EN 14180:2025
(Main)Sterilizers for medical purposes - Low temperature steam and formaldehyde sterilizers - Requirements and testing
Sterilizers for medical purposes - Low temperature steam and formaldehyde sterilizers - Requirements and testing
1.1 This document specifies requirements and tests for LTSF sterilizers, which use a mixture of low temperature steam and formaldehyde as sterilizing agent, and which are working below ambient pressure only.
These sterilizers are primarily used for the sterilization of heat labile medical devices in health care facilities.
1.2 This document specifies minimum requirements:
- for the performance and design of sterilizers intended to deliver an LTSF process capable of sterilizing medical devices;
- for the equipment and controls of these sterilizers which are needed for operation, control and monitoring of the sterilization processes, and which can be used for validation of the sterilization process.
1.3 This document specifies further test equipment and test procedures used to verify conformance of the equipment design and performance specified by this document.
1.4 This document does not specify requirements and tests for decontamination systems for use in rooms, enclosures, or environmental spaces.
Sterilisatoren für medizinische Zwecke - Niedertemperatur-Dampf-Formaldehyd-Sterilisatoren - Anforderungen und Prüfung
Dieses Dokument legt Anforderungen und Prüfverfahren für NTDF Sterilisatoren fest, in denen als Sterilisiermittel ein Gemisch von Niedertemperatur-Dampf und Formaldehyd angewendet wird und die nur unterhalb des Umgebungsdrucks arbeiten.
Diese Sterilisatoren werden in erster Linie in medizinischen Einrichtungen zur Sterilisation hitzeempfindlicher Medizinprodukte verwendet.
1.2 Dieses Dokument legt Mindestanforderungen zu folgenden Punkten fest:
für die Leistung und Konstruktion von Sterilisatoren, um ein NTDF Verfahren bereitzustellen, das in der Lage ist, Medizinprodukte zu sterilisieren;
an die Ausrüstung und Bedienelemente dieser Sterilisatoren, die für den Betrieb, die Steuerung und Überwachung der Sterilisationsverfahren erforderlich sind und welche bei der Validierung der Sterilisationsverfahren angewendet werden können.
1.3 Dieses Dokument legt weitere Prüfgeräte und Prüfverfahren fest, um die Konformität der Ausrüstungs¬konstruktion und der nach diesem Dokument festgelegten Leistung zu verifizieren.
1.4 Dieses Dokument legt keine Anforderungen an und Prüfungen für Dekontaminationssysteme zur Verwendung in Räumen, umschlossenen Räumen oder umgebenden Räumen fest.
Stérilisateurs à usage médical - Stérilisateurs à la vapeur et au formaldéhyde à basse température - Exigences et essais
1.1 Le présent document spécifie les exigences et les essais relatifs aux stérilisateurs à la vapeur et au formaldéhyde à basse température, utilisant comme agent stérilisant un mélange à basse température de vapeur d’eau et de formaldéhyde et fonctionnant uniquement à une pression inférieure à la pression atmosphérique.
Ces stérilisateurs sont utilisés en priorité pour stériliser les dispositifs médicaux thermolabiles dans les centres de soins.
1.2 Le présent document spécifie les exigences minimales :
- de performances et de conception des stérilisateurs destinés à fournir un procédé LTSF capable de stériliser des dispositifs médicaux ;
- pour les équipements et commandes de ces stérilisateurs nécessaires au fonctionnement, au pilotage et à la surveillance des procédés de stérilisation et qui peuvent être utilisés pour la validation du procédé de stérilisation.
1.3 Le présent document spécifie l’appareillage d’essai et des modes opératoires d’essai supplémentaires utilisés pour vérifier la conformité de la conception et des performances de l’équipement spécifiées par le présent document.
1.4 Le présent document ne spécifie par d’exigences ni d’essais concernant les systèmes de décontamination destinés à être utilisés dans des salles, des enceintes ou des espaces environnementaux.
Sterilizatorji za uporabo v medicini - Sterilizatorji s paro z nizko temperaturo in s formaldehidom - Zahteve in preskušanje
1.1 Ta dokument določa zahteve in preskuse za sterilizatorje s paro z nizko temperaturo in s formaldehidom (LTSF) kot sterilizacijskim sredstvom, ki delujejo samo pri nizkem zračnem tlaku. Ti sterilizatorji se uporabljajo predvsem v zdravstvenih ustanovah za sterilizacijo medicinskih pripomočkov, občutljivih na vročino. 1.2 Ta dokument določa minimalne zahteve: – za delovanje in načrtovanje sterilizatorjev, namenjenih izvajanju postopka s paro z nizko temperaturo in s formaldehidom, ki omogoča sterilizacijo medicinskih pripomočkov; – za opremo in kontrolnike teh sterilizatorjev, ki so potrebni za delovanje, nadzor in spremljanje sterilizacijskih postopkov ter jih je mogoče uporabiti tudi za njihovo potrjevanje. 1.3 Ta dokument določa opremo za nadaljnje preskušanje in preskusne postopke, ki se uporabljajo za preverjanje skladnosti zasnove in delovanja opreme, določene v tem dokumentu. 1.4 Ta dokument ne določa zahtev in preskusov za sisteme za dekontaminacijo v zaprtih, ograjenih ali okoljskih prostorih.
