SIST EN 17398:2020
(Main)Patient involvement in health care - Minimum requirements for person-centred care
Patient involvement in health care - Minimum requirements for person-centred care
This document specifies minimum requirements for patient involvement in health care services with the aim to create favourable structural conditions for person-centred care.
It is applicable for use before, during and after the actual care that is provided by the care personnel.
This document is also applicable for use on a strategic level for quality assurance and quality improvement, for procurement, educational and supervisory purposes and as a guiding document for research and development projects in the field of intervention and implementation of person-centred care.
Patientenbeteiligung bei der Gesundheitsversorgung - Mindestanforderungen an die personenzentrierte Versorgung
Dieses Dokument legt Mindestanforderungen für die Patientenbeteiligung in Dienstleistungen für die Gesundheitsversorgung fest, mit dem Ziel, günstige strukturelle Bedingungen für die personenzentrierte Versorgung zu schaffen.
Es ist zur Nutzung vor, während und nach der tatsächlichen Pflege durch das Personal der Gesundheitsversorgung anwendbar.
Dieses Dokument ist ferner zur Nutzung auf strategischer Ebene zur Qualitätssicherung und -verbesserung, für Zwecke der Beauftragung, Ausbildung und Überwachung sowie als Leitdokument für Forschungs- und Entwicklungsprojekte im Bereich der Vermittlung und Umsetzung der personenzentrierten Versorgung anwendbar.
Implication du patient dans les soins de santé - Exigences minimales relatives aux soins axés sur la personne
Le présent document spécifie les exigences minimales relatives à l’implication du patient dans les services de soins de santé dans le but de créer des conditions structurelles propices aux soins centrés sur la personne.
Il est destiné à être utilisé avant, pendant et après les soins prodigués par le personnel soignant.
Le présent document est également destiné à être utilisé au niveau stratégique pour l’assurance qualité et l’amélioration de la qualité, pour l’approvisionnement, la formation et la supervision, ainsi que comme document de référence pour les projets de recherche et de développement dans le cadre de l’intervention et de la mise en oeuvre de soins centrés sur la personne.
Vključevanje bolnikov v zdravstveno oskrbo - Minimalne zahteve za oskrbo, osredotočeno na posameznika
General Information
- Status
- Published
- Public Enquiry End Date
- 31-Jul-2019
- Publication Date
- 22-Jun-2020
- Technical Committee
- I13 - Imaginarni 13
- Current Stage
- 6060 - National Implementation/Publication (Adopted Project)
- Start Date
- 18-Jun-2020
- Due Date
- 23-Aug-2020
- Completion Date
- 23-Jun-2020
Overview
EN 17398:2020 (CEN) - "Patient involvement in health care - Minimum requirements for person‑centred care" defines baseline requirements to create favourable structural conditions for patient involvement and person‑centred care (PCC). The standard applies across the care pathway - before, during and after care - and at multiple levels: point‑of‑care, organisational and strategic. It is intended for use in clinical practice, quality assurance, procurement, education, supervision and research and supports integration of the patient perspective into health services.
Key topics and requirements
EN 17398:2020 focuses on practical, minimum requirements to enable partnership between patients and care personnel. Core technical topics include:
- Patient’s narrative and experience of illness
- Prioritise the patient’s story and perspective as the basis for planning and decision‑making.
- Partnership and shared decision‑making
- Structures and processes to support two‑way communication and consensus on goals and outcomes.
- Documentation, care plan and information sharing
- Access to, and input on, individual care plans; consistent documentation that reflects the patient’s preferences and self‑care strategies.
- Patient and public involvement in management and policy
- Inclusion of patient views in organisational governance, procurement, service design and quality improvement.
- Operational vs strategic requirements
- Distinct requirements at organisational level (policies, resources, training) and at point‑of‑care (interaction, care planning, follow‑up).
- Guidance annexes
- Informative examples and tools (Annex A) and practical guidance for applying PCC across care levels and phases (Annex B).
The standard highlights evidence that PCC improves medical outcomes, self‑efficacy and care processes (Cochrane review cited), and underscores confidentiality, consent and involvement of family/support networks where appropriate.
Applications and who should use it
EN 17398:2020 is relevant to:
- Healthcare providers (primary care, hospitals, dental, rehabilitation, long‑term and home care)
- Clinical managers and quality assurance teams
- Procurement officers (embedding patient involvement in contracts)
- Educators and training programs (PCC competencies)
- Policy makers and researchers designing PCC interventions
- Patient advocacy groups and public involvement coordinators
Use cases:
- Drafting or updating care plans and documentation practices
- Developing organisational policies to embed shared decision‑making
- Designing procurement specifications that require patient involvement
- Structuring patient participation in governance and quality improvement
Related standards
- EN 15224 (quality management in health care) - the document notes EN 17398 can support patient‑involvement aspects of quality systems such as EN 15224.
