate-free air filter (HEPA)
porous filter normally used for removing particulate matter from air streams
1.3.5
incident
potentially dangerous situation which could result in an injury to the patient and/or other
personnel
1.3.6
irradiance
radiant flux, in watts per unit irradiated area, W/m . See also 3.35 of IEC 60825-1.
1.3.7
laser controlled area
area where laser safety controls apply. See also 3.37 of IEC 60825-1.
1.3.8
laser operator
person who operates laser controls (e.g. parameter settings, actuation switch). The LASER
OPERATOR may also be the LASER USER.
1.3.9
laser user
person who controls the delivery of the laser radiation to the working area
1.3.10
laser safety officer (LSO)
person who has the authority to monitor and enforce the control of laser safety hazards, and to
effect knowledgeable evaluation and control of laser hazards. See also 3.43 of IEC 60825-1.
1.3.11
maximum permissible exposure (MPE)
that level of radiation to which, in normal circumstances, the skin or eye may be exposed
without suffering adverse effects. See also A.2 of IEC 60825-1.
– 8 – TR 60825-8 © IEC:1999(E)
1.3.12
nominal ocular hazard area (NOHA)
area around the laser beam inside which the IRRADIANCE or RADIANT EXPOSURE is expected to
exceed the MPE. See 3.55 of IEC 60825-1.
1.3.13
nominal ocular hazard distance (NOHD)
distance from the laser aperture below which the IRRADIANCE or RADIANT EXPOSURE is expected
to exceed the MPE. See 3.56 of IEC 60825-1.
1.3.14
operator
See LASER OPERATOR.
1.3.15
optical density (OD)
negative of the logarithm to base ten of the factor related to the material’s property to attenuate
light during transmission, e.g. when the transmission factor is 0,01, the OD is 2; when the
transmission factor is 0,00001, the OD is 5. See 3.78 of IEC 60825-1.
1.3.16
pulse duration
time increment measured between the half peak power points at the leading and trailing edges
of a pulse. See 3.60 of IEC 60825-1.
1.3.17
radiance
radiant flux emitted by a unit area and propagating in a unit solid angle, expressed in W/m sr.
See also 3.62 of IEC 60825-1.
1.3.18
radiant exposure
radiant energy per unit irradiated area, expressed in J/m . See 3.64 of IEC 60825-1.
1.3.19
radiant power (radiant flux)
power emitted, transferred or received in the form of radiation, expressed in watts. See 3.65 of
IEC 60825-1.
1.3.20
remote interlock connector
socket on the laser equipment, allowing for a remotely connected emergency laser switch to
make provisions to interrupt the laser’s emission with a door interlock or other external safety
interlock switches. See also 3.67 of IEC 60825-1.
1.3.21
responsible body
individual or group responsible for the use and maintenance of equipment, and for assuring
that LASER OPERATORS and LASER USERS are adequately trained
1.3.22
user
See LASER USER.
TR 60825-8 © IEC:1999(E) – 9 –
2 Hazards, goals and control measures
2.1 Eye hazards
The retina of the eye is particularly susceptible to injury from laser radiation at wavelengths in
the visible and near-infrared regions (wavelengths between 400 nm and 1 400 nm). This is
because these wavelengths are readily transmitted through the ocular media and focused onto
the retina. Due to the focusing action of the eye, the retina may be exposed to an IRRADIANCE
that is over 100 000 times the IRRADIANCE arriving at the cornea. Surgical lasers, e.g. Nd-YAG
or argon-ion lasers, thus present a potential threat to the eyesight by direct exposure to the
beam or by specular (mirror-like) reflections from flat surfaces. Furthermore, looking at diffuse
reflections from rough surfaces can be hazardous with surgical lasers at all wavelengths.
The heat generated in retinal tissues exposed to laser radiation can cause rapid and
irreversible damage. Injury is dependent on the total RADIANT POWER passing through the pupil,
the laser wavelength and its transmission through the ocular media, the duration of the
exposure and the size of the image formed. A precise injury threshold is therefore difficult to
define. It should be emphasized that, in contrast to other tissues where tiny lesions may not
cause significant loss of function, a retinal lesion can cause irreversible loss of central vision.