General Information
- Status
- Published
- Publication Date
- 01-Apr-2025
- Technical Committee
- CEN/TC 102 - Sterilizers for medical purposes
- Drafting Committee
- CEN/TC 102/WG 6 - Gas sterilizers
- Current Stage
- 6060 - Definitive text made available (DAV) - Publishing
- Start Date
- 02-Apr-2025
- Due Date
- 29-May-2024
- Completion Date
- 02-Apr-2025
Relations
- Effective Date
- 19-Jan-2023
- Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Refers
EN IEC 60751:2022 - Industrial platinum resistance thermometers and platinum temperature sensors - Effective Date
- 09-Feb-2026
- Refers
EN 62366-1:2015 - Medical devices - Part 1: Application of usability engineering to medical devices - Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
Overview - EN 14180:2025 (CEN)
EN 14180:2025 is the European standard from CEN that specifies requirements and tests for low temperature steam and formaldehyde (LTSF) sterilizers used in healthcare. It replaces EN 14180:2014 and covers sterilizers that operate below ambient pressure only, primarily intended for sterilizing heat‑labile medical devices. The standard defines minimum design, performance, control, monitoring and validation requirements, plus test methods and procedures to verify conformity.
Key topics and technical requirements
- Scope and definitions: Clarifies LTSF sterilizer types, terms and limits (below ambient pressure; exclusion of room or environmental decontamination systems).
- Equipment design and construction: Material, chamber design, doors/interlocks, insulation, pipework, vaporizers, evacuation and aeration systems, vibration, transport and user interfaces.
- Safety, risk control and usability: Protective measures, interlocks and safety requirements for device and operator protection.
- Instrumentation, control and recording: Automatic controllers, monitoring of temperature, pressure, time and sterilant dose, status indicators, alarms, analogue/digital recording and data formats for sterilant application.
- Performance assessment and testing: Test instrumentation, physical condition attainment, sterilant control, microbicidal performance, desorption efficacy, load dryness and pressure change tests.
- Services & environment: Requirements for electrical, water, steam, vacuum, drainage, ventilation, emissions (electromagnetic, noise, exhaust and heat).
- Information and documentation: Information to be supplied before purchase and installation, marking, labelling and comprehensive instructions for use.
- Normative test methods: Annexes include test loads, test procedures and sterilizer testing protocols to verify conformity.
Practical applications - who uses EN 14180:2025
- Manufacturers and designers of LTSF sterilizers for product design, CE marking and conformity testing.
- Validation and quality engineers in healthcare and medical device sterilization departments for process validation and routine performance checks.
- Hospital procurement and biomedical engineering teams for specifying equipment, ensuring compliance and safe installation.
- Test laboratories and notified bodies performing type testing, conformity assessment and performance verification.
- Regulatory and compliance staff ensuring devices meet European requirements for medical sterilization equipment.
Related standards and context
EN 14180:2025 is part of the broader set of sterilization and medical device equipment standards. It complements other European and international standards that address steam sterilization, low‑temperature sterilization technologies, validation practices and laboratory testing, and is used together with applicable national regulations when selecting or validating sterilization equipment.
Keywords: EN 14180:2025, LTSF sterilizers, low temperature steam and formaldehyde, sterilizer requirements, sterilization testing, medical device sterilization, CEN standard, sterilizer validation.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
EN 14180:2025 is a standard published by the European Committee for Standardization (CEN). Its full title is "Sterilizers for medical purposes - Low temperature steam and formaldehyde sterilizers - Requirements and testing". This standard covers: 1.1 This document specifies requirements and tests for LTSF sterilizers, which use a mixture of low temperature steam and formaldehyde as sterilizing agent, and which are working below ambient pressure only. These sterilizers are primarily used for the sterilization of heat labile medical devices in health care facilities. 1.2 This document specifies minimum requirements: - for the performance and design of sterilizers intended to deliver an LTSF process capable of sterilizing medical devices; - for the equipment and controls of these sterilizers which are needed for operation, control and monitoring of the sterilization processes, and which can be used for validation of the sterilization process. 1.3 This document specifies further test equipment and test procedures used to verify conformance of the equipment design and performance specified by this document. 1.4 This document does not specify requirements and tests for decontamination systems for use in rooms, enclosures, or environmental spaces.
