SIST EN 17387:2022
(Main)Chemical disinfectants and antiseptics - Quantitative test for the evaluation of bactericidal and yeasticidal and/or fungicidal activity of chemical disinfectants in the medical area on non-porous surfaces without mechanical action - Test method and requirements (phase 2, step 2)
Chemical disinfectants and antiseptics - Quantitative test for the evaluation of bactericidal and yeasticidal and/or fungicidal activity of chemical disinfectants in the medical area on non-porous surfaces without mechanical action - Test method and requirements (phase 2, step 2)
This document specifies a test method and the minimum requirements for bactericidal and yeasticidal and additionally fungicidal activity of chemical disinfectant products that form a homogeneous, physically stable preparation when diluted with hard water - or in the case of ready-to-use products - with water.
NOTE Dilutions are necessary as three concentrations in the active to non-active range are tested.
This document applies to products that are used in the medical area for disinfecting non-porous surfaces without mechanical action.
This document applies to areas and situations where disinfection or antisepsis is medically indicated. Such indications occur in patient care, for example:
- in hospitals, in community medical facilities and in dental institutions;
- in clinics of schools, of kindergartens and of nursing homes;
and can occur in the workplace and in the home. It can also include services such as laundries and kitchens supplying products directly for the patients.
EN 14885 specifies in detail the relationship of the various tests to one another and to use recommendations.
Using this document, it is possible to determine the activity of products like commercial formulations or active substances on bacteria and/or fungi in the conditions in which they are used and therefore it corresponds to a phase 2, step 2 test.
This method excludes the evaluation of the activity of products against mycobacteria and bacterial spores.
Chemische Desinfektionsmittel und Antiseptika - Quantitativer Versuch zur Bestimmung der bakteriziden und levuroziden und/oder fungiziden Wirkung chemischer Desinfektionsmittel im humanmedizinischen Bereich auf nicht porösen Oberflächen ohne mechanische Einwirkung - Prüfverfahren und Anforderungen (Phase 2, Stufe 2)
Dieses Dokument legt ein Prüfverfahren und die Mindestanforderungen an die bakterizide und levurozide und zusätzlich auch fungizide Wirkung von chemischen Desinfektionsmitteln fest, die bei Verdünnung mit Wasser standardisierter Härte als homogene, physikalisch stabile Zubereitung vorliegen bzw. bei gebrauchs¬fertigen Produkten mit Wasser verdünnt werden.
ANMERKUNG Verdünnungen sind erforderlich, da drei Konzentrationen im aktiven bis nichtaktiven Bereich geprüft werden.
Dieses Dokument gilt für Produkte, die ohne mechanische Einwirkung zur Desinfektion nichtporöser Oberflächen im humanmedizinischen Bereich verwendet werden.
Dieses Dokument gilt für Bereiche und unter Bedingungen, wo eine Desinfektion oder Antiseptik aus medizinischen Gründen angezeigt ist. Indikationen dieser Art liegen z. B. bei der Patientenbetreuung in:
- Krankenhäusern, kommunalen medizinischen Einrichtungen und im Dentalbereich;
- medizinischen Einrichtungen in Schulen, Kindergärten und Heimen;
vor und können auch am Arbeitsplatz und im häuslichen Bereich gegeben sein. Eingeschlossen sein können auch Einrichtungen wie Wäschereien und Küchen, die der direkten Versorgung der Patienten dienen.
EN 14885 legt im Einzelnen die Beziehungen der verschiedenen Prüfungen untereinander und zu den Anwendungsempfehlungen fest.
Mit diesem Dokument ist es möglich, die Wirkung von Produkten wie handelsüblichen Formulierungen oder Wirkstoffen unter den Bedingungen, unter denen sie verwendet werden, auf Bakterien und/oder Pilze zu bestimmen und entspricht somit einer Prüfung der Phase 2, Schritt 2.
Dieses Verfahren schließt die Bewertung der Wirkung von Produkten gegen Mykobakterien und bakterielle Sporen aus.
Antiseptiques et désinfectants chimiques - Essai quantitatif pour l’évaluation de l’activité bactéricide et levuricide et/ou fongicide des désinfectants chimiques utilisés en médecine sur des surfaces non poreuses sans action mécanique - Méthode d’essai et exigences (phase 2, étape 2)
Le présent document spécifie une méthode d’essai et les exigences minimales relatives à l’activité bactéricide, levuricide ainsi que fongicide des désinfectants chimiques qui forment une préparation homogène, physiquement stable, lorsqu’ils sont dilués dans l’eau dure ou - dans le cas de produits prêts à l’emploi - dans l’eau.
NOTE Des dilutions sont nécessaires car trois concentrations dont une concentration active et une concentration non active sont soumises à essai.
Le présent document s’applique aux produits utilisés en médecine pour désinfecter les surfaces non poreuses sans action mécanique.
Le présent document s’applique aux zones et aux situations où la désinfection ou l’antisepsie est médicalement préconisée. De telles indications se rencontrent dans le cadre des soins apportés aux patients, par exemple :
- dans des hôpitaux, centres de soins médicaux et cabinets dentaires ;
- dans des infirmeries d’écoles, de jardins d’enfants et de maisons de retraite ;
et peuvent aussi se rencontrer sur les lieux de travail ou à domicile. Elles peuvent également concerner des services tels que des blanchisseries et des cuisines qui fournissent des produits directement aux patients.
L’EN 14885 précise de manière détaillée la relation entre les différents essais et les recommandations d’utilisation.
Il est possible, en utilisant le présent document, de déterminer l’activité de produits tels que les formulations ou substances actives commerciales sur les bactéries et/ou champignons dans leurs conditions d’utilisation, ce qui correspond à un essai de phase 2, étape 2.
Cette méthode exclut l’évaluation de l’activité de produits sur les mycobactéries et les spores de bactéries.
Kemična razkužila in antiseptiki - Kvantitativni preskus na neporoznih površinah brez mehanskega delovanja za vrednotenje baktericidnega in/ali fungicidnega delovanja in delovanja kemičnih razkužil na kvasovke v humani medicini - Preskusna metoda in zahteve (faza 2, stopnja 2)
Ta evropski standard določa preskusno metodo in minimalne zahteve za baktericidno in/ali fungicidno delovanje kemičnih razkužil in/ali delovanje kemičnih razkužil na kvasovke, ki tvorijo homogen, fizikalno stabilen pripravek, če so razredčena s trdo vodo oziroma, pri proizvodih, ki so pripravljeni za uporabo, z vodo.