Wavelengths above 1 400 nm are absorbed in the anterior components of the eye (cornea and
aqueous humour). Beyond 1 900 nm, the cornea is considered the sole absorber. Heat
produced in the anterior part of the cornea from, for example, a surgical carbon dioxide (CO )
laser may be conducted to adjacent tissues causing thermal damage. A surgical CO laser may
continuously vaporize surface tissue; the cornea of the eye can easily be injured if accidentally
exposed to this laser beam.
Other parts of the eye can also sustain injury, depending on the wavelength of the laser
radiation. The ultraviolet (UV) spectrum is divided into three specific regions which are related
to different biological responses:
– UV-A (315 nm to 400 nm) is strongly absorbed by the lens of the adult eye. The harmful
effects of exposure may not become apparent for many years (small lens opacities can
form, which may become clinically significant);
– UV-B (280 nm to 315 nm) and UV-C (100 nm to 280 nm) are mainly absorbed by the cornea
and conjunctiva and this can lead to inflammation of the cornea (photokeratitis) and
conjunctivitis. Damage limited to the outer layer of the cornea may be temporary. Special
considerations should be given to those persons who may be at particular risk from UV
exposure, e.g. aphakes or photosensitized persons. Refer to annex A.
2.1.1 Goal
Any person who is present within the nominal ocular hazard area (NOHA) should be protected
against unintended laser exposure above the maximum permissible exposure (MPE) for the
cornea.
2.1.2 Control measures
2.1.2.1 Laser protective eyewear (goggles or glasses)
Unless there is no reasonably foreseeable risk (as assessed by the LSO) that personnel may
be exposed to laser radiation in excess of the MPE, eye protection specifically designed for the
wavelength(s) and output in use should be worn in addition to any other controls that may be in
place. “Personnel” includes the patient, LASER USER, LASER OPERATOR, anaesthetists, assisting
staff and spectators. It is one of the duties of the LSO to specify appropriate eyewear, resistant
to the power or energy levels of the treatment beam expected during reasonably foreseeable
hazard conditions. When the treatment region is close to the eye, the patient’s eye protection
should be selected carefully, since the aiming beam as well as the treatment beam IRRADIANCE
– 10 – TR 60825-8 © IEC:1999(E)
or RADIANT EXPOSURE may exceed the MPE. Additionally, the blink reflex may be altered due to
anaesthetic drugs.
Laser protective eyewear should be clearly marked with the wavelength(s) and corresponding
OPTICAL DENSITY. Additionally, it is recommended that an unambiguous and robust method of
marking the laser safety eyewear be employed to ensure that there is a clear link to the
particular laser for which it has been specified.
The extent of the NOHA will vary according to the type of laser used and the optical properties
of the applicators used. Placement of the laser equipment and the patient within the room can
do much to control the direction and reduce the risk of exposure to errant beams.
As an alternative to having many people in the NOHA, which would require many pairs of
goggles to be available, consideration should be given to installing a remote video monitor
outside the NOHA.
2.1.2.2 Eye protection with viewing optics
When using viewing optics, e.g. endoscopes, microscopes, colposcopes, laparoscopes, slit
lamps and other optical devices, the person(s) looking through the eyepiece(s) should be
protected with a suitable filter or a shutter fitted to reduce the risk from radiation reflected
through the vision channel. In case of monocular optics, consideration should be given to
protecting the unshielded eye.
The use of a video endoscope can overcome the problems of reflected radiation in the viewing
optics; however, it is still advisable for all persons present to wear eye protection when there is
a risk of fibre breakage, or accidental firing of the laser when the fibre is out of the endoscope.
A risk assessment should be undertaken by the LSO.
2.1.2.3 Windows
Persons behind windows can be adequately protected by means of an opaque material
temporarily attached or unfolded at the window inside the room. For carbon dioxide lasers or
other lasers which emit at wavelengths longer than approximately 4 000 nm, glass may provide
sufficient absorption. Windows and shields should provide sufficient protection against
IRRADIANCE for the exposure duration likely to be encountered in normal use, as identified in
the risk assessment carried out by the LSO. For possible technical solutions, see annex B.
2.1.2.4 Reflecting surfaces
Reflections from shiny surfaces such as surgical instruments may focus the laser beam, which
can be hazardous, particularly to the eyes. Depending on the wavelength and beam
1)
configuration, diffuse reflections like that from the irradiated tissue from class 4 lasers may
also be hazardous.
a) Wall and ceiling surface or texture
The surface of the wall and ceiling should be chosen such that reflections are minimized.