1.1 This document specifies requirements and tests for LTSF sterilizers, which use a mixture of low temperature steam and formaldehyde as sterilizing agent, and which are working below ambient pressure only. These sterilizers are primarily used for the sterilization of heat labile medical devices in health care facilities. 1.2 This document specifies minimum requirements: - for the performance and design of sterilizers intended to deliver an LTSF process capable of sterilizing medical devices; - for the equipment and controls of these sterilizers which are needed for operation, control and monitoring of the sterilization processes, and which can be used for validation of the sterilization process. 1.3 This document specifies further test equipment and test procedures used to verify conformance of the equipment design and performance specified by this document. 1.4 This document does not specify requirements and tests for decontamination systems for use in rooms, enclosures, or environmental spaces.
EN 14180:2025 is classified under the following ICS (International Classification for Standards) categories: 11.080.10 - Sterilizing equipment. The ICS classification helps identify the subject area and facilitates finding related standards.
EN 14180:2025 has the following relationships with other standards: It is inter standard links to EN 14180:2014, EN IEC 61326-1:2021, EN 60584-1:2013, ISO 8573-1:2010, EN IEC 60751:2022, EN 62366-1:2015, EN 61010-1:2010/A1:2019, EN IEC 61010-2-040:2021, EN 62366-1:2015/A1:2020, EN 61010-1:2010, EN ISO 11607-1:2020, EN 13445-1:2021, EN ISO 11138-5:2017, EN ISO 20417:2021, EN ISO 11607-1:2020/A11:2022. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
EN 14180:2025 is associated with the following European legislation: EU Directives/Regulations: 2017/745; Standardization Mandates: M/575, M/575 AMD 1, M/575 AMD 2. When a standard is cited in the Official Journal of the European Union, products manufactured in conformity with it benefit from a presumption of conformity with the essential requirements of the corresponding EU directive or regulation.
EN 14180:2025 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-junij-2025
Nadomešča:
SIST EN 14180:2014
Sterilizatorji za uporabo v medicini - Sterilizatorji s paro z nizko temperaturo in s
formaldehidom - Zahteve in preskušanje
Sterilizers for medical purposes - Low temperature steam and formaldehyde sterilizers -
Requirements and testing
Sterilisatoren für medizinische Zwecke - Niedertemperatur-Dampf-Formaldehyd-
Sterilisatoren - Anforderungen und Prüfung
Stérilisateurs à usage médical - Stérilisateurs à la vapeur et au formaldéhyde à basse
température - Exigences et essais
Ta slovenski standard je istoveten z: EN 14180:2025
ICS:
11.080.10 Sterilizacijska oprema Sterilizing equipment
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
EN 14180
EUROPEAN STANDARD
NORME EUROPÉENNE
April 2025
EUROPÄISCHE NORM
ICS 11.080.10 Supersedes EN 14180:2014
English Version
Sterilizers for medical purposes - Low temperature steam
and formaldehyde sterilizers - Requirements and testing
Stérilisateurs à usage médical - Stérilisateurs à la Sterilisatoren für medizinische Zwecke -
vapeur et au formaldéhyde à basse température - Niedertemperatur-Dampf-Formaldehyd-Sterilisatoren
Exigences et essais - Anforderungen und Prüfung
This European Standard was approved by CEN on 24 February 2025.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this
European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references
concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN
member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by
translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management
Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Türkiye and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2025 CEN All rights of exploitation in any form and by any means reserved Ref. No. EN 14180:2025 E
worldwide for CEN national Members.