Keywords: EN 17398:2020, patient involvement, person‑centred care, care plan, shared decision‑making, documentation, healthcare procurement, quality assurance, CEN.
Frequently Asked Questions
SIST EN 17398:2020 is a standard published by the Slovenian Institute for Standardization (SIST). Its full title is "Patient involvement in health care - Minimum requirements for person-centred care". This standard covers: This document specifies minimum requirements for patient involvement in health care services with the aim to create favourable structural conditions for person-centred care. It is applicable for use before, during and after the actual care that is provided by the care personnel. This document is also applicable for use on a strategic level for quality assurance and quality improvement, for procurement, educational and supervisory purposes and as a guiding document for research and development projects in the field of intervention and implementation of person-centred care.
This document specifies minimum requirements for patient involvement in health care services with the aim to create favourable structural conditions for person-centred care. It is applicable for use before, during and after the actual care that is provided by the care personnel. This document is also applicable for use on a strategic level for quality assurance and quality improvement, for procurement, educational and supervisory purposes and as a guiding document for research and development projects in the field of intervention and implementation of person-centred care.
SIST EN 17398:2020 is classified under the following ICS (International Classification for Standards) categories: 11.020.10 - Health care services in general. The ICS classification helps identify the subject area and facilitates finding related standards.
SIST EN 17398:2020 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-september-2020
Vključevanje bolnikov v zdravstveno oskrbo - Minimalne zahteve za oskrbo,
osredotočeno na posameznika
Patient involvement in health care - Minimum requirements for person-centred care
Patientenbeteiligung bei der Gesundheitsversorgung - Mindestanforderungen an die
personenzentrierte Versorgung
Implication du patient dans les soins de santé - Exigences minimales relatives aux soins
axés sur la personne
Ta slovenski standard je istoveten z: EN 17398:2020
ICS:
11.020.10 Zdravstvene storitve na Health care services in
splošno general
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
EN 17398
EUROPEAN STANDARD
NORME EUROPÉENNE
June 2020
EUROPÄISCHE NORM
ICS 11.020.10
English Version
Patient involvement in health care - Minimum
requirements for person-centred care
Implication du patient dans les soins de santé - Patientenbeteiligung bei der Gesundheitsversorgung -
Exigences minimales relatives aux soins centrés sur la Mindestanforderungen an die personenzentrierte
personne Versorgung
This European Standard was approved by CEN on 10 May 2020.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this
European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references
concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN
member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by
translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management
Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2020 CEN All rights of exploitation in any form and by any means reserved Ref. No. EN 17398:2020 E
worldwide for CEN national Members.
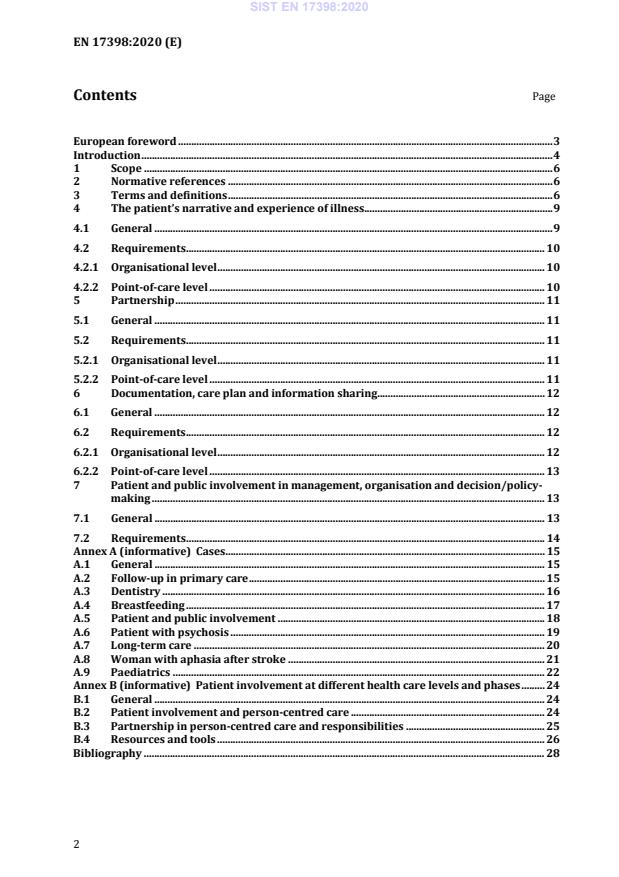
Contents Page
European foreword . 3
Introduction . 4
1 Scope . 6
2 Normative references . 6
3 Terms and definitions . 6
4 The patient’s narrative and experience of illness. 9
4.1 General . 9
4.2 Requirements . 10
4.2.1 Organisational level . 10
4.2.2 Point-of-care level . 10
5 Partnership . 11
5.1 General . 11
5.2 Requirements . 11
5.2.1 Organisational level . 11
5.2.2 Point-of-care level . 11
6 Documentation, care plan and information sharing . 12
6.1 General . 12
6.2 Requirements . 12
6.2.1 Organisational level . 12
6.2.2 Point-of-care level . 13
7 Patient and public involvement in management, organisation and decision/policy-
making . 13
7.1 General . 13
7.2 Requirements . 14
Annex A (informative) Cases . 15
A.1 General . 15
A.2 Follow-up in primary care . 15
A.3 Dentistry . 16
A.4 Breastfeeding . 17
A.5 Patient and public involvement . 18
A.6 Patient with psychosis . 19
A.7 Long-term care . 20