Ta evropski standard se uporablja za proizvode, ki se na zdravstvenem področju uporabljajo za razkuževanje neporoznih površin brez mehanskega delovanja.
Ta evropski standard se uporablja za področja in primere, ko obstajajo zdravniške indikacije za dezinfekcijo. Te indikacije se pojavljajo pri negi bolnikov, na primer:
v bolnišnicah, javnih zdravstvenih in zobozdravstvenih ustanovah;
v ambulantah šol, vrtcev in domov za starejše;
in lahko se pojavljajo na delovnem mestu ali doma. Vključujejo lahko tudi storitve, kot so pralnice in kuhinje, ki proizvode dostavljajo neposredno bolnikom.
OPOMBA: Ta metoda ustreza preskusu stopnje 2 faze 2.
Standard EN 14885 podrobno določa razmerje med različnimi preskusi in »priporočili za uporabo«.
General Information
- Status
- Published
- Public Enquiry End Date
- 01-Aug-2019
- Publication Date
- 12-Dec-2021
- Technical Committee
- KDS - Cosmetics, chemical disinfectants and surface active agents
- Current Stage
- 6060 - National Implementation/Publication (Adopted Project)
- Start Date
- 04-Mar-2021
- Due Date
- 09-May-2021
- Completion Date
- 13-Dec-2021
Overview
EN 17387:2021 (CEN) specifies a quantitative laboratory test method (phase 2, step 2) and minimum performance requirements to evaluate bactericidal, yeasticidal and fungicidal activity of chemical disinfectants and antiseptics used on non‑porous surfaces in the medical area. The standard applies to products that form a homogeneous, physically stable preparation when diluted with hard water (or ready‑to‑use products diluted with water). It simulates practical application conditions (temperature, contact time, organic load) and is used to determine activity on surfaces such as stainless steel without mechanical action.
Key topics and requirements
- Scope: Surface disinfection in medical settings (hospitals, dental clinics, nursing homes, schools, laundries, kitchens supplying patients, workplaces, home use where medically indicated).
- Test type: Phase 2, step 2 quantitative surface test - organisms are dried onto a stainless steel surface, treated with product, neutralized and surviving colony counts determined.
- Microorganisms: Mandatory strains include Staphylococcus aureus, Enterococcus hirae, Pseudomonas aeruginosa (bactericidal); Candida albicans (yeasticidal); Aspergillus brasiliensis and Candida albicans (fungicidal). Additional strains may be used for specific claims.
- Performance thresholds: Minimum ≥5 log10 reduction for bacteria and ≥4 log10 reduction for fungi under specified conditions.
- Test conditions:
- Temperature range: (4 ± 1) °C to (30 ± 1) °C (room temperature defined as 21.5 ± 3.5 °C).
- Contact times: from 1 min (minimum) up to 5 min for surfaces likely to contact patients/staff; up to 60 min permitted for other surfaces (tested at intervals as defined in the standard).
- Interfering substances: clean (0.3 g/L bovine albumin) and dirty (3.0 g/L bovine albumin + 3.0 mL/L erythrocytes).
- Method essentials: Three concentrations (active-to-non‑active range) are tested; validated neutralizers are used to stop product action; method excludes activity against mycobacteria and bacterial spores.
Applications
- Product development & registration: Manufacturers use EN 17387 to generate data for label claims and regulatory submission for surface disinfectants intended for medical use.
- Independent testing labs: Implement the standardized procedure to validate efficacy claims.
- Infection prevention teams & procurement: Use results to compare products for use in healthcare, dental, and communal care environments.
- Regulators & standards bodies: Reference the method to harmonize requirements across markets.
Related standards
- EN 14885 - application of European standards for chemical disinfectants and antiseptics (relationship of tests to use recommendations).
- EN 17272 - for airborne disinfection methods (EN 17387 is not intended for airborne applications).
Keywords: EN 17387, chemical disinfectants, surface disinfection test, bactericidal, yeasticidal, fungicidal, phase 2 step 2, non‑porous surfaces, CEN.
Frequently Asked Questions
SIST EN 17387:2022 is a standard published by the Slovenian Institute for Standardization (SIST). Its full title is "Chemical disinfectants and antiseptics - Quantitative test for the evaluation of bactericidal and yeasticidal and/or fungicidal activity of chemical disinfectants in the medical area on non-porous surfaces without mechanical action - Test method and requirements (phase 2, step 2)". This standard covers: This document specifies a test method and the minimum requirements for bactericidal and yeasticidal and additionally fungicidal activity of chemical disinfectant products that form a homogeneous, physically stable preparation when diluted with hard water - or in the case of ready-to-use products - with water. NOTE Dilutions are necessary as three concentrations in the active to non-active range are tested. This document applies to products that are used in the medical area for disinfecting non-porous surfaces without mechanical action. This document applies to areas and situations where disinfection or antisepsis is medically indicated. Such indications occur in patient care, for example: - in hospitals, in community medical facilities and in dental institutions; - in clinics of schools, of kindergartens and of nursing homes; and can occur in the workplace and in the home. It can also include services such as laundries and kitchens supplying products directly for the patients. EN 14885 specifies in detail the relationship of the various tests to one another and to use recommendations. Using this document, it is possible to determine the activity of products like commercial formulations or active substances on bacteria and/or fungi in the conditions in which they are used and therefore it corresponds to a phase 2, step 2 test. This method excludes the evaluation of the activity of products against mycobacteria and bacterial spores.