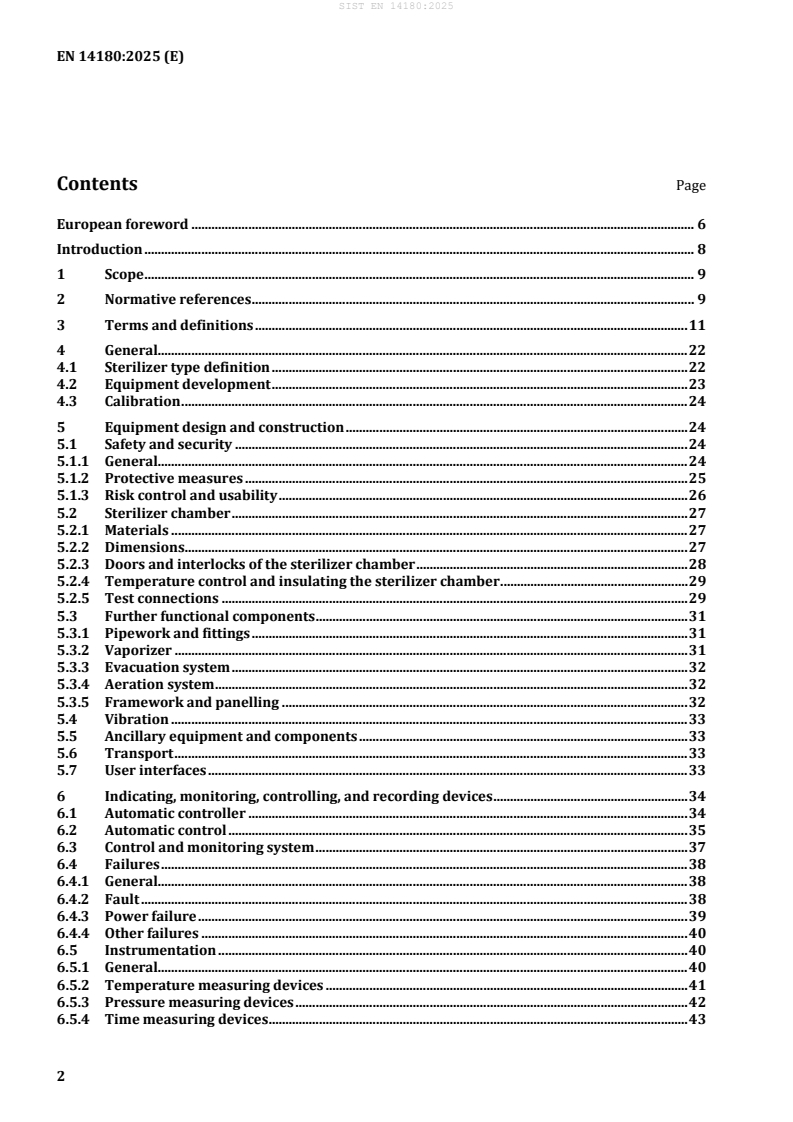
Contents Page
European foreword . 6
Introduction . 8
1 Scope . 9
2 Normative references . 9
3 Terms and definitions . 11
4 General. 22
4.1 Sterilizer type definition . 22
4.2 Equipment development . 23
4.3 Calibration . 24
5 Equipment design and construction . 24
5.1 Safety and security . 24
5.1.1 General. 24
5.1.2 Protective measures . 25
5.1.3 Risk control and usability . 26
5.2 Sterilizer chamber . 27
5.2.1 Materials . 27
5.2.2 Dimensions. 27
5.2.3 Doors and interlocks of the sterilizer chamber . 28
5.2.4 Temperature control and insulating the sterilizer chamber . 29
5.2.5 Test connections . 29
5.3 Further functional components . 31
5.3.1 Pipework and fittings . 31
5.3.2 Vaporizer . 31
5.3.3 Evacuation system . 32
5.3.4 Aeration system . 32
5.3.5 Framework and panelling . 32
5.4 Vibration . 33
5.5 Ancillary equipment and components . 33
5.6 Transport . 33
5.7 User interfaces . 33
6 Indicating, monitoring, controlling, and recording devices . 34
6.1 Automatic controller . 34
6.2 Automatic control . 35
6.3 Control and monitoring system . 37
6.4 Failures . 38
6.4.1 General. 38
6.4.2 Fault . 38
6.4.3 Power failure . 39
6.4.4 Other failures . 40
6.5 Instrumentation . 40
6.5.1 General. 40
6.5.2 Temperature measuring devices . 41
6.5.3 Pressure measuring devices . 42
6.5.4 Time measuring devices . 43
6.5.5 Sterilizing agent control and measuring devices . 43
6.6 Indicating devices . 44
6.6.1 General . 44
6.6.2 Cycle parameter indicating devices . 44
6.6.3 Cycle parameter indications . 46
6.6.4 Status indicators and indications . 47
6.6.5 Operating cycle counter . 48
6.7 Recording systems . 48
6.7.1 General . 48
6.7.2 Records . 49
6.7.3 Analogue presentation of records . 50
6.7.4 Digital records . 50
6.7.5 Data format for applied sterilant amount . 51
6.8 Operating cycle . 51
6.8.1 General . 51
6.8.2 Leak test . 51
6.8.3 Sterilization cycles . 52
7 Services and local environment . 54
7.1 General . 54
7.2 Sterilizing agent and sterilant . 55
7.3 Electrical supply . 56
7.4 Water . 56
7.4.1 Water used for sterilizer operation . 56
7.4.2 Feed water . 56
7.5 Steam . 56
7.6 Vacuum . 56
7.7 Drainage and discharges . 56
7.8 Lighting . 57
7.9 Compressed air . 57
7.10 Air and inert gases. 57
7.11 Ventilation and environment . 57
8 Emissions . 58
8.1 Electromagnetic emissions . 58
8.2 Noise . 58
8.3 Exhaust emissions . 59
8.4 Heat emissions . 59
9 Test instrumentation . 59
10 Performance assessment . 59
10.1 General . 59
10.2 Attainment of conditions . 60
10.2.1 Physical conditions . 60
10.2.2 Sterilant and sterilizing agent . 62
10.2.3 Microbicidal performance . 62
10.3 Desorption efficacy . 62
10.4 Load dryness . 62
10.5 Pressure change . 62
11 Information to be supplied . 63
11.1 General . 63
11.2 Information to be available prior to purchase . 63
11.3 Information prior to installation . 64
11.4 Marking and labelling . 65
11.5 Instructions for use . 66
11.6 Further information to be provided . 67
12 Packaging . 68
Annex A (normative) Test methods. 69
A.1 General. 69
A.2 Test loads . 69
A.3 Test procedures . 71
Annex B (normative) Sterilizer testing . 78
B.1 General. 78
B.2 Type test . 78
B.3 Works test . 79
B.4 Installation qualification test provisions . 79
B.5 Operational qualification test provisions . 80
Annex C (normative) Test equipment . 81
C.1 Pressure instrumentation . 81
C.2 Temperature sensors . 81
C.3 Temperature recording instrument . 81
C.4 Pressure recording instrument . 82
C.5 Penetration type test device (PTTD) . 83
C.6 Residues challenge device . 83
C.7 Biological indicators and systems . 84
C.8 Sterile barrier systems . 84
Annex D (normative) Determination of formaldehyde residuals in a filter indicator . 85