A.8 Woman with aphasia after stroke . 21
A.9 Paediatrics . 22
Annex B (informative) Patient involvement at different health care levels and phases . 24
B.1 General . 24
B.2 Patient involvement and person-centred care . 24
B.3 Partnership in person-centred care and responsibilities . 25
B.4 Resources and tools . 26
Bibliography . 28
European foreword
This document (EN 17398:2020) has been prepared by the Technical Committee CEN/TC 450
“Patient involvement in person-centred care”, the secretariat of which is held by SIS.
This European Standard shall be given the status of a national standard, either by publication of an
identical text or by endorsement, at the latest by December 2020, and conflicting national standards
shall be withdrawn at the latest by December 2020.
Attention is drawn to the possibility that some of the elements of this document may be the subject
of patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
According to the CEN-CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria,
Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary,
Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal,
Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland,
Turkey and the United Kingdom.
Introduction
This document aims to facilitate patient involvement and the development of a partnership between
the patient and the care personnel. Patient involvement and partnership are based on the patient’s
resources and capacities as well as wishes and needs, primarily focusing on the patient ́s narrative,
shared decision-making, information sharing as well as documentation on the individual, operational
and strategic level (see Annex B).
Guiding principle
This document provides minimum requirements for patient involvement in health care. It aims to
facilitate the partnership between patients and care personnel in the design, implementation and
evaluation of health care services. The document can be used as an aid in the planning, management,
implementation and systematic evaluation of daily activities, enabling the patients to manage their
daily life and empowering them in the care process. Furthermore, it can be used to support patient
involvement on a systemic level; ensuring that the patient perspective is included in the
development, implementation and evaluation of health care services, research and policies.
This document focuses on patient involvement in health care. However, in many situations social
care is closely related to, or is provided along with, health care services. Thus, this document could
be used as a guide for social care alongside health care services.
This document applies to all health care services, e.g. in general practices, primary care centres,
dental practices, home care, rehabilitation, preventive and long-term care. Further, when the needs
of the patients are being considered, the family and the support networks around the patient such as
patient proxies should be included where appropriate (see Annex B).
This document can be used before, during and after a procurement process. It provides all parties
with a common understanding of the minimum level of patient involvement and enables the
establishment of related processes and structures for all aspects of the contact between the patient,
the care personnel and the health care service providers. This also includes transitions between
different levels of care.
The document can be used for education, training and continuous development (see Annex B). The
document can also serve as support when it comes to quality aspects related to patient involvement,
e.g. in EN 15224.
Patient involvement
Effective inter-professional communication, which involves the patient in the sharing of knowledge
and creating a common understanding of objectives and self-care strategies, is a key aspect of care
optimization. The health care providers should create favourable conditions for establishing a
partnership with the patient.
A partnership involving patients should be based on confidentiality, privacy and necessary consents,
when applicable, and encompass:
— at least two parties, including the patient;
— the sharing of information and knowledge, taking into account the patient’s perspective;
— a common strive towards a consensus for the setting of objectives and outcomes;
— a context where the patient has access to documentation and can provide input on the care plan
and any follow-up thereof.