This document specifies a test method and the minimum requirements for bactericidal and yeasticidal and additionally fungicidal activity of chemical disinfectant products that form a homogeneous, physically stable preparation when diluted with hard water - or in the case of ready-to-use products - with water. NOTE Dilutions are necessary as three concentrations in the active to non-active range are tested. This document applies to products that are used in the medical area for disinfecting non-porous surfaces without mechanical action. This document applies to areas and situations where disinfection or antisepsis is medically indicated. Such indications occur in patient care, for example: - in hospitals, in community medical facilities and in dental institutions; - in clinics of schools, of kindergartens and of nursing homes; and can occur in the workplace and in the home. It can also include services such as laundries and kitchens supplying products directly for the patients. EN 14885 specifies in detail the relationship of the various tests to one another and to use recommendations. Using this document, it is possible to determine the activity of products like commercial formulations or active substances on bacteria and/or fungi in the conditions in which they are used and therefore it corresponds to a phase 2, step 2 test. This method excludes the evaluation of the activity of products against mycobacteria and bacterial spores.
SIST EN 17387:2022 is classified under the following ICS (International Classification for Standards) categories: 11.080.20 - Disinfectants and antiseptics. The ICS classification helps identify the subject area and facilitates finding related standards.
SIST EN 17387:2022 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-januar-2022
Kemična razkužila in antiseptiki - Kvantitativni preskus na neporoznih površinah
brez mehanskega delovanja za vrednotenje baktericidnega in/ali fungicidnega
delovanja in delovanja kemičnih razkužil na kvasovke v humani medicini -
Preskusna metoda in zahteve (faza 2, stopnja 2)
Chemical disinfectants and antiseptics - Quantitative test for the evaluation of
bactericidal and yeasticidal and/or fungicidal activity of chemical disinfectants in the
medical area on non-porous surfaces without mechanical action - Test method and
requirements (phase 2, step 2)
Chemische Desinfektionsmittel und Antiseptika - Quantitativer Versuch zur Bestimmung
der bakteriziden und levuroziden und/oder fungiziden Wirkung chemischer
Desinfektionsmittel im humanmedizinischen Bereich auf nicht porösen Oberflächen ohne
mechanische Einwirkung - Prüfverfahren und Anforderungen (Phase 2, Stufe 2)
Antiseptiques et désinfectants chimiques - Essai quantitatif pour l’évaluation de l’activité
bactéricide et levuricide et/ou fongicide des désinfectants chimiques utilisés en
médecine sur des surfaces non poreuses sans action mécanique - Méthode d’essai et
exigences (phase 2, étape 2)
Ta slovenski standard je istoveten z: EN 17387:2021
ICS:
11.080.20 Dezinfektanti in antiseptiki Disinfectants and antiseptics
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
EN 17387
EUROPEAN STANDARD
NORME EUROPÉENNE
August 2021
EUROPÄISCHE NORM
ICS 11.080.20; 71.100.35
English Version
Chemical disinfectants and antiseptics - Quantitative test
for the evaluation of bactericidal and yeasticidal and/or
fungicidal activity of chemical disinfectants in the medical
area on non-porous surfaces without mechanical action -
Test method and requirements (phase 2, step 2)
Antiseptiques et désinfectants chimiques - Essai Chemische Desinfektionsmittel und Antiseptika -
quantitatif pour l'évaluation de l'activité bactéricide et Quantitativer Versuch zur Bestimmung der
levuricide et/ou fongicide des désinfectants chimiques bakteriziden und levuroziden und/oder fungiziden
utilisés en médecine sur des surfaces non poreuses Wirkung chemischer Desinfektionsmittel im
sans action mécanique - Méthode d'essai et exigences humanmedizinischen Bereich auf nicht porösen
(phase 2, étape 2) Oberflächen ohne mechanische Einwirkung -
Prüfverfahren und Anforderungen (Phase 2, Stufe 2)
This European Standard was approved by CEN on 25 January 2021.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this
European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references
concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN
member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by
translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management
Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2021 CEN All rights of exploitation in any form and by any means reserved Ref. No. EN 17387:2021 E
worldwide for CEN national Members.
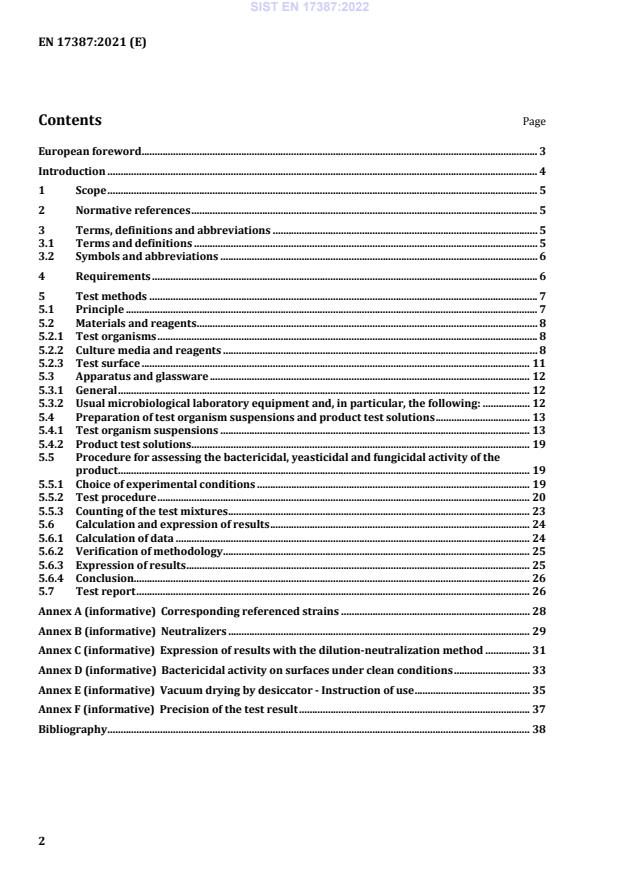
Contents Page
European foreword . 3
Introduction . 4
1 Scope . 5
2 Normative references . 5
3 Terms, definitions and abbreviations . 5
3.1 Terms and definitions . 5
3.2 Symbols and abbreviations . 6
4 Requirements . 6
5 Test methods . 7
5.1 Principle . 7
5.2 Materials and reagents . 8
5.2.1 Test organisms . 8
5.2.2 Culture media and reagents . 8
5.2.3 Test surface . 11
5.3 Apparatus and glassware . 12
5.3.1 General . 12
5.3.2 Usual microbiological laboratory equipment and, in particular, the following: . 12
5.4 Preparation of test organism suspensions and product test solutions . 13
5.4.1 Test organism suspensions . 13
5.4.2 Product test solutions . 19
5.5 Procedure for assessing the bactericidal, yeasticidal and fungicidal activity of the
product . 19
5.5.1 Choice of experimental conditions . 19
5.5.2 Test procedure . 20
5.5.3 Counting of the test mixtures . 23
5.6 Calculation and expression of results . 24
5.6.1 Calculation of data . 24
5.6.2 Verification of methodology . 25
5.6.3 Expression of results . 25
5.6.4 Conclusion. 26
5.7 Test report . 26
Annex A (informative) Corresponding referenced strains . 28
Annex B (informative) Neutralizers . 29
Annex C (informative) Expression of results with the dilution-neutralization method . 31
Annex D (informative) Bactericidal activity on surfaces under clean conditions . 33
Annex E (informative) Vacuum drying by desiccator - Instruction of use . 35
Annex F (informative) Precision of the test result . 37
Bibliography . 38
European foreword
This document (EN 17387:2021) has been prepared by Technical Committee CEN/TC 216 “Chemical
disinfectants and antiseptics”, the secretariat of which is held by AFNOR.