D.1 Procedure for sample preparation . 85
D.2 Analysis of formaldehyde contents in filter indicator . 85
Annex E (informative) Application of Formaldehyde in LTSF-processes . 88
E.1 Formaldehyde concentrations, physico-chemical conditions during a cycle . 88
E.2 Formaldehyde residuals on medical devices . 90
Annex F (informative) Illustrations of the interrelationship between control and recording. 93
F.1 Introduction . 93
F.2 Illustration 1 . 95
F.3 Illustration 2 . 96
F.4 Illustration 3 . 97
Annex G (informative) Additional information on protective measures . 100
Annex H (informative) Environmental aspects . 101
H.1 Environmental aspects regarding the life cycle of LTSF sterilizers . 101
H.2 Formaldehyde (brief description) . 101
H.3 Environmental impact . 101
Annex ZA (informative) Relationship between this European Standard and the General Safety and
Performance Requirements of Regulation (EU) 2017/745 aimed to be covered . 103
Bibliography . 125
European foreword
This document (EN 14180:2025) has been prepared by Technical Committee CEN/TC 102 “Sterilizers
and associated equipment for processing of medical devices”, the secretariat of which is held by DIN.
This European Standard shall be given the status of a national standard, either by publication of an
identical text or by endorsement, at the latest by October 2025, and conflicting national standards shall
be withdrawn at the latest by October 2025.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
This document supersedes EN 14180:2014.
This document has been prepared under a standardization request addressed to CEN by the European
Commission. The Standing Committee of the EFTA States subsequently approves these requests for its
Member States.
For the relationship with EU Legislation, see informative Annex ZA, which is an integral part of this
document.
In comparison with the previous edition, the following technical modifications have been made:
— structure of the main text has been adapted to the structure of ISO/TS 22421:2021 and harmonized
with the current revisions of EN 17180 and EN 1422 in 2024;
— references have been updated, including Table H.1 on Environmental Aspects, and the bibliography;
— some definitions of terms have been added, most definitions have been adapted with reference to
EN ISO 11139:2018;
— a separate clause ‘Protective measures’ has been implemented for referencing to individual clauses
of EN IEC 61010-2-040:2021;
— a new Annex G ‘Additional information on protective measures’ has been added;
— requirements on the control and monitoring system have been merged into a new clause and
informative illustrations including some explanations have been provided in a new Annex F;
— an informative new Annex E ‘Application of Formaldehyde in LTSF-processes’ has been added to
explain in some detail the physico-chemical specifics during operation of the sterilizer;
— the specifications provide as a new option a specific cycle for simple items and a ‘simple items test
load’ to allow (shorter) cycles for load configurations providing a lower challenge to the sterilization
process regarding sterilizing agent penetration, desorption and total mass of the load;
— new Annex ZA has been added to show the Relationship between this European Standard the General
Safety and Performance Requirements of Regulation (EU) 2017/745 aimed to be covered.
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN-CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria, Croatia,
Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland,
Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of North
Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Türkiye and the United
Kingdom.
