SIST EN 17272:2020+A1:2026
(Main + Amendment)Chemical disinfectants and antiseptics - Methods of airborne room disinfection by automated process - Determination of bactericidal, mycobactericidal, sporicidal, fungicidal, yeasticidal, virucidal and phagocidal activities
Chemical disinfectants and antiseptics - Methods of airborne room disinfection by automated process - Determination of bactericidal, mycobactericidal, sporicidal, fungicidal, yeasticidal, virucidal and phagocidal activities
The test methods described are designed to determine the disinfectant activity of processes used in the 1) medical area, 2) veterinary area, 3) food, industrial, domestic and institutional area using automated processes for distributing chemicals by air diffusion with no operator manually applying the disinfectant. This document covers the disinfection of nonporous surfaces but not that of the air.
The objective of the described processes is to disinfect the surfaces of the overall area including the external surfaces of the equipment contained in such rooms. Air handling and products or processes specifically designed for the disinfection of medical devices are excluded from the scope of this document. The test methods and volumes described provide a defined challenge.
This document is applicable to processes for which activity is claimed against the following groups of microorganisms:
— vegetative bacteria,
— mycobacteria,
— bacterial spores,
— yeasts,
— fungal spores,
— viruses,
— bacteriophages.
This document does not cover processes for which the mode of action is based on immersing and/or circulation, flooding, spraying, wiping or other processes where the product is directly applied to the surfaces and not via air dispersion.
Chemische Desinfektionsmittel und Antiseptika- Verfahren zur luftübertragenen Raumdesinfektion durch automatisierte Verfahren- Bestimmung der bakteriziden, mykobakteriziden, sporiziden, fungiziden, levuroziden, viruziden und Phagen-Wirksamkeit
Antiseptiques et désinfectants chimiques - Méthodes de désinfection des pièces par voie aérienne par des procédés automatisés - Détermination de l'activité bactéricide, fongicide, levuricide, sporicide, virucide et phagocid
Kemična razkužila in antiseptiki - Metode za dezinfekcijo površin v prostorih z delci v zraku z avtomatiziranim postopkom - Določanje baktericidnega, mikobaktericidnega, sporocidnega, fungicidnega, virucidnega in fagocidnega delovanja ter delovanja na kvasovke
General Information
- Status
- Published
- Publication Date
- 10-Dec-2025
- Technical Committee
- KDS - Cosmetics, chemical disinfectants and surface active agents
- Current Stage
- 6060 - National Implementation/Publication (Adopted Project)
- Start Date
- 08-Oct-2025
- Due Date
- 13-Dec-2025
- Completion Date
- 11-Dec-2025
Relations
- Effective Date
- 01-Jan-2026
- Effective Date
- 01-Jan-2026
Overview
SIST EN 17272:2020+A1:2026 (aligned with EN 17272:2020+A1:2025) defines laboratory test methods for automated airborne room disinfection processes that distribute chemical disinfectants by air diffusion (gas, vapour or aerosol) to disinfect non‑porous surfaces. It is a Phase 2, step 2 standard intended to evaluate the combined device + product process under controlled, reproducible conditions. The standard covers claims of bactericidal, mycobactericidal, sporicidal, fungicidal, yeasticidal, virucidal and phagocidal activity for applications in medical, veterinary, food, industrial, domestic and institutional areas. It explicitly excludes air-only disinfection, medical device disinfection, and methods where the product is directly applied by immersion, flooding, spraying, wiping or circulation.
Key topics and technical requirements
- Two-part test design:
- Part 1 - Efficacy test: verifies minimum log‑reduction performance against specified test organisms under defined conditions.
- Part 2 - Distribution test: confirms product distribution and activity throughout the enclosure using reference organisms at multiple sampling positions.
- Defined challenge conditions: carrier placement, ADC (airborne disinfection contact) time, and aeration time are specified to simulate practical use.
- Required reductions (expressed as log10 reductions):
- Bactericidal: ≥ 5 lg on specified bacterial organisms
- Mycobactericidal: ≥ 4 lg
- Sporicidal: ≥ 4 lg (medical), ≥ 3 lg (veterinary; food/industrial/domestic)
- Fungicidal / Yeasticidal: ≥ 4 lg
- Virucidal and phagocidal activities are also covered for validated organisms
- The standard treats the device and chemical product as a single process; they cannot be assessed separately.