Person-centred care
Person-centred care (PCC) is an approach in which patients take part in their care, self-care and in
the decision-making process. A person has capacities, feelings, wishes and needs – and should
therefore become a partner (in some cases also involving patient proxies) in their care and treatment.
This reflects an understanding that patients are, by virtue of their health knowledge and experience,
experts on their own health status. Patients are persons and should not be reduced to their health
status alone, but rather be integrated within a given environment, with their rights and future plans
being recognized. Hence, for most of time, the patient is not in a health care context. Therefore, there
is strong reason to acknowledge and endorse every patient’s resources, interests, needs and
responsibilities in situations which concern them. Especially in cases of life-long illness, persons
manage their life for the vast majority of time without care providers. This makes it important to
focus on the person’s self-care capacities. PCC is facilitated when care personnel work together with
users of health care services, tailoring the services to the resources, needs and goals of the individual.
PCC is a shared understanding and agreement about:
1. what really matters to the patient, in order to set care objectives that incorporate what health
and quality of life means for the individual person,
2. the professional assessment and guideline-driven care that incorporates evidence-based care
and national/local routines (see Annex A for examples).
Patients and care personnel identify and discuss problems and strategies related to the patient’s
condition(s), giving due consideration to the patient's experiences and preferences, clinical analyses,
tests and treatments and to the practical, social, and emotional effects of the condition(s) and care on
their daily life.
In a Cochrane review of central PCC components (including almost 11,000 patients), significant
improvements were observed in medical outcomes, self-efficacy and self-care when PCC was applied.
Controlled clinical trials have shown positive outcomes in terms of shorter hospitalization periods,
cost reduction, improved everyday life activities and discharge process, increased self-efficacy,
disease knowledge, improved health status and improved life quality in end of life care.
While the above mentioned approaches are often seen as a basis for modern health care, testimonies
point to the lack of structure, knowledge and policies to operationalise patient involvement.
1 Scope
This document specifies minimum requirements for patient involvement in health care services with
the aim to create favourable structural conditions for person-centred care.
It is applicable for use before, during and after the actual care that is provided by the care personnel.
This document is also applicable for use on a strategic level for quality assurance and quality
improvement, for procurement, educational and supervisory purposes and as a guiding document
for research and development projects in the field of intervention and implementation of person-
centred care.
2 Normative references
There are no normative references in this document.
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
• IEC Electropedia: available at http://www.electropedia.org/
• ISO Online browsing platform: available at https://www.iso.org/obp
3.1
care
activities within health care services, social care services or an integration of both, including care
provided by informal carers
Note 1 to entry: An informal carer includes any person such as a family member, friend or a neighbour, who
provides regular ongoing assistance to another person.
3.2
care period
time during which a person receives care (3.1), running from the first request or contact between the
care seeker and care provider to the end of the episode of care
3.3
care personnel
persons working in the provision of health care (3.8) or social care (3.24) services, whether as
individual practitioners or employees of health institutions and programmes
3.4
care plan
plan of needs, expectations, goals, resources and treatment, developed by the care provider in
partnership (3.13) with the patient (3.14)
Note 1 to entry: In some European countries, an individual care plan is required by national legislation for
patients with long term health needs.
3.5
contact
any interaction or communication between the patient (3.14) and the care personnel (3.3)
Note 1 to entry: Interaction includes physical and non-physical communication as facilitated by assistive
technology.
3.6
continuum of care
provision and consistency of care (3.1) over a period of time spanning all levels and intensities of
care, and including self-care
3.7
documentation
record of the health status (3.10), health care (3.8) and social care (3.24) of a patient, based on the
patient's narrative (3.12)
3.8
health care
care activities, services, management or supplies related to the health of an individual
Note 1 to entry: activities undertaken by care personnel are intended to maintain and improve health,
prevent harm and illness, slow down the deterioration of health and alleviate pain and suffering
[SOURCE: EN ISO 13940:2016, 3.1.1, modified - Note 1 to entry has been replaced]
3.9
health care services
services covering the whole spectrum of care (3.1), from promotion and prevention to diagnostic,
rehabilitation and palliative care, as well as all levels of care including self-care, home care,
community care, primary care, long-term care and hospital care for the purpose of providing
integrated health services throughout life
3.10
health status
level of health of a person as assessed in relation to physical and mental functions, body structure,
personal factors, activities, participation and environmental aspects
3.11
inter-professional team
team composed of members from the same or different professions and occupations with varied and
specialised knowledge, skills and methods, who are committed to a common purpose, approach and
performance goals for which they are held mutually accountable
Note 1 to entry: Terms such as interdisciplinary, inter-professional, multi-professional and multidisciplinary
are often used interchangeably.