This European Standard shall be given the status of a national standard, either by publication of an
identical text or by endorsement, at the latest by February 2022, and conflicting national standards
shall be withdrawn at the latest by February 2022.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN-CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria,
Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland,
Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of
North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and the
United Kingdom.
Introduction
This document describes a surface test method for establishing whether a chemical disinfectant in the
area and fields described in the scope (Clause 1) has or does not have bactericidal and/or fungicidal or
yeasticidal activity on non-porous surfaces without mechanical action.
The laboratory test closely simulates practical conditions of application. Chosen conditions (contact
time, temperature, and microorganisms on surfaces.) reflect parameters which are found in practical
situations including conditions which can influence the action of disinfectants.
However, for some applications the recommendations of use of a product can differ and therefore
additional test conditions need to be used.
This document is not intended to be used when product is applied via an automatic airborne
disinfection method; in such cases, see EN 17272.
1 Scope
This document specifies a test method and the minimum requirements for bactericidal and yeasticidal
and additionally fungicidal activity of chemical disinfectant products that form a homogeneous,
physically stable preparation when diluted with hard water – or in the case of ready-to-use products –
with water.
NOTE Dilutions are necessary as three concentrations in the active to non-active range are tested.
This document applies to products that are used in the medical area for disinfecting non-porous
surfaces without mechanical action.
This document applies to areas and situations where disinfection or antisepsis is medically indicated.
Such indications occur in patient care, for example:
— in hospitals, in community medical facilities and in dental institutions;
— in clinics of schools, of kindergartens and of nursing homes; and can occur in the workplace and in
the home. It can also include services such as laundries and kitchens supplying products directly for
the patients.
EN 14885 specifies in detail the relationship of the various tests to one another and to use
recommendations.
Using this document, it is possible to determine the activity of products like commercial formulations or
active substances on bacteria and/or fungi in the conditions in which they are used and therefore it
corresponds to a phase 2, step 2 test.
This method excludes the evaluation of the activity of products against mycobacteria and bacterial
spores.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
EN 12353, Chemical disinfectants and antiseptics - Preservation of test organisms used for the
determination of bactericidal (including Legionella), mycobactericidal, sporicidal, fungicidal and virucidal
(including bacteriophages) activity
EN 14885, Chemical disinfectants and antiseptics - Application of European Standards for chemical
disinfectants and antiseptics
3 Terms, definitions and abbreviations
3.1 Terms and definitions
For the purposes of this document, the terms and definitions given in EN 14885 apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https://www.iso.org/obp
— IEC Electropedia: available at http://www.electropedia.org/
3.2 Symbols and abbreviations
c is the sum of V -values taken into account
C
cfu colony forming units
d is the dilution taken into account, lower dilution factor
m, m’ are the two replicas at the lower dilution expressed as cfu;
n, n’ are the two replicas at the higher dilution expressed as cfu;
n is the number of V -values taken into account
C
N number of cells per ml in the test suspension
N lg number of cfu recovered from the test surface in the water control
c
N counting of the cfu in the neutralizer control
C
N lg number of cfu recovered from the test surface in the test
d
N counting of the cfu in the method validation
T
Nts number of colony forming units remaining on the test surface
R reduction
V is the volume of the inoculated into the plate expressed in ml
4 Requirements
The product shall demonstrate at least a 5 decimal log (lg) reduction for bacteria and at least a 4
decimal log (lg) reduction for fungi, when tested in accordance with Table 1 and 5.5.
NOTE The 5 lg reduction is deemed necessary for the medical area to minimize the risk for the patients.
Table 1 — Experimental conditions
Test conditions Bactericidal activity Yeasticidal activity Fungicidal activity
Staphylococcus aureus
Minimum
Aspergillus brasiliensis
spectrum of Enterococcus hirae Candida albicans
Candida albicans
test organisms
Pseudomonas aeruginosa
additional any relevant test organism
according to the manufacturer’s recommendation, but between
Test
(4 ± 1) °C to (30 ± 1) °C
temperature
For tests performed at room temperature, the range shall be (21,5 ± 3,5) °C
according to the manufacturer’s recommendation, but at minimum 1 min
a
Contact time
and no longer than 5 min or 60 min (from 1 min to 5 min at intervals of 1 min and
from 5 min to 60 min at intervals of 5 min)
Interfering substance
clean conditions 0,3 g/l bovine albumin
dirty conditions 3,0 g/l bovine albumin plus 3,0 ml/l erythrocytes
additional any relevant substance
a
The contact times for surface disinfectants stated in this table are chosen on the basis of the practical
conditions of the product. The recommended contact time for the use of the product is within the responsibility
of the manufacturer. Products intended to disinfect surfaces that are likely to come into contact with the patient
and / or the medical staff and surfaces, which are frequently touched by different people, leading to the
transmission of microorganisms to the patient, shall be tested with a contact time of maximum 5 min. The same
applies where the contact time of the product shall be limited for practical reasons. Products for other surfaces
than stated above may be tested with a contact time of maximum 60 min.
NOTE For the additional conditions, the concentration defined as a result can be lower than the one obtained
under the minimum test conditions.
