SIST EN 16372:2015
(Main)Aesthetic surgery services
Aesthetic surgery services
This European Standard addresses the requirements for clinical aesthetic practice: This covers surgical services to patients who want to change their physical appearance.
This European Standard provides recommendations for procedures for clinical treatment, including the ethical framework and general principles according to which clinical services are provided by all aesthetic practitioners. These recommendations apply before, during and after the procedure.
Dentistry ) procedures, reconstructive surgery procedures and aesthetic non-surgical medical procedures are excluded from the scope of this European Standard.
Aesthetic non-medical procedures (e.g. tattoos, piercing) which can be legally performed by non-physicians (e.g. beauty therapists, hairdressers) are excluded from the scope of this European Standard.
Dienstleistungen in der ästhetischen Chirurgie
Diese Europäische Norm legt Anforderungen an die klinisch ästhetische Praxis fest: Dies gilt für chirurgische Dienstleistungen für Patienten, die beabsichtigen, ihre äußere Erscheinung zu ändern.
Diese Europäische Norm gibt Empfehlungen in Bezug auf Verfahrensweisen der klinischen Behandlung, einschließlich des ethischen Rahmens und allgemeiner Grundsätze, nach denen klinische Dienstleistungen durch alle Ärzte in der ästhetischen Chirurgie erbracht werden. Diese Empfehlungen gelten vor, während und nach der Behandlung.
Verfahren der Zahnheilkunde1) sowie der rekonstruktiven Chirurgie und ästhetische nicht-chirurgische medizinische Eingriffe sind aus dem Anwendungsbereich dieser Europäischen Norm ausgeschlossen.
Ästhetische nicht-medizinische Verfahren (z. B. Tätowierungen, Piercing), die von anderen nichtärztlichen Fachgruppen (z. B. von Kosmetikern, Friseuren) auf gesetzlich zulässige Weise durchgeführt werden können, sind aus dem Anwendungsbereich dieser Europäischen Norm ausgeschlossen.
Services en chirurgie esthétique
La présente Norme européenne prévoit les exigences concernant la pratique de la chirurgie esthétique. Elle concerne les actes chirurgicaux proposés aux patients désirant modifier leur apparence physique.
La présente Norme européenne fournit des recommandations sur les procédures liées aux interventions chirurgicales, y compris un cadre éthique et des principes généraux d’exécution des actes chirurgicaux par tous les praticiens de chirurgie esthétique. Ces recommandations sont applicables avant, pendant et après l’intervention.
Le domaine d’application de la présente Norme européenne n’inclut pas les interventions en dentisterie ), les interventions de chirurgie reconstructive et les procédures de médecine esthétique non chirurgicales.
Les actes esthétiques non médicaux (par exemple le tatouage, les piercings) qui peuvent être légalement réalisées par des non-médecins (par exemple les esthéticiennes, les coiffeurs) sont également exclues du champ d’application de cette Norme européenne.
Storitve estetske kirurgije
Ta evropski standard določa zahteve in podaja priporočila storitev estetske kirurgije pacientom, vključno z etičnim okvirom ter splošnimi načeli, v skladu s katerimi te storitve (in sicer prej, med in po posegu) zagotavljajo vse ustanove.
General Information
- Status
- Published
- Public Enquiry End Date
- 15-Jul-2013
- Publication Date
- 18-Jan-2015
- Technical Committee
- I13 - Imaginarni 13
- Current Stage
- 6060 - National Implementation/Publication (Adopted Project)
- Start Date
- 05-Jan-2015
- Due Date
- 12-Mar-2015
- Completion Date
- 19-Jan-2015
- Ref Project
EN 16372:2014 - Aesthetic surgery services
Overview
EN 16372:2014 - Aesthetic surgery services is a European Standard published by CEN that defines requirements and recommendations for clinical aesthetic practice. It covers surgical services provided to patients who seek to change, restore or improve their physical appearance and sets out an ethical and clinical framework for care before, during and after procedures. The standard focuses on patient safety, quality of service and consistent professional practice across Europe.
Note: the standard excludes dentistry, reconstructive surgery, aesthetic non‑surgical medical procedures and legally permitted non‑medical aesthetic services (e.g., tattoos, piercing).
Key topics and requirements
EN 16372:2014 addresses practical and technical areas including:
- Competencies and training
- Requirements for practitioner qualifications, documented competence, continuing professional development (CPD/CME) and recommended registration for aesthetic surgeons.
- Management and patient communication
- Patient consultation, assessment, informed consent, documentation, investigations, cooling‑off periods, fees and medical indemnity.
- Clinical governance
- Risk management, adverse‑event reporting, complaints handling, confidentiality and ethical advertising (Code of Ethics in Annex A).
- Facilities and safety
- Facility evaluation, staffing, procedure rooms and operating theatre recommendations, hygiene, anaesthesia device considerations, medications and emergency/out‑of‑hours cover.
- Procedure classification and identification
- Guidance on categorising aesthetic surgical procedures by risk, practitioner, facility and anaesthesia level (annexes include practitioner classification and deviations).
- Post‑operative care
- Follow‑up, dressings, timing of procedures and management of multiple procedures to protect patient safety and outcomes.