Introduction
This document provides minimum requirements and test methods for sterilizers working below ambient
atmospheric pressure performing a low temperature steam and formaldehyde (LTSF) process.
LTSF sterilizers typically use a mixture of steam and formaldehyde at thermodynamic equilibrium
conditions. Sterilization occurs in the condensate layer at the surface of the items to be sterilized.
LTSF sterilizers are primarily used for the sterilization of medical devices in health care facilities but may
also be used during the commercial production of medical devices.
LTSF processes are specified by physical parameters and verified using physical, chemical, and
microbiological means [42]. The sterilizers operate automatically using pre-set cycles.
The test methods and test equipment given may also be applicable to validation and routine control.
Validation and routine control of sterilization processes are essential to ensure their efficacy. This
document does not cover validation and routine control of a LTSF process. Criteria for validation and
routine control of LTSF sterilization processes are given in EN ISO 25424.
At the present state of knowledge, LTSF sterilizers should not be assumed to deliver processes effectively
inactivating the causative agents of spongiform encephalopathies such as scrapie, Bovine Spongiform
Encephalopathy and Creutzfeldt-Jakob Disease. Specific recommendations have been produced in
particular countries for the processing of materials potentially contaminated with these agents. See also
EN ISO 25424:2019, 1.2.1.
Planning and design of products applying to this standard should consider not only technical issues but
also the environmental impact from the product during its life cycle. Environmental aspects are
addressed in Annex H of this document.
General safety requirements for sterilizers are specified by EN IEC 61010-2-040, amending or modifying
respective clauses in EN 61010-1 by references. Further, EN 60204-1 can provide valuable additional
options. They are referenced herein, but not repeated. Occupational safety is not addressed in this
standard.
1 Scope
1.1 This document specifies requirements and tests for LTSF sterilizers, which use a mixture of low
temperature steam and formaldehyde as sterilizing agent, and which are working below ambient
pressure only.
These sterilizers are primarily used for the sterilization of heat labile medical devices in health care
facilities.
1.2 This document specifies minimum requirements:
— for the performance and design of sterilizers intended to deliver an LTSF process capable of
sterilizing medical devices;
— for the equipment and controls of these sterilizers which are needed for operation, control and
monitoring of the sterilization processes, and which can be used for validation of the sterilization
process.
1.3 This document specifies further test equipment and test procedures used to verify conformance of
the equipment design and performance specified by this document.
1.4 This document does not specify requirements and tests for decontamination systems for use in
rooms, enclosures, or environmental spaces.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
EN 764-7:2002, Pressure equipment — Part 7: Safety systems for unfired pressure equipment
EN 13445-1:2021, Unfired pressure vessels — Part 1: General
EN 13445-2:2021+A1:2023, Unfired pressure vessels — Part 2: Materials
EN 13445-3:2021, Unfired pressure vessels — Part 3: Design
EN 13445-4:2021+A1:2023, Unfired pressure vessels — Part 4: Fabrication
EN 13445-5:2021+A1:2024, Unfired pressure vessels — Part 5: Inspection and testing
EN 13445-8:2021, Unfired pressure vessels — Part 8: Additional requirements for pressure vessels of
aluminium and aluminium alloys
EN 14222:2021, Stainless steel steam boilers
EN 60584-1:2013, Thermocouples — Part 1: EMF specifications and tolerances (IEC 60584-1:2013)
EN 61010-1:2010, Safety requirements for electrical equipment for measurement, control, and laboratory
use — Part 1: General requirements (IEC 61010-1:2010)
This document is impacted by corrigendum EN 764-7:2002/AC:2006.
This document is impacted by amendment EN 61010-1:2010/A1:2019 and corrigendum
EN 61010-1:2010/A1:2019/AC:2019.