3.12
narrative
patients' own account of what matters to them in the present situation, past experiences and future
expectations
3.13
partnership
relationship of collaboration and mutual respect between a patient (3.14) and care personnel (3.3)
3.14
patient
person seeking or needing care or receiving health care (3.8) or social care (3.24) services
Note 1 to entry: In situations where a patient, for whatever reason, are incapable of defending their interest,
a patient proxy assists or represents the patient.
Note 2 to entry: In some care facilities, patients are not referred to as “patients” but rather as residents,
clients, etc.
Note 3 to entry: A patient may or may not have a diagnosis.
3.15
patient involvement
patients' participation in their care on the organisational and/or individual level
3.16
patient proxy
representative who assists or acts on behalf of the patient (3.14) in the narrative (3.12), decision-
making and patient care process (3.17)
Note 1 to entry: The term patient proxy can be subject to different meanings and legal contexts in national
legislation.
3.17
process
set of interrelated or interacting activities that use inputs to deliver an intended result
[SOURCE: ISO 9000:2015, 3.4.1]
3.18
public involvement
participation, or attempt thereto, of public or lay people and/or organisations in decision and policy
making
3.19
quality in health care
degree to which health care fulfils requirements related to defined quality aspects
[SOURCE: EN 15224:2016, 3.11]
3.20
quality of life
persons' perception of life in terms of physical and mental state, personal beliefs, social relations and
relationship to their personal environment
3.21
self-care
persons' behaviour and actions regarding their own health and care (3.1), and ability to engage in
health promoting activities, if needed facilitated by partnership (3.13) between the patient and care
personnel or other parties
3.22
service
output of an organisation with at least one activity necessarily performed between the organisation
and the customer
Note 1 to entry: In health care and social care, the service can be provided by an individual.
[SOURCE: ISO 9000:2015, 3.7.7, modified - Note 1 to entry has been added]
3.23
shared decision-making
decision-making made in in partnership (3.13) between patient (3.14) and care personnel (3.3)
3.24
social care
care (3.1) provided with a focus to assist and support a patient in coping with activities of everyday
life
Note 1 to entry: There are variations in social care content in different European countries and the care can be
regulated in national legislation.
4 The patient’s narrative and experience of illness
4.1 General
The patient’s narrative is essential when it comes to identifying patients' views of their objectives,
needs, preferences, values and resources, as well as perception of their own role in their care. The
narrative includes information regarding the patient’s everyday life, condition, symptoms, disease
knowledge and perception, and motivation/objectives. The question “what matters to you” can be a
starting point that helps the patients present themselves as persons through a narrative (see
Clause A.1). The narrative should in turn build on partnership between the care personnel and
patient which encourages and empowers the patient to take part in the care process.
The patient's narrative enables care personnel to listen and try to understand the request (for health
care services) of each specific individual. It can be a request for preventive care or relate to the
patient’s experience of illness. Diseases and conditions can be described according to different
criteria, but to understand what illness means in everyday life, the care personnel should listen
carefully to each patient’s narrative. It is the care personnel’s responsibility to understand the
patient’s objectives, knowledge, self-management skills and confidence, to strengthen these aspects
where necessary and to ensure that relevant interventions and support services are available (see
Clause A.3). The essence is to understand what an illness means in the everyday life of the person.
This should be the point of departure for all subsequent interventions in the care of that person. This
can be obtained through a narrative, but also through other means of communication when the
patient is not able to provide a narrative. Necessary insights (see Clause A.7 for example) are
obtained through a process of interpretation of words or observations carried out by the care
personnel.
In order to facilitate patient involvement in health care services, the following focus areas regarding
the patient’s narrative and experience of illness, should be taken into account in order to guide the
care process:
— inter-professional and person-centred approach;
— respect for values, preferences and expressed needs;
— physical comfort;
— emotional support.
Effective communication between care personnel and patients is a prerequisite for patient
involvement. It needs to be recognized that e.g. sensory or cognitive impairments, educational
differences, differences in language, or culture can hamper communication between the patient and
care personnel (see Clause A.7).
In paediatric settings, the patients may be represented by their parent or legal guardian who can help
form their narrative of the illness or the experience of illness. However, it is also essential to involve
children and young people, as much as possible and in an appropriate way, in discussions about their
care, even if they are not able to make decisions of their own. Young patients' abilities to
communicate and contribute to narratives and make decisions, depends more on their ability to
understand and consider options, than on their age. It is important that a the patient’s maturity and
understanding is assessed on an individual basis. Even a very young child will be able to contribute
to some degree (see Clause A.9 for example).