- Normative references and annexes provide detailed procedures, interfering substances, spore preparation, apparatus, and test reporting requirements.
Practical applications and users
- Primary users:
- Manufacturers of automated airborne disinfection devices and disinfectant formulations
- Independent microbiological test laboratories and validation service providers
- Infection prevention and control teams in healthcare, veterinary and laboratory settings
- Food industry and facility hygiene validation teams
- Regulatory and standards bodies assessing product claims
- Practical uses:
- Product/process qualification for market claims of surface decontamination efficacy
- Comparative testing of airborne disinfection systems
- Establishing validated operational parameters (dose, exposure and aeration) for site deployment
- Supporting biosecurity and environmental hygiene validation programs
Related standards
- EN 14885 - Application of European standards for chemical disinfectants and antiseptics
- EN 12353 - Preservation of test organisms
- Other CEN/TC 216 standards for suspension and carrier testing
Keywords: airborne room disinfection, automated airborne disinfection, disinfectant activity, bactericidal, sporicidal, mycobactericidal, virucidal, EN 17272, surface disinfection validation.
Frequently Asked Questions
SIST EN 17272:2020+A1:2026 is a standard published by the Slovenian Institute for Standardization (SIST). Its full title is "Chemical disinfectants and antiseptics - Methods of airborne room disinfection by automated process - Determination of bactericidal, mycobactericidal, sporicidal, fungicidal, yeasticidal, virucidal and phagocidal activities". This standard covers: The test methods described are designed to determine the disinfectant activity of processes used in the 1) medical area, 2) veterinary area, 3) food, industrial, domestic and institutional area using automated processes for distributing chemicals by air diffusion with no operator manually applying the disinfectant. This document covers the disinfection of nonporous surfaces but not that of the air. The objective of the described processes is to disinfect the surfaces of the overall area including the external surfaces of the equipment contained in such rooms. Air handling and products or processes specifically designed for the disinfection of medical devices are excluded from the scope of this document. The test methods and volumes described provide a defined challenge. This document is applicable to processes for which activity is claimed against the following groups of microorganisms: — vegetative bacteria, — mycobacteria, — bacterial spores, — yeasts, — fungal spores, — viruses, — bacteriophages. This document does not cover processes for which the mode of action is based on immersing and/or circulation, flooding, spraying, wiping or other processes where the product is directly applied to the surfaces and not via air dispersion.
The test methods described are designed to determine the disinfectant activity of processes used in the 1) medical area, 2) veterinary area, 3) food, industrial, domestic and institutional area using automated processes for distributing chemicals by air diffusion with no operator manually applying the disinfectant. This document covers the disinfection of nonporous surfaces but not that of the air. The objective of the described processes is to disinfect the surfaces of the overall area including the external surfaces of the equipment contained in such rooms. Air handling and products or processes specifically designed for the disinfection of medical devices are excluded from the scope of this document. The test methods and volumes described provide a defined challenge. This document is applicable to processes for which activity is claimed against the following groups of microorganisms: — vegetative bacteria, — mycobacteria, — bacterial spores, — yeasts, — fungal spores, — viruses, — bacteriophages. This document does not cover processes for which the mode of action is based on immersing and/or circulation, flooding, spraying, wiping or other processes where the product is directly applied to the surfaces and not via air dispersion.
SIST EN 17272:2020+A1:2026 is classified under the following ICS (International Classification for Standards) categories: 11.080.20 - Disinfectants and antiseptics; 71.100.35 - Chemicals for industrial and domestic disinfection purposes. The ICS classification helps identify the subject area and facilitates finding related standards.