EN 62366-1:2015, Medical devices — Part 1: Application of usability engineering to medical devices
EN IEC 60751:2022, Industrial platinum resistance thermometers and platinum temperature sensors
(IEC 60751:2022)
EN IEC 61010-2-040:2021, Safety requirements for electrical equipment for measurement, control, and
laboratory use — Part 2-040: Particular requirements for sterilizers and washer-disinfectors used to treat
medical materials (IEC 61010-2-040:2020)
EN IEC 61326-1:2021, Electrical equipment for measurement, control and laboratory use — EMC
requirements — Part 1: General requirements (IEC 61326-1:2020)
EN ISO 228-1:2003, Pipe threads where pressure-tight joints are not made on the threads — Part 1:
Dimensions, tolerances and designation (ISO 228-1:2000)
EN ISO 3746:2010, Acoustics — Determination of sound power levels and sound energy levels of noise
sources using sound pressure — Survey method using an enveloping measurement surface over a reflecting
plane (ISO 3746:2010)
EN ISO 11138-5:2017, Sterilization of health care products — Biological indicators — Part 5: Biological
indicators for low-temperature steam and formaldehyde sterilization processes (ISO 11138-5:2017)
EN ISO 11140-6:2022, Sterilization of health care products — Chemical indicators — Part 6: Type 2
indicators and process challenge devices for use in performance testing of small steam sterilizers
(ISO 11140-6:2022)
EN ISO 11607-1:2020, Packaging for terminally sterilized medical devices — Part 1: Requirements for
materials, sterile barrier systems and packaging systems (ISO 11607-1:2019)
EN ISO 11607-2:2020, Packaging for terminally sterilized medical devices — Part 2: Validation
requirements for forming, sealing and assembly processes (ISO 11607-2:2019)
EN ISO 14971:2019, Medical devices — Application of risk management to medical devices
(ISO 14971:2019)
EN ISO 15223-1:2021, Medical devices — Symbols to be used with information to be supplied by the
manufacturer — Part 1: General requirements (ISO 15223-1:2021)
EN ISO 20417:2021, Medical devices — Information to be supplied by the manufacturer (ISO 20417:2021,
Corrected version 2021-12)
EN ISO 25424:2019, Sterilization of health care products — Low temperature steam and formaldehyde —
Requirements for development, validation and routine control of a sterilization process for medical devices
(ISO 25424:2018)
ISO 8573-1:2010, Compressed air — Part 1: Contaminants and purity classes
This document is impacted by corrigenda EN 62366-1:2015/AC:2015 and EN 62366-1:2015/AC:2016-09 and
amendment EN 62366-1:2015/A1:2020.
This document is impacted by amendments EN 11607-1:2020/A11:2022 and EN 11607-1:2020/A1:2023.
This document is impacted by amendments EN 11607-2:2020/A11:2022 and EN 11607-2:2020/A1:2023.
This document is impacted by amendment EN 14971:2019/A11:2021.
This document is impacted by amendment EN ISO 25424:2019/A1:2022.
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https://www.iso.org/obp
— IEC Electropedia: available at https://www.electropedia.org/
3.1
access device
means by which entry to restricted parts of equipment is achieved
Note 1 to entry: This can be a dedicated key, code or tool.
[SOURCE: EN ISO 11139:2018, 3.4]
3.2
aeration
part of the sterilization cycle during which the sterilizing agent and/or its reaction products desorb from
the health care product until predetermined levels are reached
[SOURCE: EN ISO 11139:2018, 3.7]
3.3
automatic controller
device that directs the equipment sequentially through required stages of the cycle in response to
programmed cycle parameters
[SOURCE: EN ISO 11139:2018, 3.18]
3.4
biological indicator
test system containing viable microorganisms providing a specified resistance to a specified sterilization
process
[SOURCE: EN ISO 11139:2018, 3.29]
3.5
chamber
part of equipment in which load is processed
Note 1 to entry: In this document the chamber is the “sterilizer chamber”.
[SOURCE: EN ISO 11139:2018, 3.36, modified – Note 1 to entry added.]
3.6
chamber pre-heating
process that raises the temperature of internal chamber surfaces prior to the commencement of an
operating cycle
[SOURCE: EN ISO 11139:2018, 3.37]
3.7
chamber volume
enclosed space of a chamber, including the volume of nozzles to the first connection or weld, and
excluding the volume of permanent internal parts
[SOURCE: EN ISO 11139:2018, 3.318.1]
3.8
conditioning
treatment of product prior to the exposure phase to attain a specified temperature, relative humidity, or
other process variable throughout the load
[SOURCE: EN ISO 11139:2018, 3.58]
3.9
control
regulation of variables within specified limits
[SOURCE: EN ISO 11139:2018, 3.63]
3.10
cycle complete
message from the automatic controller that the operating cycle has ended successfully
[SOURCE: EN ISO 11139:2018, 3.71]
3.11
cycle parameter
value of a cycle variable including its tolerance used for control, monitoring, indication and recording of
an operating cycle
[SOURCE: EN ISO 11139:2018, 3.72]
3.12
cycle variable
property used to control, monitor, indicate, or record an operating cycle
[SOURCE: EN ISO 11139:2018, 3.74]
3.13
desorption
removal of the sterilizing agent from the chamber and the load at the end of the exposure phase
[SOURCE: EN ISO 11139:2018, 3.78]
3.14
development
act of elaborating a specification
[SOURCE: EN ISO 11139:2018, 3.79]
3.15
double-ended
having separate doors for loading and unloading in separate areas
[SOURCE: EN ISO 11139:2018, 3.92]
3.16
equilibration time
period between the attainment of defined sterilization process parameters at the reference measurement
point and the attainment of the specified sterilization process parameters at all points within the load
[SOURCE: EN ISO 11139:2018, 3.105]
3.17
establish
determine by theoretical evaluation and confirm by experimentation
[SOURCE: EN ISO 11139:2018, 3.107]
3.18
exposure stage
cycle stage between the introduction of the sterilizing agent or disinfecting agent into the chamber and
when its microbicidal effect has become negligible
Note 1 to entry: The exposure stage comprises that part of the process for which microbial lethality is claimed.