5 Test methods
5.1 Principle
A test suspension of bacteria or fungi in a solution of interfering substances (5.2.2.8) is inoculated onto
a test stainless steel surface and dried. A sample of the product under test is applied in a manner that
completely covers the dried test organisms. The surface is maintained at the temperature and contact
time exemplified in Clause 4 and 5.5.1. At the end of the contact time the surface is transferred to a
previously validated neutralization medium to suppress any product activity. The number of surviving
test organisms which can be recovered from the surface is determined quantitatively.
The number of bacteria or fungi on a test surface treated with hard water (or water in case of ready to
use products) in place of the product under test is also determined and the reduction in viable counts
attributed to the product is calculated as the difference between the two test surfaces’ results.
5.2 Materials and reagents
5.2.1 Test organisms
The bactericidal activity shall be evaluated using the following strains :
— Staphylococcus aureus ATCC 6 538;
— Enterococcus hirae ATCC 10 541;
— Pseudomonas aeruginosa ATCC 15 442.
The yeasticidal activity shall be evaluated using the following strain :
— Candida albicans ATCC 10 231.
The fungicidal activity shall be evaluated using the following strains :
— Aspergillus brasiliensis ATCC 16 404;
— Candida albicans ATCC 10 231.
If required for specific applications, additional strains may be chosen.
NOTE See Annex A for corresponding strain numbers in some other culture collections.
If additional test organisms are used, they shall be incubated under optimum growth conditions
(temperature, time, atmosphere, media) noted in the test report. If the additional test organisms
selected do not correspond to the specified strains, their suitability for supplying the required inocula
shall be verified. If these additional test organisms are not classified at a reference centre, their
identification characteristics shall be stated. In addition, they shall be held by the testing laboratory or
national culture collection under a reference for five years.
5.2.2 Culture media and reagents
5.2.2.1 General
All weights of chemical substances given in this document refer to the anhydrous salts. Hydrated forms
may be used as an alternative, but the weights required shall be adjusted to allow for consequent
molecular weight differences.
The reagents shall be of analytical grade and/or appropriate for microbiological purposes. They shall be
free from substances that are toxic or inhibitory to the test organisms.
To improve reproducibility, it is recommended that commercially available dehydrated material is used
for the preparation of culture media. The manufacturer's instructions relating to the preparation of
these products should be rigorously followed.
For each culture medium and reagent, a time limitation for use should be fixed.
All specified pH values are measured at (20 ± 1) °C.
The ATCC numbers are the collection numbers of strains supplied by these culture collections. This
information is given for the convenience of users of this European Standard and does not constitute an
endorsement by CEN of the product named.
5.2.2.2 Water
The water shall be freshly glass-distilled water and not demineralized water. If distilled water of
adequate quality is not available, water for injections can be used.
Sterilize in the autoclave [5.3.2.1a)]. Sterilization is not necessary if the water is used e.g. for
preparation of culture media and subsequently sterilized.
NOTE See 5.2.2.7 for the procedure to prepare hard water.
5.2.2.3 Tryptone soya agar (TSA)
For maintenance of bacterial strains and performance of viable counts.
Tryptone, pancreatic digest of casein 15,0 g
Soya peptone, papaic digest of Soybean meal 5,0 g
Sodium chloride (NaCl) 5,0 g
Agar 15,0 g
Water (5.2.2.2) to 1 000,0 ml
Sterilize in the autoclave [5.3.2.1 a)]. After sterilization the pH (5.3.2.6) of the medium shall be
equivalent to 7,2 ± 0,2.
5.2.2.4 Malt extract agar (MEA)
For maintenance of fungal strains, sporulation and performance of viable counts.
Malt extract [food grade (e.g. Christomalt powder from Difal) or 30,0 g
an equivalent extract that is not highly purified and not only
based on maltose (e.g. Malt extract from OXOID)]
Agar 15,0 g
Water (5.2.2.2) to 1 000,0 ml
However, if there are problems producing at least 75 % spiny spores see 5.4.1.3.
Sterilize in the autoclave [5.3.2.1 a)]. After sterilization, the pH (5.3.2.6) of the medium shall be
equivalent to 5,6 ± 0,2.
In case of an encountering problems with neutralization (5.5.2.3 and 5.5.2.4), it may be necessary to add
neutralizer (5.2.2.6) to MEA (5.2.2.4). Annex B gives guidance on the neutralizers that can be used. It is
recommended not to use neutralizer that causes opalescence in the agar.
5.2.2.5 Diluent
Tryptone sodium chloride solution:
Tryptone, pancreatic digest of casein 1,0 g
Sodium chloride 8,5 g
Water (5.2.2.2) to 1 000,0 ml
This Malt extracts from Difal and OXOID are examples of a suitable product available commercially. This
information is given for the convenience of users of this European Standard and does not constitute an
endorsement by CEN of this product.
Sterilize in the autoclave [5.3.2.1 a)]. After sterilization, the pH (5.3.2.6) of the diluent shall be
equivalent to 7,0 ± 0,2.
5.2.2.6 Neutralizer
The neutralizer shall be validated for the product being tested in accordance with 5.5.2.3 and 5.5.2.4. It
shall be sterile.
NOTE Information on neutralizers that have been found to be suitable for some categories of products is
given in Annex B.
5.2.2.7 Hard water for dilution of products
For the preparation of 1 l of hard water, the procedure is as follows:
— Prepare solution A: dissolve 19,84 g magnesium chloride (MgCl ) and 46,24 g calcium chloride
(CaCl ) in water (5.2.2.2) and dilute to 1 000 ml. Sterilize by membrane filtration (5.3.2.19) or in the
autoclave [5.3.2.1 a)]. Autoclaving – if used - can cause a loss of liquid. In this case make up to
1 000 ml with water (5.2.2.2) under aseptic conditions. Store the solution in the refrigerator
(5.3.2.15) for no longer than one month.
— Prepare solution B: dissolve 35,02 g sodium bicarbonate (NaHCO ) in water (5.2.2.2) and dilute to
1000 ml. Sterilize by membrane filtration (5.3.2.19). Store the solution in the refrigerator (5.3.2.15)
for no longer than one week.