SIST EN 17272:2020+A1:2026 has the following relationships with other standards: It is inter standard links to SIST EN 17272:2020, SIST EN 17272:2020/kFprA1:2025. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
SIST EN 17272:2020+A1:2026 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-januar-2026
Nadomešča:
SIST EN 17272:2020
Kemična razkužila in antiseptiki - Metode za dezinfekcijo površin v prostorih z
delci v zraku z avtomatiziranim postopkom - Določanje baktericidnega,
mikobaktericidnega, sporocidnega, fungicidnega, virucidnega in fagocidnega
delovanja ter delovanja na kvasovke
Chemical disinfectants and antiseptics - Methods of airborne room disinfection by
automated process - Determination of bactericidal, mycobactericidal, sporicidal,
fungicidal, yeasticidal, virucidal and phagocidal activities
Chemische Desinfektionsmittel und Antiseptika- Verfahren zur luftübertragenen
Raumdesinfektion durch automatisierte Verfahren- Bestimmung der bakteriziden,
mykobakteriziden, sporiziden, fungiziden, levuroziden, viruziden und Phagen-
Wirksamkeit
Antiseptiques et désinfectants chimiques - Méthodes de désinfection des pièces par voie
aérienne par des procédés automatisés - Détermination de l'activité bactéricide,
fongicide, levuricide, sporicide, virucide et phagocid
Ta slovenski standard je istoveten z: EN 17272:2020+A1:2025
ICS:
11.080.20 Dezinfektanti in antiseptiki Disinfectants and antiseptics
71.100.35 Kemikalije za dezinfekcijo v Chemicals for industrial and
industriji in doma domestic disinfection
purposes
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
EN 17272:2020+A1
EUROPEAN STANDARD
NORME EUROPÉENNE
November 2025
EUROPÄISCHE NORM
ICS 11.080.20; 71.100.35 Supersedes EN 17272:2020
English Version
Chemical disinfectants and antiseptics - Methods of
airborne room disinfection by automated process -
Determination of bactericidal, mycobactericidal,
sporicidal, fungicidal, yeasticidal, virucidal and phagocidal
activities
Antiseptiques et désinfectants chimiques - Méthodes Chemische Desinfektionsmittel und Antiseptika-
de désinfection des pièces par voie aérienne par des Verfahren zur luftübertragenen Raumdesinfektion
procédés automatisés - Détermination de l'activité durch automatisierte Verfahren- Bestimmung der
bactéricide, fongicide, levuricide, sporicide, virucide et bakteriziden, mykobakteriziden, sporiziden,
phagocid fungiziden, levuroziden, viruziden und Phagen-
Wirksamkeit
This European Standard was approved by CEN on 13 October 2019 and includes Amendment 1 approved by CEN on 7 April
2025.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this
European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references
concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN
member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by
translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management
Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Türkiye and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2025 CEN All rights of exploitation in any form and by any means reserved Ref. No. EN 17272:2020+A1:2025 E
worldwide for CEN national Members.
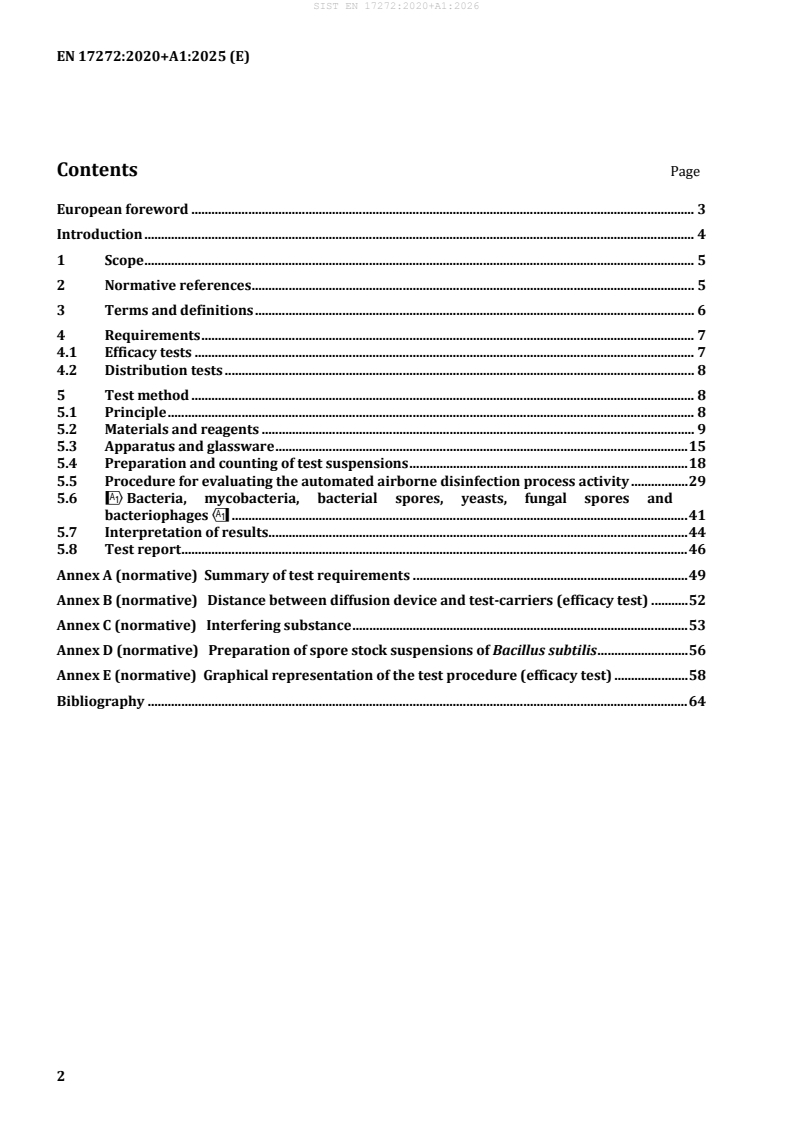
Contents Page
European foreword . 3
Introduction . 4