The LSO should consider the risks due to possible reflections. A matt finish of any colour
will normally meet this requirement.
b) Room equipment
Glossy surfaces may be found with windows, cupboards, vent frames, fixation frames at
tables, infusion stands, sterilization cases, X-ray viewing screens, video monitors, operating
room lights, etc. Shiny surfaces may reflect laser radiation in an unpredictable way. The
LSO should identify the hazards involved and decide on the appropriate measures to be
taken. The checklist as described in annex C may be used.
––––––––––
1)
Class 3B laser diffuse reflections are not normally considered hazardous.
TR 60825-8 © IEC:1999(E) – 11 –
c) Instrumentation
Care should be taken to prevent the unintentional reflection of the laser beam from an
instrument. If the laser beam is likely to hit an instrument, any such instruments which may
be used with a laser should either be
– convex with small radii, if polished, or
– roughened, or
– anodized.
The USER should be aware that a surface which does not reflect visible light may reflect long-
wavelength infra-red laser radiation such as that from a CO laser. Black instruments may
absorb sufficient energy to become hot, causing unintended patient burns. These instruments
may also be significantly reflective at infra-red wavelengths. When working in the upper
USER
respiratory/digestive tract, the should consider that a reflected beam or a hot instrument
can perforate the endotracheal tube, possibly igniting it, with the risk of a severe endotracheal
fire, see also annex F.
Reflective surfaces are sometimes used to deflect the laser energy into an otherwise
inaccessible operating site. Mirrors or other reflective devices should be suitable for the laser
wavelengths and powers or energies employed.
NOTE Glass mirrors may shatter if used at high laser powers.
2.2 Skin hazards
ln general terms, the skin can tolerate a great deal more exposure to laser beam energy than
the eye. The biological effect of irradiation of the skin by lasers operating in the visible (400 nm
to 780 nm) and infra-red (780 nm to 1 mm) spectral regions may vary from a mild erythema to
severe blisters. See annex A.
2.2.1 Goal
Every person should be protected against unintended hazardous laser exposure.
2.2.2 Control measures (protective clothing)
The LSO should recommend or approve the use of appropriate clothing or covers, as
determined from the risk assessment, see annex C.
2.3 Fire and burn hazards
Lasers of class 4 may produce sufficient energy to ignite flammable materials particularly in
oxygen enriched atmospheres.
2.3.1 Goal
All personnel including the patient should be sufficiently protected against burns.
2.3.2 Methods of compliance
2.3.2.1 Endotracheal fires
When performing airway laser surgery in the presence of endotracheal tubes, the tube should
have adequate protection or be specially designed to reduce the likelihood of fire. For more
detailed information on this subject, reference is made to ISO/TR 11991. Fire hazards related
to endotracheal tubes, plastics, adhesive tapes, ointment and surgical preparatory solutions
can be controlled by various methods. These include (but are not confined to) the use of
non-combustible surgical instrumentation, Venturi (jet) ventilation techniques, shielding with
wet substances and the use of low-combustion gas mixtures. Anaesthetics personnel should
use non-flammable, specially manufactured or adequately protected laser resistant tubes.
– 12 – TR 60825-8 © IEC:1999(E)
Standard plastic and rubber tubes are particularly hazardous and should be avoided, unless
there is no practical alternative. There have been ACCIDENTS involving spirally wound metal
tapes and these should be avoided. If there is no medical contra-indication, the endotracheal
tube cuffs should be inflated with liquid and externally protected with wet swabs.
Since combustion may be initiated in the respiratory/digestive tract in high oxygen concen-
trations, or in the presence of oxidizing gases (nitrous oxide), the lowest possible concentration
of oxygen should be used in laryngo-tracheal procedures. In some cases where co-axial fibres
2)
are used, CO can be passed down the fibre at a low rate to minimize flammability at the
laser target site. Care should be taken to monitor p(O ).
2.3.2.2 Endogeneous combustion
In order to avoid combustion of endogeneous gases like methane in the gastro-intestinal tract,
localized ventilation techniques should be employed.