— Place 600 ml to 700 ml of water (5.2.2.2) in a 1 000 ml volumetric flask (5.3.2.13) and add 6,0 ml of
solution A, then 8,0 ml of solution B. Mix and dilute to 1 000 ml with water (5.2.2.2). The pH
(5.3.2.6) of the hard water shall be 7,0 ± 0,2. If necessary, adjust the pH by using a solution of
approximately 40 g/l (about 1 mol/l) of sodium hydroxide (NaOH) or approximately 36,5 g/l
(about 1 mol/l) of hydrochloric acid (HCl).
The hard water shall be freshly prepared under aseptic conditions and used within 12 h.
NOTE When preparing the product test solutions (5.4.2), the addition of the product to the hard water
produces different final water hardness in each test tube. In any case, the final hardness expressed as calcium
carbonate (CaCO ) is lower than 375 mg/l in the test tube.
5.2.2.8 Interfering substance
5.2.2.8.1 General
The interfering substance shall be chosen according to the conditions of use laid down for the product.
The interfering substance shall be sterile and prepared at 2 times its final concentration in the test.
For any additional interfering substance, the ionic composition (e.g. pH, calcium and/or magnesium
hardness) and chemical composition (e.g. mineral substances, protein, carbohydrates, lipids,
detergents) shall be fully defined.
NOTE The term “interfering substance” is used even if it contains more than one substance.
The methods of preparation and sterilization together with the composition shall be noted in the test
report (5.7).
5.2.2.8.2 Bovine albumin solution
Bovine albumin solutions for the test conditions shall be prepared as follows.
a) Preparation for clean conditions:
— Dissolve 0,3 g of bovine albumin fraction V (suitable for microbiological purposes) in 100 ml of
diluent (5.2.2.5).
— Sterilize by membrane filtration (5.3.2.19).
— Dilute to the 1/5th with diluent (5.2.2.5).
— Keep in the refrigerator and use within one month.
The final concentration of bovine albumin in the test procedure (5.5.2) is 0,3 g/l.
b) Preparation for dirty conditions:
— Dissolve 3,0 g of bovine albumin fraction V (suitable for microbiological purposes) in 97 ml of
diluent (5.2.2.5).
— Sterilize by membrane filtration (5.3.2.19).
— Prepare at least 8,0 ml fresh sterile defibrinated sheep blood. Centrifuge the sheep blood at 800
g (5.3.2.14) for 10 min. After discarding the supernatant, resuspend erythrocytes in diluent
N
(5.2.2.5).
— Repeat this procedure at least 3 times, until the supernatant is colourless.
— Resuspend 3 ml of the packed sheep erythrocytes in the 97 ml of sterilized bovine albumin
solution (above).
— Dilute to the 1/5th with diluent (5.2.2.5).
— To avoid contamination this mixture should be split in portions probably needed per day and
kept in separate containers for a maximum of 7 days in a refrigerator (5.3.2.15).
The final concentration of bovine albumin and sheep erythrocytes in the test procedure (5.5) shall be
3 g/l and 3 ml/l respectively.
5.2.3 Test surface
The test surface is a flat stainless steel 304 ([1],[2]) disc (2 cm diameter) with grade 2b finish on both
sides. Only one side of a disc shall be used. The discs shall be used only once and manipulated with
forceps (5.3.2.16).
For cleaning, the discs shall be placed in a beaker (minimum size: 50 ml) containing not less than 20 ml
®3
of 5 % (V/V) Decon for 60 min. Immediately rinse the discs twice with water (5.2.2.2) for 10 s to
completely remove the cleanser. Do not let the discs dry.
3 ®
Decon is an example of a suitable product available commercially. This information is given for the
convenience of users of this standard and does not constitute an endorsement by CEN of this product.
NOTE To supply a satisfactory flow of water, a sterilized fluid dispensing pressure vessel with suitable hose
and connectors or other suitable method can be used and regulated to supply approximately 2 000 ml per min.
For decontamination, place the clean disc in a bath containing 70 % (V/V) iso-propanol for 15 min.
Remove the disc and dry by evaporation under laminar air flow (5.3.2.17).
5.3 Apparatus and glassware
5.3.1 General
Sterilize all glassware and parts of the apparatus that will come into contact with the culture media and
reagents or the sample, except those which are supplied sterile, by one of the following methods:
a) by moist heat, in the autoclave [5.3.2.1 a)];
b) by dry heat, in the hot air oven [5.3.2.1 b)].
5.3.2 Usual microbiological laboratory equipment and, in particular, the following:
5.3.2.1 Apparatus for sterilization (moist and dry heat)
+3
a) For moist heat sterilization, an autoclave capable of being maintained at ( 121 ) °C for a minimum
holding time of 15 min;
+5
b) for dry heat sterilization, a hot air oven capable of being maintained at ( 180 ) °C for a minimum
+5 +5
holding time of 30 min, at ( 170 ) °C for a minimum holding time of 1 h or at ( 160 ) °C for a
0 0
minimum holding time of 2 h.
5.3.2.2 Temperature controlled cabinet or chamber capable of being controlled at test temperatures
(θ ± 1) °C (for test temperatures others than room temperature (21,5 ± 3,5) °C).
5.3.2.3 Water baths, capable of being controlled at (20 ± 1) °C, at (45 ± 1) °C and at additional test
temperatures (θ ± 1) °C (5.5.1).
5.3.2.4 Incubator (for bactericidal activity), capable of being controlled either at (36 ± 1) °C or
(37 ± 1) °C. An incubator at (37 ± 1) °C may be used if an incubator at (36 ± 1) °C is not available. The
same temperature shall be used for incubations performed during a test and its control and validation.
5.3.2.5 Incubator (for fungicidal or yeasticidal activity), capable of being controlled at (30 ± 1) °C.
5.3.2.6 pH-meter, having an inaccuracy of calibration of no more than ± 0,1 pH units at (20 ± 1) °C.
5.3.2.7 Stopwatch
5.3.2.8 Shakers
® 5
a) Electromechanical agitator, i.e. Vortex mixer ;
b) Mechanical shaker.
Disposable sterile equipment is an acceptable alternative to reusable glassware.
5 ®
Vortex is an example of a suitable product available commercially. This information is given for the
convenience of users of this European Standard and does not constitute an endorsement by CEN of this product.