1 Scope . 5
2 Normative references . 5
3 Terms and definitions . 6
4 Requirements . 7
4.1 Efficacy tests . 7
4.2 Distribution tests . 8
5 Test method . 8
5.1 Principle . 8
5.2 Materials and reagents . 9
5.3 Apparatus and glassware . 15
5.4 Preparation and counting of test suspensions . 18
5.5 Procedure for evaluating the automated airborne disinfection process activity . 29
5.6 !Bacteria, mycobacteria, bacterial spores, yeasts, fungal spores and
bacteriophages" . 41
5.7 Interpretation of results . 44
5.8 Test report . 46
Annex A (normative) Summary of test requirements . 49
Annex B (normative) Distance between diffusion device and test-carriers (efficacy test) . 52
Annex C (normative) Interfering substance . 53
Annex D (normative) Preparation of spore stock suspensions of Bacillus subtilis . 56
Annex E (normative) Graphical representation of the test procedure (efficacy test) . 58
Bibliography . 64
European foreword
This document (EN 17272:2020+A1:2025) has been prepared by Technical Committee CEN/TC 216
“Chemical disinfectants and antiseptics”, the secretariat of which is held by AFNOR.
This European Standard shall be given the status of a national standard, either by publication of an
identical text or by endorsement, at the latest by May 2026, and conflicting national standards shall be
withdrawn at the latest by May 2026.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
This document includes Amendment 1 approved by CEN on 07 April 2025.
This document supersedes !EN 17272:2020".
The start and finish of text introduced or altered by amendment is indicated in the text by tags !".
This document describes a Phase 2 step 2 method designed:
— to check, under standardized laboratory conditions close to real-world practice, that the proposed
airborne surface disinfection processes meet the objective for which they were devised;
— to cross-compare different processes under reproducible conditions;
— to provide an experimental design within specified limits when real-world-practice conditions
depart from the conditions given in the text below.
!Results obtained using the 2020 version of the standard prior to the amendment remain valid."
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN-CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria,
Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland,
Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of
North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Türkiye and the
United Kingdom.
Introduction
The purpose of this document is to describe a test method for assessing the disinfectant activity of
airborne surface disinfection processes under a specific experimental condition.
The proposed test method consists of 2 parts:
— Part 1 - Efficacy test: intended to ensure that minimum efficacy requirements are fulfilled for each
type of activity claimed and for the targeted application area(s) (CEN/TC 216 WG 1 and/or WG 2
and/or WG 3).
— Part 2 - Distribution test: intended to ensure efficacy of the process throughout the enclosure. It is
performed with a reference test organism at 4 sampling positions.
The processes concerned include those involving chemical disinfectants in dispersed gaseous, vapour
and/or aerosolised form.