2.3.2.3 Endoscope burns
Care should be taken to avoid laser beam exposure of the sheaths of flexible fibre optic
endoscopes since most of the sheaths are flammable. For metallic tubular delivery systems
(i.e. bronchoscopes, laparoscopes, laryngoscopes), heating the wall should be avoided to
minimize the risk of thermal damage to adjoining tissue.
The USER should check the proper positioning of the laser delivery fibre (or waveguide) within
the endoscope prior to releasing the beam. Means include
– checking the integrity of the aiming spot;
– introducing the fibre far enough so that the tip can be seen through the endoscope. It
should be realized that the tip of the fibre may become excessively heated during laser
transmission and may cause heat damage to the endoscope or (upon contact) to the tissue
although the aiming spot looks normal.
Care should be taken when endoscopy is performed in an oxygen enriched atmosphere.
2.3.2.4 Cleaning, disinfecting and anaesthetic agents
Any new agent used with a laser should be checked for flammability before use. The USER
should consider the use of non-flammable agents (e.g. water-based). If the use of flammable
agents cannot be avoided, time should be allowed for complete dispersal of the agent to take
place.
2.3.2.5 Drapes and covers
Sponges, gauze pads and swabs located near the operating field should be moistened with
saline or sterile water. If class 4 laser equipment is used, surgical drapes may catch fire. The
region of the drape near the operating field should be kept moistened with saline or sterile
water.
If the laser handpiece is placed on a dry region of the sterile drape, the drape may be ignited if
the laser is accidentally operated, or if the handpiece is hot following use. This may go
unnoticed. It should, therefore, become a matter of routine either to cover the aperture with a
laser-resistant cap or to put the laser handpiece in a safe holder during a treatment pause
and/or to set the laser equipment to stand-by. The laser transmission system should never be
left lying on the patient or under uncontrolled conditions.
––––––––––
2)
The anaesthesiologist should be consulted. A typical rate is 250 cm per minute.
TR 60825-8 © IEC:1999(E) – 13 –
2.4 Fumes, plumes and vapours
In most class 4 laser operations, the vaporization of target tissue produces noxious airborne
contaminants. The smoke plume may contain viral particles having a respiratory size of the
order of 0,1 μm.
2.4.1 Goal
Laser generated fumes, plumes and vapours should be removed from the operating environ-
ment to produce a level which is considered acceptable.
2.4.2 Control measures
2.4.2.1 Dedicated smoke evacuation systems
Masks, including special laser surgical masks, are not recommended for use as the primary
method of filtration.
Airborne contaminants should be captured as near as practicable to the source and removed
by local exhaust ventilation. This should be designed to ensure that any potentially infectious
agents are not passed downstream in the air handling/exhaust system. This may be accom-
plished with a portable smoke extractor using charcoal or HEPA filters (at least 0,1 μm) with an
extraction efficiency at this particle size of more than 99 %. Local extraction of fume also
eliminates cellular debris and vapours, thus providing greater visibility for increased precision
and safety.
Replaceable filters should be monitored and replaced on a regular basis in accordance with the
manufacturer's recommendations.
2.4.2.2 High speed particles
Consideration should be given to protecting the eyes and the respiratory tract from particles
which may be ejected at high speed from the treatment site. Laser safety eyewear, if worn,
should provide adequate protection for the eyes.
2.4.2.3 Laser plume in the patient’s respiratory system
When jet ventilation is applied during laser treatment in the upper respiratory tract, the
ventilation flow may transport plume particles and gases into the patient’s respiratory system.
2.4.2.4 Surgical suction systems
If the amounts of fume are small, surgical suction may be used to clean the operating site.
2.4.2.5 Scavenging system for anaesthetic gases
The scavenging system for anaesthetic gases may also be used for the removal of fumes from
the use of laser systems. Disposable in-line filters may need to be included.
2.5 Collateral hazards
2.5.1 Noxious vapours
Presently, many hazardous gases such as chlorine, fluorine, hydrogen chloride and hydrogen
fluoride are used in some laser systems. Care should be taken with their storage and to ensure
adequate removal of noxious vapours in the event of failure. Dyes and associated solvents are
often toxic. The manufacturer's handling recommendations should be rigorously observed
when draining or filling dye lasers. Skin contact with the fluid used and inhalation of its vapour
should be avoided. Waste material should be disposed of in an approved manner.