4.2 Requirements
4.2.1 Organisational level
The organisation shall ensure that:
a) the patient’s narrative can be shared within patient confidentiality among parties in the inter-
professional team as soon as possible, including, if needed, all subsequent revisions of the
narrative which are required during the care period;
b) the environment facilitates the capturing and sharing of the patient's narrative, while
recognizing the need for privacy;
c) time for the care personnel is set aside for discussion and exploration of the patient's narrative;
d) the care personnel is trained to obtain the narrative.
4.2.2 Point-of-care level
The care personnel shall ensure that:
a) patients are prepared, and given the opportunity, to provide their narrative at each care contact;
b) the following aspects can be included in the patient narrative:
— the reason why the patient is seeking help or advice, and how the everyday life is affected;
— the patient's feeling of wellbeing;
— the patient's objectives, motivations and values regarding the care process and care
outcomes;
c) in cases where it is not possible to obtain a narrative, an alternative approach is used to capture
the information needed.
5 Partnership
5.1 General
The use of an inter-professional and person-centred approach throughout the continuum of care,
including transitions between levels of care, where the patient is a partner of the team, is a key aspect
of care. All involved experts, including the patient, should be taking part in the care-related decisions.
In order to facilitate patient involvement in health care services, the following focus areas should be
taken into account in order to guide the partnership process:
— inter-professional and person-centred approach;
— coordination and integration of care;
— information;
— communication;
— continuous education.
5.2 Requirements
5.2.1 Organisational level
The organisation shall ensure that:
a) there are routines enabling the patient to be continuously involved in the decision-making
process, as well as the follow up and revision (if necessary) of the care process during the care
period;
b) there are routines in place to ensure that time is set aside for the care personnel to establish a
partnership;
c) in situations where a partnership is not possible due to the patient’s cognitive or physical status,
language barriers or other aspects of communication, decisions made by the care personnel shall
be duly documented and re-evaluated as soon as possible together with the patient.
5.2.2 Point-of-care level
The care personnel shall ensure that:
a) the patient’s understanding of shared decision-making is assessed, and that the patient's
preferences are documented;
b) the patient’s motivations, values, and objectives are discussed, and strategies for the patient’s
resources, objectives, wishes and needs are incorporated into the care plan;
c) the patient and the care personnel have a common and mutual understanding regarding the care,
impact on symptoms and possible side effects, including the foreseeable consequences of lack of
care;
d) the patient’s concerns and fears are discussed and strategies for reducing the patient's concerns
and fears are incorporated into the care plan;
e) shared decision-making processes are upheld throughout the care period, and, if required, also
throughout the continuum of care, including self-care;
f) a common agreement is established regarding the responsibilities of the patient and the care
personnel in the agreed care plan, for the current care episode, and, if needed, also for the
continuum of care;
g) the resource/outcome considered possible and realistic are discussed and that a common
understanding therefore is reached between the patient and the care personnel. If no common
understanding or agreement can be reached regarding a central aspect of the care process, the
divergent opinions shall be documented;
h) resources, including training and information, are provided to the patient in order to facilitate
self-care.
6 Documentation, care plan and information sharing
6.1 General
Documentation can take the form of a care plan, either using digital or traditional media, to provide
information on the patient’s objectives, preferences and values within patient confidentiality.
The use of a structured care plan has resulted in positive outcomes in a range of different hospital
settings and throughout the continuum of care. The care plan is subject to discussion and, if
necessary, revised together with the patient throughout the continuum of care. Joint decisions, and
the documentation thereof, safeguards patient involvement. Patient’s involvement is documented in
the form of the patient's preferences, beliefs and values, as well as participation in the care and
treatment-related decisions (see Clause A.2). It is also important to highlight that the key issue here
is not only documentation, but co-creation and information sharing.
In order to facilitate patient involvement in health care services, the following focus areas should be
taken into account in order to guide the documentation process:
— access to relevant and understandable information;
— communication;
— continuous education;
— continuum of care;
— continuous documentation.
6.2 Requirements
6.2.1 Organisational level
The organisation shall ensure that:
a) there are routines in place for the care personnel to review the care plan, as well as for
continuous patient access to the updated care plan;
b) there are routines in place for the allocation of time for the care personnel to document the
narrative and establish and review the care plan.