Every automated airborne disinfection cycle/application is unique and the purpose of this document is
to provide a defined challenge for the automated airborne disinfection system to successfully meet in
order to be considered an efficacious process. This standard method should therefore be regarded as a
useful starting point and not as a validation for all intended treatments with a particular automated
airborne disinfection system.
The method is used to qualify the process, i.e. the device(s) and product(s) needed for implementation.
For such chemical processes, the combination of device and product cannot be separated.
For the defined test conditions the number of carriers and their test positions can be increased
according to specific needs of a given application or local requirements.
The manufacturer:
— specifies the limitations and precautions for use of the process;
— ensures that the specified test conditions are representative for the recommended application(s).
The aim of this document is to simulate practical conditions of airborne disinfection in a laboratory
situation; obligatory conditions are defined according to the test method defined below. Additional
conditions are also proposed.
The test report specifies and summarizes the conditions under which the tests are carried out.
Generally, the processes are implemented after a cleaning procedure and then tested, according to the
application areas, under clean or low-level soiling conditions. For specified applications and/or
according to the manufacturer recommendations, test methods with other interfering substance can
also be envisaged as additional conditions.
The tests described in this document are based on measuring the reduction (expressed as decimal
logarithm lg) in terms of numbers of surviving test organisms of different strains of bacteria,
mycobacteria, bacterial spores, fungal spores, yeasts, viruses or bacteriophages and under specified
conditions. Test organisms may be supplemented by other test organisms. The experimental design
described in this document is expected to be followed, but the conditions can be varied according to the
needs of the practical application(s).
This method can be used as a basis for biosecurity applications in laboratories.
CEN/TC 216 phase 2, step 1 suspension tests for evaluating the irreversible inactivation by the product
cannot be performed as the product is changed by the diffusion through the air (e.g. liquid state vs
vapour state).
1 Scope
The test methods described are designed to determine the disinfectant activity of processes used in the
1) medical area, 2) veterinary area, 3) food, industrial, domestic and institutional area using automated
processes for distributing chemicals by air diffusion with no operator manually applying the
disinfectant. This document covers the disinfection of nonporous surfaces but not that of the air.
The objective of the described processes is to disinfect the surfaces of the overall area including the
external surfaces of the equipment contained in such rooms. Air handling and products or processes
specifically designed for the disinfection of medical devices are excluded from the scope of this
document. The test methods and volumes described provide a defined challenge.
This document is applicable to processes for which activity is claimed against the following groups of
microorganisms:
— vegetative bacteria,
— mycobacteria,
— bacterial spores,
— yeasts,
— fungal spores,
— viruses,
— bacteriophages.
This document does not cover processes for which the mode of action is based on immersing and/or
circulation, flooding, spraying, wiping or other processes where the product is directly applied to the
surfaces and not via air dispersion.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
EN 10088-2, Stainless steels —Part 2: Technical delivery conditions for sheet/plate and strip of corrosion
resisting steels for general purposes
EN 12353, Chemical disinfectants and antiseptics — Preservation of test organisms used for the
determination of bactericidal (including Legionella), mycobactericidal, sporicidal, fungicidal and virucidal
(including bacteriophages) activity
EN 14885, Chemical disinfectants and antiseptics — Application of European Standards for chemical
disinfectants and antiseptics
3 Terms and definitions
For the purposes of this document, the terms of EN 14885 and the following definitions apply:
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
• IEC Electropedia: available at https://www.electropedia.org/
• ISO Online browsing platform: available at https://www.iso.org/obp
3.1
chemical process
process in which the active substance is a chemical agent (product) diffused in gas, liquid and/or solid
form
Note 1 to entry: The product and the diffusion system (device) cannot be evaluated separately.
3.2
automated airborne disinfection process
process diffusing a product in the form of a gas, vapour and/or an aerosol (excluding aqueous steam)
from a device, without the need for human intervention, targeting surfaces and not the air
3.3
airborne disinfection contact time
ADC time
time from the first release of the product (disinfectant) to the point where carriers are recovered or to
the point where aeration starts, if an aeration time is considered necessary
Note 1 to entry: The carriers can be recovered at the end of ADC time, or during the aeration time, with suitable
personal protective equipment (PPE) where necessary.