5.3.2.9 Containers: Test tubes, culture bottles or flasks of suitable capacity.
5.3.2.10 Graduated pipettes of nominal capacities 10 ml, 1 ml, 0,1 ml, 0,05 ml and 0,001 ml, or
calibrated automatic pipettes.
5.3.2.11 Petri dishes of size 90 mm to 100 mm.
5.3.2.12 Glass beads (Diameter: ≤ 5 mm).
5.3.2.13 Volumetric flasks
5.3.2.14 Centrifuge (800 g ).
N
5.3.2.15 Refrigerator capable of being controlled at (5 ± 3) °C.
5.3.2.16 Forceps
5.3.2.17 Microbiological filtered laminar air flow cabinet
5.3.2.18 Fritted filter: Porosity of 40 µm to 100 µm (ISO 4793, [3]).
5.3.2.19 Membrane filtration apparatus, constructed of a material compatible with the substances to
be filtered.
The apparatus shall have a filter holder of at least 50 ml volume. It shall be suitable for use with filters
of diameter 47 mm to 50 mm and 0,45 μm pore size for sterilization of hard water (5.2.2.7).
5.3.2.20 Vacuum desiccator
Vacuum source may be a pump or central supply and should achieve a vacuum of 20 in mercury to 25 in
mercury (508 torr to 635 torr; 677 mbar to 847 mbar; 68 000 Pascal to 85 000 Pascal; conversion
tables are readily available on the Internet for other units). For details how to proceed see Annex E.
NOTE Other types of desiccators are allowed if they lead to the same results – independent from the locality
where it is used.
5.3.2.21 Flasks with ventilated caps: Roux bottles or similar flasks.
5.3.2.22 Spectrophotometer or other suitable technique
5.3.2.23 Microscope
5.4 Preparation of test organism suspensions and product test solutions
5.4.1 Test organism suspensions
5.4.1.1 Preservation and Stock cultures of test organisms
The test organisms and their stock cultures shall be prepared and kept in accordance with EN 12353.
5.4.1.2 Working culture of test organisms
a) Bacteria
In order to prepare the working culture of the test organism (5.2.1), subculture from the stock culture
(5.4.1.1) by streaking on TSA (5.2.2.3) slopes and incubate (5.3.2.4). After 18 h to 24 h, prepare a second
subculture from the first subculture in the same way and incubate for 18 h to 24 h. From this second
subculture, a third subculture may be produced in the same way. The second and (if produced) third
subculture is/are the working culture(s).
If it is not possible to prepare the second subculture on a particular day, a 48 h subculture may be used
for subsequent subculturing, provided that the subculture has been kept in the incubator during the
48 h period.
Never produce and use a fourth subculture.
For additional strains (5.2.1), any departure from this method of culturing the bacteria or preparing the
suspensions shall be noted, giving the reasons in the test report.
b) Fungi
In order to prepare the working culture of Candida albicans (5.2.1), subculture from the stock culture
(5.4.1.1) by streaking onto MEA (5.2.2.4) slopes and incubate (5.3.2.5). After 42 h to 48 h, prepare a
second subculture from the first subculture in the same way and incubate for 42 h to 48 h. From this
second subculture a third subculture can be produced in the same way. The second and (if produced)
third subculture is/are the working culture(s).
For Aspergillus brasiliensis (5.2.1), use only the first subculture grown on MEA (5.2.2.4) in Petri dishes
(5.3.2.11) or flasks with ventilated caps (5.3.2.21) and incubate at (30 ± 1) °C for 7 d to 9 d. No further
subculturing is needed. Do not stack the Petri dishes during the incubation to improve the temperature
homogenization.
At the end of incubation, all the cultures shall show a dark brown or black surface. Cultures with
appearance of rare and small white or grey areas might be kept (Figure 1 and Figure 2).
Figure 1 —Examples of appropriate cultures of A. brasiliensis ATCC 16404 after 7 d of incubation
at 30 °C
Figure 2 —Example of inappropriate (not usable) culture of A. brasiliensis ATCC 16404 after 7 d
of incubation at 30 °C
5.4.1.3 Test suspensions
a) Bacterial test suspension
Take 10 ml of diluent (5.2.2.5) and place in a 100 ml flask (5.3.2.13) with 5 g of glass beads (5.3.2.12).
Take the working culture (5.4.1.2) and transfer loopfuls of the cells into the diluent. The cells should be
suspended in the diluent by immersing the loop in the diluent and rubbing it against the side of the flask
to dislodge the cells. Shake the flask for 3 min using a mechanical shaker [5.3.2.8 b)]. Aspirate the
suspension from the glass beads and transfer to another flask (5.3.2.13). Adjust the number of cells in
9 9
the suspension to 1,5 × 10 cfu/ml to 5,0 × 10 cfu/ml using the diluent. The numbers of units shall be
estimated by means of spectrophotometer or any other suitable technique (5.3.2.22) Maintain this
suspension in the water bath at (20 ± 1) °C (5.3.2.3) and use within 2 h.
b) Fungal test suspension
1) Candida albicans
Take 10 ml of diluent (5.2.2.5) and place in a 100 ml flask with 5 g of glass beads. Take the working
culture (5.4.1.2) and transfer loopfuls of the cells into the diluent. The cells should be suspended in
the diluent by immersing the loop in the diluent and rubbing it against the side of the flask to
dislodge the cells. Shake the flask for 3 min using a mechanical shaker [5.3.2.8 b)]. Aspirate the
suspension from the glass beads and transfer to another flask. Adjust the number of cells in the
8 8
suspension from 1,5 × 10 cfu/ml to 5,0 × 10 cfu/ml using the diluent, estimating the numbers of
units by means of a spectrophotometer or other suitable technique (5.3.2.22). Maintain this
suspension in the water bath at (20 ± 1) °C (5.3.2.3) and use within 2 h.
2) Aspergillus brasiliensis
Take the working culture (5.4.1.2) and suspend the cells in 10 ml of sterile 0,05 % w/v polysorbate
806 solution in water (5.2.2.2). Using a sterile glass rod or spatula detach the conidiospores from
the culture surface. Transfer the suspension into a flask and gently shake by hand for one minute
together with 5 g glass beads (5.3.2.12). The suspension is filtered through a fritted filter (5.3.2.18).