Practical applications - who uses this standard
EN 16372:2014 is primarily used by:
- Private and public aesthetic surgery clinics and hospitals
- Plastic and cosmetic surgeons, clinical directors and facility managers
- Health‑care quality and compliance officers implementing clinical governance
- Regulators and accreditation bodies aligning local requirements with European practice
- Healthcare insurers and legal advisors assessing risk and indemnity needs
Practical uses include designing facility protocols, staff training programmes, informed‑consent processes, advertising practices, procedure classification, and audit/quality management systems.
Related standards
- EN 15224 (quality management system for health‑care services) and EN ISO 9001 references for QMS alignment.
- Annexes in EN 16372 provide a Code of Ethics, practitioner classification and guidance on deviations.
EN 16372:2014 is a key reference for organizations aiming to improve patient safety, standardize aesthetic surgical care and demonstrate compliance with European best practice.
Frequently Asked Questions
SIST EN 16372:2015 is a standard published by the Slovenian Institute for Standardization (SIST). Its full title is "Aesthetic surgery services". This standard covers: This European Standard addresses the requirements for clinical aesthetic practice: This covers surgical services to patients who want to change their physical appearance. This European Standard provides recommendations for procedures for clinical treatment, including the ethical framework and general principles according to which clinical services are provided by all aesthetic practitioners. These recommendations apply before, during and after the procedure. Dentistry ) procedures, reconstructive surgery procedures and aesthetic non-surgical medical procedures are excluded from the scope of this European Standard. Aesthetic non-medical procedures (e.g. tattoos, piercing) which can be legally performed by non-physicians (e.g. beauty therapists, hairdressers) are excluded from the scope of this European Standard.
This European Standard addresses the requirements for clinical aesthetic practice: This covers surgical services to patients who want to change their physical appearance. This European Standard provides recommendations for procedures for clinical treatment, including the ethical framework and general principles according to which clinical services are provided by all aesthetic practitioners. These recommendations apply before, during and after the procedure. Dentistry ) procedures, reconstructive surgery procedures and aesthetic non-surgical medical procedures are excluded from the scope of this European Standard. Aesthetic non-medical procedures (e.g. tattoos, piercing) which can be legally performed by non-physicians (e.g. beauty therapists, hairdressers) are excluded from the scope of this European Standard.
SIST EN 16372:2015 is classified under the following ICS (International Classification for Standards) categories: 11.020.10 - Health care services in general. The ICS classification helps identify the subject area and facilitates finding related standards.
SIST EN 16372:2015 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.Storitve estetske kirurgijeDienstleistungen in der ästhetischen ChirurgieServices en chirurgie esthétiqueAesthetic surgery services11.020.10Zdravstvene storitve na splošnoHealth care services in generalICS:Ta slovenski standard je istoveten z:EN 16372:2014SIST EN 16372:2015en01-februar-2015SIST EN 16372:2015SLOVENSKI
STANDARD
EUROPEAN STANDARD NORME EUROPÉENNE EUROPÄISCHE NORM
EN 16372
December 2014 ICS 03.080.99; 11.020 English Version
Aesthetic surgery services
Services en chirurgie esthétique
Dienstleistungen in der ästhetischen Chirurgie This European Standard was approved by CEN on 28 October 2014.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, Former Yugoslav Republic of Macedonia, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre:
Avenue Marnix 17,
B-1000 Brussels © 2014 CEN All rights of exploitation in any form and by any means reserved worldwide for CEN national Members. Ref. No. EN 16372:2014 ESIST EN 16372:2015
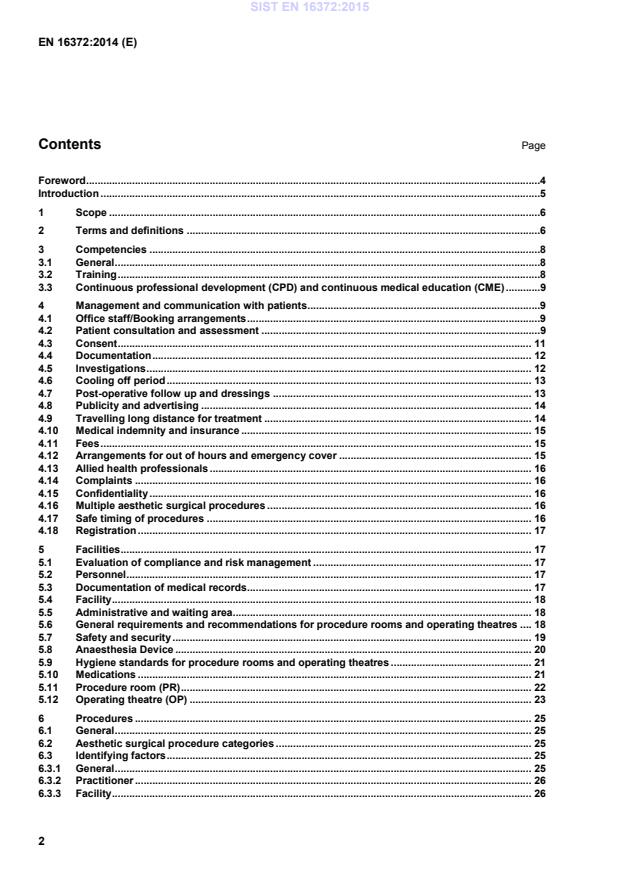
Code of Ethics for marketing and advertising. 30 Annex B (informative)
Classification of practitioners . 32 Annex C (informative)
A–deviations . 33 Bibliography . 43
1) As defined in EN ISO 1942. SIST EN 16372:2015
...



Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...