3.4
aeration time
period of time during which an air exchange of the enclosure achieves an appropriate concentration of
the product in the enclosure based on the manufacturer’s use instructions and risk assessment, to
enable the recovery of the carriers
Note 1 to entry: The duration of this aeration time is dependent of the air treatment system characteristics.
3.5
distribution test
placement of test-carriers loaded with test organisms in such a way that the distribution of a product by
the combination of a device (machine) and the product achieves its claimed activity throughout the
enclosure
Note 1 to entry: This test is performed after or in parallel with the efficacy test.
3.6
supplementary obligatory conditions
test conditions used instead of the obligatory conditions where the practical use of the process and the
manufacturers claims are clearly and unambiguously excluding the obligatory test conditions
3.7
sensitive test organism
test organism where the drying causes a lg reduction of more than 1,5 by the end of the aeration time
4 Requirements
4.1 Efficacy tests
The automated airborne disinfection process to be tested under the obligatory experimental conditions
defined in 5.5 shall lead to the following reductions in terms of numbers, expressed in decimal log (lg):
Bactericidal activity:
— 5 lg or greater reduction on test-carriers compared to control-carriers not exposed to the process,
for each of the four specified bacterial test organisms.
For medical area, refer to 5.2.1.2, 5.2.1.3, 5.2.1.4, 5.2.1.5.
For veterinary area, refer to 5.2.1.1, 5.2.1.2, 5.2.1.3, 5.2.1.6.
For food, industrial, domestic and institutional area, refer to 5.2.1.1, 5.2.1.2, 5.2.1.3, 5.2.1.4.
Mycobactericidal activity:
— 4 lg or greater reduction for medical area and food industry and laboratory area on test-carriers
comparative to control-carriers not exposed to the process for the two test organisms
implemented, refer to 5.2.1.7, 5.2.1.8.
— 4 lg or greater reduction for veterinary area on test-carriers comparative to control-carriers not
exposed to the process for the specified test organism, refer to 5.2.1.7.
Sporicidal activity:
— 4 lg or greater reduction for medical area, 3 lg for veterinary area and food, industrial, domestic and
institutional area on test-carriers compared to control-carriers not exposed to the process for the
specified bacterial spore test organism, refer to 5.2.1.9.
Fungicidal activity:
— 4 lg or greater for medical area, veterinary area and food, industrial, domestic and institutional area
on test-carriers compared to control-carriers not exposed to the process for the two specified
fungal test organisms (yeast and fungal spore), refer to 5.2.1.10 and 5.2.1.11.
Yeasticidal activity:
— 4 lg or greater reduction for medical area, veterinary area and food industry and laboratory area on
test-carriers comparative to control-carriers not exposed to the process for the specified yeast test
organism, refer to 5.2.1.10.
Virucidal activity:
— 4 lg or greater reduction for medical area and food industry and laboratory area on test-carriers
comparative to control-carriers not exposed to the process, for the two specified test organisms,
refer to 5.2.1.12 and 5.2.1.13.
— 4 lg or greater reduction for veterinary area on test-carriers comparative to control-carriers not
exposed to the process, for the specified test organism, refer to 5.2.1.14.
Phagocidal activity:
— 4 lg or greater reduction for food industry and laboratory area on test-carriers comparative to
control-carriers not exposed to the process for the specified two test organisms, refer to 5.2.1.15
and 5.2.1.16.
The requirements and test methods are summarized in Annex A.
The reductions are expressed as decimal logarithmic values (lg).
The reductions indicated in the table of Annex A are the minimum reductions to be obtained on test-
carriers in comparison to control-carriers not exposed to the process.
These activities may be determined independently, i.e. by separate testing of the different
microbiological groups, e.g. mycobacteria, and !are not required to" be undertaken
simultaneously. Each activity can be claimed independently but passing both bactericidal and
yeasticidal activity as described in Annex A is the minimum requirement to claim compliance with this
document.
These seven activities shall be determined under the standard-reference experimental conditions
defined in 5.5.