– 14 – TR 60825-8 © IEC:1999(E)
2.5.2 Contaminants from gas containers used in endoscopy
Bacterial contaminants and metallic residues have been found in gas cylinders and pressure
regulators. Fibre delivery systems, as well as Venturi ventilation systems, that deliver gas from
gas containers to the lumen should therefore be equipped with an in-line filter to remove the
contaminants.
2.5.3 Collateral radiation
Many lasers employ high voltage, radio-frequency and intense optical sources for excitation.
These high-energy sources can be hazardous both to personnel and other equipment, if not
shielded. Under normal conditions, modern laser systems are safe. In order to ensure this, the
manufacturer's instructions should be followed by all staff using or maintaining the laser.
2.5.4 Gas embolism
The use of gases in laser surgery in closed body cavities can lead to a risk of gas embolism in
the patient. This risk can be minimized by using carbon dioxide, if a gas is required, or by using
a fluid. In particular, it is recommended that no gas be used in the uterus.
3 Administrative procedures
3.1 Laser safety officer (LSO)
For installations where lasers of class 3B or class 4 are in use, the RESPONSIBLE BODY should
appoint a LASER SAFETY OFFICER (LSO) and define his/her responsibilities. More than one LSO
may be appointed where multiple lasers are used. The LSO should be sufficiently
knowledgeable to be able to advise the RESPONSIBLE BODY of the healthcare facility on aspects
of laser safety which relate to the lasers in use in that facility. In small healthcare facilities, the
head or a member of the RESPONSIBLE BODY may assume the role of the LSO, provided the
appropriate knowledge is possessed. The LSO should cooperate directly with the USERS of the
equipment.
Locally, within the LASER CONTROLLED AREA, there should be a designated person, suitably
trained, who ensures that on a day-to-day basis safety measures are obeyed. The USER may
assume this role.
NOTE Medical laser equipment is frequently used in small clinics whose staff may consist of a single LASER USER
and a receptionist. This situation is found in the offices of physicians, podiatrists, dentists and others. The
requirements and principles of the safe use of such equipment in these settings are no less stringent than when the
same systems are used in large institutional settings such as hospitals. It is the responsibility of the healthcare
professional who is using the laser to be aware of the requirements for safe use. In effect, the individual
professional USER becomes responsible for consideration of the recommendations for safe use outlined in this
report. The professional should assume the administrative responsibilities of the LSO, as well as seeing that all
national regulations are met and non-governmental controls are in place. This means that he or she should be
trained in laser safety issues, and be responsible for, among others, the LASER CONTROLLED AREA and its warning
signs, proper use of protective eyewear and other safety measures both for protection of the patient and other
personnel who may be potentially exposed to hazards associated with laser use. The individual should also be
responsible for maintenance and other practices required for the safe operation of the healthcare laser equipment
he or she is using.
3.1.1 Duties and responsibilities of the LSO
3.1.1.1 Duties
The primary duty of the LSO should be to support and advise the RESPONSIBLE BODY with
respect to the safe use of lasers and protection measures.
TR 60825-8 © IEC:1999(E) – 15 –
3.1.1.2 Responsibilities
More specifically, the responsibilities of the LSO include:
a) performing a hazard assessment of laser treatment areas, including the determination of
the nominal hazard area; a scheme of a risk assessment should be followed (see annex C);
b) giving advice to the administrative head and to the responsible person in the area about
safety issues when purchasing and putting into operation the laser equipment as well as
operational and occupational safety measures;
c) choosing personal protective equipment;
d) contributing to the education of employees who work with or close to lasers about the
hazards and about the safety measures;
e) contributing to the checking and approval of laser equipment according to national
regulations and verifying that the maintenance and service of the equipment are performed
by persons who have been trained for that purpose or are otherwise qualified;
f) ensuring, by repeated auditing, that the prescribed control measures are effective, e.g.
checking that personal protective equipment, laser radiation barriers and laser signs are
in place, verifying standard operating procedures, alignment procedures, peri-operative
checklists;
g) providing information to the administrative head and to the responsible person in the area
about shortcomings and failures of the laser equipment;
h) investigating all ACCIDENTS and INCIDENTS involving lasers, providing information (see 3.3)
on preventive measures to those involved, including the dedicated safety specialists of the
facility.