6.2.2 Point-of-care level
The care personnel shall ensure that:
a) the patient takes part in the planning, monitoring and evaluation of the care plan and the
discharge planning;
b) the care plan is documented in partnership with the patient, and accessible to the patient;
c) the patient’s symptoms, resources and needs are monitored and evaluated in a systematic way,
using validated instruments where available.
7 Patient and public involvement in management, organisation and
decision/policy-making
7.1 General
Patient involvement in health care services implies that the patient’s perspective is considered at all
strategic levels of the management of care as well as in research, development, education, training
and policies. It is not limited to the individual patient contact but may also include the structure and
organisation of the care in all stages of the patient's care path. Hence, public and patient involvement
should be ensured at all strategic management levels in order to safeguard that the patient’s
perspective is considered in the health care services (see Clause A.4). Patient involvement is an
important element in the constant improvement processes in the continuum of care, including but
not limited to health and technology assessments, legislation, pricing and reimbursement policies.
In order to facilitate public and patient involvement in health care services, the following focus areas
should be taken into account in order to guide the care process:
— inter-professional approach;
— patient involvement;
— continuum of care;
— accessibility;
— continuity.
This section provides an overview of the structures, responsibilities and resources, which are
required to ensure continuous improvement and learning at the point of care. The focus is put on
outcomes of importance to the patients and their relatives. For small and medium size organisations,
some of these requirements could, where applicable, be applied in the context of an overarching
association or network. The requirements are still applicable to the small and medium size
organisation.
7.2 Requirements
Management teams, organisations and decision-makers/policy-makers shall ensure:
a) an inter-professional approach to quality improvement on the operational and strategic
development level, including the involvement of patient’s proxies;
b) a structured evaluation and follow up of patient reported outcome measurements (PROM), such
as symptoms, functional capacities, quality of life, health status, and patient reported experience
measurements (PREM) during and after the care periods;
c) the encouragement and provision of necessary resources and structures for patient involvement
on the organisational and system level and, if needed, the establishment of patient organisations;
d) education and continuous training in patient involvement as part of the training of care
personnel and other staff members;
e) the creation of structures and policies for systematic quality and safety improvement regarding
patient involvement;
f) periodical monitoring of documented care plans that include patient objectives and shared
decision-making. If the set objectives are not met, an improvement plan shall be developed,
operationalised and evaluated within the following year.
Annex A
(informative)
Cases
A.1 General
This annex illustrates how patients can be involved in different ways by giving examples and practical
advice through the description of cases. The cases can be used as examples in the application of this
document at all health care service levels.
A.2 Follow-up in primary care
Gary is a 72-year-old retired businessman and devoted golfer who suffered a minor myocardial
infarction 15 years ago. After the recovery, he returned to playing golf and was in good health until
he one day collapsed. Resuscitation was immediately initiated. He was referred to a tertiary hospital
to receive an Implantable Cardiac Defibrillator (ICD). However, a new angiography of his coronary
lesion indicated a potential need for a coronary by-pass operation. The operation was scheduled a
month afterwards.
Gary was very worried about the upcoming surgery. He was so concerned about his condition that
he did not dare to go for a walk and gave up golfing. None of the records made any reference to Gary's
concerns about surgery or his treatment preferences. Since the care personnel had simply informed
him that he was to undergo surgery, he assumed that he had no other option.
What can we do to improve patient involvement?
With respect to the patient's narrative:
Through the patient's narrative, the care personnel can identify Gary's objectives, needs, preferences,
values and resources. The narrative can be obtained by asking questions such as “what matters to
you?”. This would have made it possible for Gary to indicate that, in order to maintain a good quality
of life, it was important to him to remain physically active and play golf. After collection of medical
data, different treatment options and information from the patient (needs, preferences etc.), the care
personnel and Gary should have chosen the treatment in shared decision-making.
These actions are in compliance with the requirement in 4.2.1 c): The organisation shall ensure that
time for the care personnel is set aside for discussion and exploration of the patient's narrative.
With respect to partnership between the patient and the care personnel:
Based on the narrative, we know that Gary prefers a treatment that has as little effect on his physical
mobility as possible and we can assume that, if possible, he would prefer not having surgery. From
the narrative, we can also deduct that Gary had no symptoms such as dyspnoea or chest pain. Gary
met his friend and neighbour Dr. S. who offered him a second opinion. After reviewing Gary's records,
Dr. S. concluded that his condition did not clearly require by-pass surgery and that pharmacological
treatment was a viable option. After the care personnel and Gary had exchanged views, and collected
and discussed the necessary information, Gary decided not to have the surgery and continue with his
medication instead.