Additional specific bactericidal, mycobactericidal, sporicidal, fungicidal, yeasticidal, virucidal, and
phagocidal activity can, as appropriate, be determined under other conditions (e.g. other ADC times,
type of carriers, test organisms, volume of the enclosure, temperature, humidity), for specific intended
uses. These additional conditions shall be described, recorded and reported in the test report.
Even if an automated airborne disinfection system has passed all or part of the test method described
here, the system and its delivered cycles shall then be validated in the individual enclosure (e.g. hospital
room, or animal house) in practice to be disinfected using appropriate biological or validated chemical
indicators.
4.2 Distribution tests
The reduction in the number of viable bacterial cells throughout the enclosure shall be determined with
Staphylococcus aureus ATCC 6538 = CIP 4,83 (refer to 5.2.1.2) to achieve 5 lg or greater reduction on
each test–carrier. Test-carriers shall be located in accordance with Annex A, part 2. Test conditions shall
replicate those used in the efficacy tests.
5 Test method
5.1 Principle
5.1.1 Preliminary test to validate absence of residual effect
The aim of the preliminary test is to identify whether there is any residual activity due to residual
product transferred via the carriers into the subculture media (agar plates and/or membranes) and to
find a method for eliminating this effect. This procedure should ensure that the results of the efficacy
test are based only on the irreversible inactivation of the test organisms and not on an inhibitory
(static) effect.
Non-contaminated carriers are exposed to the process after deposition and drying of the interfering
substance used in the assay.
Recovery into 100 ml (20 ml for virucidal activity) of sterile liquid medium, and testing for
microbiostatic (e.g. bacteriostatic) effects due to traces of the product residing on the carriers, which
could generate an inhibitory effect in agar medium and/or on the filter membranes or a decrease in the
residual viral titre.
5.1.2 Efficacy test
Using test organism suspensions containing interfering substance, deposit 50 µl per carrier prepared as
described in 5.2.3.
Spread and air-dry the inoculum as described in 5.5.1.2.2, then expose the prepared test-carriers to the
product diffused by the tested automated airborne disinfection process, under defined conditions.
Recover the surviving bacteria, mycobacteria, bacterial spores, yeasts, fungal spores, viruses or
bacteriophages by mechanical action, such as scraping (e.g. with a glass pipette or scalpel), or if
required sonicate, from the carriers, into the recovery liquid:
For bacteria, mycobacteria, bacterial spores, fungal spores and yeasts, dilute and inoculate the agar with
a fraction of the recovery liquid. Incubate and count the colonies. Filter the remaining recovery liquid
using membrane filtration, then rinse to eliminate as much product as possible. Transfer onto agar
medium. Place the carrier into agar medium to capture any remaining surviving test organisms.
Incubate and count the number of colonies.
For viruses and bacteriophages, dilute a fraction of the recovery liquid, incubate on a cell line and
determine the viral titre.
5.1.3 Distribution test
The distribution test is a replication of the efficacy test except that only Staphylococcus aureus is used as
the test organism and the test carriers are located in other defined positions and orientations.
5.2 Materials and reagents
5.2.1 Test organisms
Depending on the type of activity targeted, tests shall use all or some of the following test organisms.
These test organisms can be obtained from culture collections. The test organisms are:
For bactericidal activity tests:
— 5.2.1.1 Pseudomonas aeruginosa ATCC 15442 = CIP 103-467 (DSM 939)
— 5.2.1.2 Staphylococcus aureus ATCC 6538 = CIP 4.83 (DSM 799)
— 5.2.1.3 Enterococcus hirae ATCC 10541 = CIP 5855 (DSM 3320)
— 5.2.1.4 Escherichia coli ATCC 10536 = CIP 54127 (DSM 682)
— 5.2.1.5 Acinetobacter baumanii ATCC 19606 = CIP 70.34 (DSM 30007)
— 5.2.1.6 Proteus hauseri ATCC 13315 = CIP 58.60(DSM 30118)
!For mycobactericidal activity:
— 5.2.1.7. Mycobacterium avium ATCC 15769 = CIP 105415
— 5.2.1.16 Mycobacterium terrae ATCC 15755 (tuberculocidal activity)
Both test organisms shall be tested, except for the veterinary area where only Mycobacterium avium is
required."