Additional responsibilities may include
i) deciding about technical and organizational safety measures;
j) advising employees working with lasers or in laser areas;
k) withdrawing laser equipment from use, if necessary;
l) initiating medical investigations, if a laser ACCIDENT is reported;
m) liaising with national authorities.
3.2 Medical supervision (ophthalmic surveillance)
In the absence of national regulations, the following recommendations should be taken into
consideration:
a) the value of medical surveillance of laser workers is a fundamental problem as yet
unresolved by the medical profession. If ophthalmic examinations are undertaken, they
should be carried out by a qualified specialist and should be confined to workers using
class 3B and class 4 lasers;
b) a medical examination by a qualified specialist should be carried out immediately
(i.e. within 24 h) after an apparent or suspected injurious ocular exposure. Such an
examination should be supplemented with a full biophysical investigation of the circum-
stances under which the ACCIDENT occurred;
NOTE Specialists performing ophthalmic examinations should be aware that many retinal lesions can be
incorrectly attributed to laser damage (see Mainster MA, Sliney DH, Marshall J., Warren KA, Timberlake GT,
Trokel SL, But is it really light damage?, Ophthalmology, Vol. 104, Nr. 2, February 1997, Guest Editorial).
c) pre-, interim- and post-employment ophthalmic examinations of workers using class 3B and
class 4 lasers have value for medico-legal reasons only and are not a necessary part of a
safety programme.
– 16 – TR 60825-8 © IEC:1999(E)
3.3 INCIDENT and ACCIDENT reporting
3.3.1 INCIDENT reporting
Any INCIDENT or ACCIDENT arising from the use of the laser should be reported immediately to
the LSO. Further use of the laser should be suspended until the LSO has made an
investigation and taken steps to ensure that the INCIDENT or ACCIDENT cannot recur.
The LSO should carry out an investigation of any INCIDENT, develop recommendations to
prevent recurrence and supply a report to the RESPONSIBLE BODY. The latter, in consultation
with the LSO, is strongly advised to circulate the recommendations resulting from the
investigation at least to
– all other LSOs of the healthcare facility;
– the biomedical engineering department, as appropriate.
USERS
The LSOs are advised to inform the and employees concerned, as appropriate. The
LSOs are also advised to keep records of all such INCIDENTS.
NOTE It is understood that any INCIDENT needs an action. Actions include the development of preventive
strategies (recommendations) and the distribution of information about the INCIDENT along with preventive
recommendations to all persons who are likely to be subjected to the same kind of danger. It is therefore mandatory
that INCIDENTs which have happened are not allowed to be kept secret; in order to motivate people to freely report
the situation, they should not be subjected to sanctions. INCIDENT reporting will more and more become part of
modern management techniques, e.g. in terms of quality assurance and ACCIDENT prevention. It appears that,
besides the United States FDA activity about collecting and reporting of laser INCIDENTS, very little is known about
the severeness and statistics of laser INCIDENTS and ACCIDENTS. Some case reports are rumoured, most of them
‘mouth to mouth’, but solid facts are rare. However, knowledge of INCIDENTS and ACCIDENTS is the best basis for
adequately aimed counter-measures. Therefore, a legalized standardized reporting system would seem worthwhile.
Any INCIDENT, whether an injury occurs or not, provides valuable information from which lessons can be learnt. This
is an important part of safety management. The value of exchanging information between healthcare facilities is
emphasized.
3.3.2 ACCIDENT reporting
ACCIDENTS involving lasers and serious defects in the equipment which could have lead to
severe injuries should be reported to the central health authority if a country-wide reporting
system is in operation.
3.3.2.1 National ACCIDENT reporting procedure
Not defined in this report.
3.3.3 Reporting scheme
Where an INCIDENT or ACCIDENT involving a laser is suspected, the LSO should prepare a report
of the circumstances. The report should contain at least the following:
a) a summary of the circumstances of the INCIDENT that led to an injury, which should specify
1) the date, location and time of the INCIDENT,
2) the names and designations of all staff and other persons involved,
3) the details of the experience of the injured person,
4) apparent contributing factors to the INCIDENT,
5) the LSO’s recommendations to prevent a recurrence, and
6) the obvious or suspected nature of any injury sustained by the person;
b) full written statements from all persons (incl
...
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...