Note 2 to entry: This can be achieved, for example, by removal or neutralization.
[SOURCE: EN ISO 11139:2018/A1:2024, 3.111, modified – Note 2 to entry added.]
3.19
F value
BIO
expression of the resistance of a biological indicator calculated as the product of the logarithm of the
initial population of microorganisms and the D value
[SOURCE: EN ISO 11139:2018, 3.113.2]
3.20
fault
situation in which one or more of the process or cycle parameters is/are outside its/their specified
tolerance(s)
[SOURCE: EN ISO 11139:2018, 3.116]
3.21
filter
construct of porous material through which a fluid is passed to remove viable and/or non-viable particles
[SOURCE: EN ISO 11139:2018, 3.117]
3.22
hazard
potential source of harm
[SOURCE: EN ISO 11139:2018, 3.130]
3.23
hazardous situation
circumstance in which people, property, or the environment is/are exposed to one or more hazards
[SOURCE: EN ISO 11139:2018, 3.131]
3.24
holding time
period during which process parameters are maintained, within their specified tolerances
[SOURCE: EN ISO 11139:2018, 3.133]
3.25
indicate
display a value, condition, or stage of process
[SOURCE: EN ISO 11139:2018, 3.139]
3.26
inspection
determination of conformity to specified requirements
Note 1 to entry: If the result of an inspection shows conformity, it can be used for purposes of verification.
Note 2 to entry: The result of an inspection can show conformity or nonconformity or a degree of conformity.
Note 3 to entry: Inspection can be understood as visual inspection and/or application testing.
Note 4 to entry: References to definitions of determination, conformity and specified requirements are removed.
[SOURCE: EN ISO 9000:2015, 3.11.7, modified – Notes 3 and 4 to entry added]
3.27
installation qualification
IQ
process of establishing by objective evidence that all key aspects of the process equipment and ancillary
system installation comply with the approved specification
[SOURCE: EN ISO 11139:2018, 3.220.2]
3.28
load
product, equipment, or materials to be processed together within an operating cycle
[SOURCE: EN ISO 11139:2018, 3.155]
3.29
load configuration
distribution and orientation of a load
[SOURCE: EN ISO 11139:2018, 3.156]
3.30
loading door
means of access through which a load is passed into the chamber before processing
[SOURCE: EN ISO 11139:2018, 3.157]
3.31
measuring chain
series of elements of a measuring instrument or measuring system, which constitutes the path of the
measurement signal from the input (quantity subject to measurement) to the output (the result of the
measurement)
[SOURCE: EN ISO 11139:2018, 3.165]
3.32
medical device
instrument, apparatus, implement, machine, appliance, implant, reagent for in vitro use or software
material, or other similar related article, intended by the manufacturer to be used, alone or in
combination, for human beings, for one or more of the specific medical purpose(s) of:
— diagnosis, prevention, monitoring, treatment or alleviation of disease,
— diagnosis, monitoring, treatment, alleviation of or compensation for an injury,
— investigation, replacement, modification or support of the anatomy or of a physiological process,
— supporting or sustaining life,
— control of conception,
— disinfection of medical devices,
— providing information by means of in vitro examination of specimens derived from the human body,
and does not achieve its primary intended action by pharmacological, immunological or metabolic means
in or on the human body, but which may be assisted in its function by such means
Note 1 to entry: Products which may be considered to be medical devices in some jurisdictions, but not in others
include:
— items specifically intended for cleaning or sterilization of medical devices;
— pouches, reel goods, sterilization wrap, and reusable containers for packaging of medical devices for
sterilization;
— disinfection substances;
— aids for persons with disabilities;
— devices incorporating animal and/or human tissues;
— devices for in vitro fertilization or assisted reproduction technologies.
[SOURCE: EN ISO 11139:2018/A1:2024, 3.166]
3.33
monitoring
continual checking, supervising, critically observing, or determining the status, in order to identify change
from the performance level required or expected
[SOURCE: EN ISO 11139:2018, 3.180]
3.34
operating cycle
complete set of stages of a process that is carried out, in a specified sequence
Note 1 to entry: Loading and unloading are not part of the operating cycle.
[SOURCE: EN ISO 11139:2018, 3.188]
3.35
operating pressure
fluid pressure occurring during an operating cyc
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...