These actions are in compliance with requirement 5.2.2 c): The care personnel shall ensure that the
patient and the care personnel have a common and mutual understanding regarding the care, impact
on symptoms and possible side effects, including the foreseeable consequences of lack of care.
With respect to the patient’s care plan:
Dr. S. ensured him that the physicians would be informed of their discussion and that Gary's
treatment decision preferences would be documented in his patient record and that the treatment
options, e.g. a surgery, would still be valid in the future. After this talk, Gary was markedly relieved.
In the next three years, Gary has continued his pharmacologic treatment, felt well and enjoyed an
active life without any cardiac-related symptoms.
These actions are in compliance with requirement 6.2.2 c): The care personnel shall ensure that the
patient’s symptoms, resources and needs are monitored and evaluated in a systematic way, using
validated instruments where available.
A.3 Dentistry
John didn’t visit a dentist for some years, until he got worried over a gap between his front teeth in
the upper jaw. He visited dentist K., whose examination showed a developed periodontitis for which
John needed treatment in the form of scaling and root planning. Several teeth were also decayed and
needed filling treatment. John asked to be treated without anaesthesia and the dentist agreed without
asking why.
In the years that followed, John regularly visited the dentist for scaling treatment. The treatment
always followed the pattern of the first appointment: no use of anaesthesia. The periodontal disease
did not improve and several recently done fillings also failed.
What can we do to improve patient involvement?
With respect to the patient's narrative:
Since dentist K’s treatment did not produce any positive results, John one day decided to consult
dentist R. instead. His gum was bleeding, he had a bad breath and two recently filled teeth were
broken. John explained that he wanted to be treated in the same way as in dentist K’s practice, that is
without anaesthesia. Dentist R. tried to talk to John in order to find out why he had willingly been
suffering that pain for so many years. By taking the time to talk with the patient, dentist R. found out
that John was actually anxious about injections and afraid of needles. John explained the reasons why
he hadn't agreed to receive anaesthesia and therefore had suffered whenever he had to go to the
dentists.
These actions are in compliance with requirement 4.2.2 b): The care personnel shall ensure that the
following aspects can be included in the patient narrative:
— the reason why the patient is seeking help or advice, and how their everyday life is affected;
— the patient's feeling of wellbeing;
— the patient's objectives, motivations and values regarding the care process and care outcome.
With respect to the partnership between the patient and care personnel:
Dentist R. explained to John that a good treatment can only be provided using anaesthesia. The pain
from the scaling in the tooth pocket was so strong that the muscles in John’s face would otherwise be
so tense that an adequate scaling down to the bottom of the dental pockets would not be feasible.
He supported his explanation with X-rays of the patient’s teeth and tooth bone, showing the bone-
loss caused by the periodontal disease. He also explained step by step how the anaesthesia is injected
and that by locally numbing the area, John would not feel a thing. Dentist R. also comforted John by
saying he was welcome to express his fear and let him know if it hurt or if something was worrying
him. After both the dentist and the dental assistant reassured the patient, John agreed to a treatment
with anaesthesia. The treatment went smoothly and ended well.
These actions are in compliance with requirement 5.2.2 d): The care personnel shall ensure that the
patient’s concerns and fears are discussed and strategies for reducing the patient concerns and fears
are incorporated into the care plan.
With respect to the care plan of the patient:
Dentist R. explained, using the patient’s X-rays, that John also suffered from decayed teeth and that
treatment of these teeth using anaesthesia should be considered since problems would otherwise
arise in the near future. The patient agreed and after 4 more appointments five teeth had been
treated, with use of anaesthesia. The patient overcame his fear of needles and was very pleased.
In the next 6 years, the patient only had to see dentist R. for the annual check-up, and regular scaling
treatment. In the same period, the periodontal status of the patient improved, and no more teeth
were broken or fillings lost. John understood that his previous fear of needles had indirectly resulted
in an inferior treatment, forcing him to visit the dentist monthly in the past.
These actions are in compliance with requirement 6.2.2 a): The care personnel shall ensure that the
patient takes part in the planning, monitoring and evaluation of the care plan and the discharge
planning.
A.4 Breastfeeding
Alice was 26 weeks pregnant with her first child. Both mother and child were in good health and so
far, the pregnancy had gone well. When she was 20 years old, Alice had had a breast reduction
surgery due to neck and back complaints.
Alice wanted to breastfeed her child. She had studied the benefits of breastfeeding and was fully
convinced of thi
...



Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...