Polysorbate 80 is an example of a suitable product available commercially. This information is given for the
convenience of users of this European Standard and does not constitute an endorsement by CEN of this product.
Carry out a microscopic (5.3.2.23) examination under x 400 magnification immediately after the
preparation to show:
— the presence of a high concentration (at least 75 % of spiny spores) of characteristic mature
spores, i.e. spiny spores (versus smooth spores) [Figure 3 and Figure 4];
— the absence of spore germination (check at least 10 fields of view);
— the absence of mycelia fragments (check at least 10 fields of view).
If germinated spores are present, discard the suspension.
If mycelia are present, proceed to a 2nd fritted filtration.
If mycelia are still present, discard the suspension.
If 75 % spiny spores are not achieved it may be due to the Aspergillus brasiliensis culture or the
media used to produce these spores. In this situation, it will be necessary to obtain the culture from
another culture collection and/or use a MEA (5.2.2.4) from a different supplier.
Figure 3 — Observation of conidiospores under light microscope: Presence of smooth (a) and
spiny (b) spores [inappropriate (not usable) suspension]
Figure 4 — Observation of conidiospores under light microscope: High concentration of
characteristic mature spores with spiny aspect (appropriate suspension)
8 8
Adjust the number of spores in the suspension from 1,5 × 10 cfu/ml to 5,0 × 10 cfu/ml using the
diluent (5.2.2.5), estimating the number of cfu by any suitable means. Use the suspension within 4 h in a
water bath controlled at (20 ± 1) °C (5.3.2.3). In any case, adjust the temperature according to 5.5.1 only
immediately before the start of the test (5.5.2).
The use of a cell counting device for adjusting the number of cells is highly recommended. When using a
suitable counting chamber, follow the instructions explicitly.
5.4.1.4 Preparation of bacterial and fungal test suspensions
−7 −8 −6
Dilute the adjusted bacterial suspensions (5.4.1.3) by 10 (serial dilutions) and 10 and by 10 (serial
−7
dilutions) and 10 for the mould spore suspension (5.4.1.3) and Candida albicans using diluent
(5.2.2.5). Mix the suspension [5.3.2.8 a)].
For bacteria and Candida albicans, take a sample of 1,0 ml of each dilution in duplicate and inoculate
using the pour plate or the spread plate technique.
1) When using the pour plate technique, transfer each 1,0 ml sample into separate Petri dishes
(5.3.2.11) and add 15 ml to 20 ml of melted TSA (5.2.2.3) for the bacteria and 15 ml to 20 ml melted
MEA (5.2.2.4) for Candida albicans, cooled to (45 ± 1) °C.
2) When using the spread plate technique, spread about one half of each 1,0 ml sample on an
appropriate number (at least two) of surface dried plates containing TSA (5.2.2.3) for bacteria and
MEA (5.2.2.4) for Candida albicans (i.e. in duplicate = four plates).
For Aspergillus brasiliensis, take a sample of 1,0 ml of each dilution in duplicate and inoculate using the
pour plate or the spread plate technique.
a) When using the pour plate technique, transfer about half of each 1,0 ml sample into separate Petri
dishes (at least two) and add 15 ml to 20 ml of melted MEA (5.2.2.4) (i.e. in duplicate = four plates).
cooled to (45 ± 1) °C.
b) When using the spread plate technique, spread about one quarter of each 1,0 ml sample on an
appropriate number (at least four) of surface dried plates containing MEA (5.2.2.4) (i.e. in duplicate
– at least eight plates).
The test suspension shall be mixed [5.3.2.8 a)] immediately before use to re-suspend the spores.
For Incubation and counting see 5.4.1.5.
5.4.1.5 Incubation and counting of bacterial and fungal test suspensions
a) Counting of bacterial test suspensions
For the bacterial strains, incubate (5.3.2.4) the plates at (36 ± 1) °C or at (37 ± 1 ) °C for 18 h to 24 h.
Discard any plates which are not countable for any reason. Incubate the plates for a further 18 h to 24 h.
Do not recount plates which no longer show countable colonies. Recount the remaining plates.
b) Counting of fungal test suspensions
For the fungal strains, incubate (5.3.2.5) the plates at (30 ± 1) °C for 18 h to 24 h (Candida albicans) or
for 42 h to 48 h (Aspergillus brasiliensis). Discard any plates which are not countable for any reason.
Count the plates and determine the number of colony forming units. Incubate the plates for a further 18
h to 24 h. Do not recount plates which no longer show well-separated colonies. Recount the remaining
plates. For Aspergillus brasiliensis, continue incubation for a further 18 h to 24 h and if necessary a
further 18 h to 24 h, provided the number of countable colonies (discrete colonies) is increasing.
Determine the highest number of colonies for each 1 ml sample.
For calculation including the determination of the weighted mean, see 5.4.1.6 and 5.4.1.7.
5.4.1.6 Determination of V -values
C
The V -values are determined as follows.
C
a) Only the plates showing a number of colonies included in a 15 to 300 for bacteria and yeast and 15
to 150 for mould range were used to perform the result calculation. A deviation of 10 % is accepted,
so the limits are 14 and 330 for bacteria and yeast and 14 and 165 for mould.
NOTE The lower limit (14) is based on the fact that the variability increases the smaller the number counted
in the sample (1 ml or 0,1 ml) is and therefore subsequent calculations may lead to wrong results. The lower
limit refers only to the sample (and not necessarily to the counting on one plate), e.g. three plates per 1 ml
sample with 3 cfu, 8 cfu and 5 cfu give a V -value of 16. The upper limits (330, 165) reflect the imprecision of
C
counting confluent colonies and growth inhibition due to nutriment depletion. They refer only to the counting
on one plate and not necessarily to the sample.
b) For counting the cfu of test suspension N (5.4.1) for all countings of the dilution-neutralization
method (5.5.2), determine and record the V -values according to the number of plates used per
C
1 ml sample.
If more than one plate per 1 ml sample has been used to determine the V -value, the countings per
C
plate should be noted.
If the count on one plate is higher than 330, report the number as “>330”. If more than one plate
per 1 ml sample has been used and at least one of them shows a number higher than 330, report
this
...



Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...