For sporicidal activity tests:
— 5.2.1.9 Bacillus subtilis spores ATCC 6633 = CIP 52 62
For yeasticidal activity tests:
— 5.2.1.10 Candida albicans ATCC 10231 = IP 4872 (DSM 1386)
For fungicidal activity tests:
— 5.2.1.10 Candida albicans ATCC 10231 = IP 4872 (DSM 1386)
— 5.2.1.11 Aspergillus brasiliensis ATCC 16404 = IP 1431-83 (DSM 1988)
For virucidal activity tests:
— !5.2.1.12 Murine Norovirus strain S99, Friedrich Loeffler Institut, Isle de Riems. MNV cultured on
RAW 264.7 (ATCC TIB-71) cells line"
— 5.2.1.13 Adenovirus type 5, adenoid strain, ATCC VR-5. Adenovirus cultured on HeLa cells or other
lines of suitable susceptibility.
— 5.2.1.14 Porcine Parvovirus NADL2 strain cultured on ST cells or other appropriate cells line
!Murine Norovirus strain S99 and Adenovirus type 5 shall be tested for medical area and domestic
and institutional area. Porcine Parvovirus NADL2 shall be tested for veterinary area."
For phagocidal activity:
— 5.2.1.15 Bacteriophage for Lactococcus lactis subspecies lactis P001 (DSM 4262)
— 5.2.1.16. Bacteriophage for Lactococcus lactis subspecies lactis P008 (DSM 10567)
The multiplication of these two bacteriophages shall be obtained from the following host strain:
Lactococcus lactis subspecies lactis F7/2 (DSM 4366).
These strains can be obtained from biological collection resource centres.
The use of other test organisms
If additional test organisms are used, they shall be incubated under optimum growth conditions
(temperature, time, atmosphere, media) and noted in the test report. If the additional test organisms
selected do not correspond to the specified strains, their suitability for supplying the required inocula
shall be verified. If these additional test organisms are not classified at a reference centre, their
identification characteristics shall be stated. In addition, they shall be held by the testing laboratory or
national culture collection under a reference for five years.
5.2.2 Culture media and reagents
5.2.2.1 General
All weights of chemical substances given in this document refer to the anhydrous salts. Hydrated forms
may be used as an alternative, but the weights required shall be adjusted to allow for consequent
molecular weight differences.
The reagents shall be of analytical grade and/or appropriate for microbiological purposes. They shall be
free from substances that are toxic or inhibitory to the test organisms.
NOTE Commercial information (e.g. product name…) are provided by CEN as a convenience to users of this
document and does not represent an endorsement by CEN of this product. Equivalent products can be used if it is
demonstrated that they lead to the same results.
5.2.2.2 Culture media for bacteria, mycobacteria, spores, fungal spores and yeasts
5.2.2.2.1 Water
The water shall be freshly glass-distilled water and not demineralized water.
Sterilize in the autoclave (5.3.2.1a).
Sterile distilled water is necessary for the preparation of suspensions for tests. Sterilization is not
necessary if the water is used for e.g. preparation of culture media and subsequently sterilized.
NOTE If distilled water of adequate quality is not available, water for injection can be used.
5.2.2.2.2 Agar for bacterial counts (Tryptone Soya Agar: TSA)
For counts of viable bacterial cells (5.2.1.1 to 5.2.1.6)
Tryptone, pancreatic digest of casein 15,0 g
Soya peptone, papaic digest of soybean meal 5,0 g
NaCl 5,0 g
Agar 15,0 g
Water (see 5.2.2.2.1) to 1 000 ml
Sterilize in the autoclave. After sterilization, pH of the medium shall be equivalent to (7,2 ± 0,2) when
measured at (20 ± 1) °C.
If necessary, add a neutralizer to the medium (and record the addition in the test report).
Agar for the preservation of test organisms 5.2.1.1 to 5.2.1.6 (refer to 5.2.2.2.2) without neutralizer.
5.2.2.2.3 Reconstituted milk for use with sensitive test organisms
!Prepare the reconstituted skimmed milk (≤15 g/l fat) as follows:
Skimmed powdered milk, guaranteed for the absence of antimicrobial activity".
Sterilize 30 min at (105 ± 3) °C or 5 min at (121 ± 3) °C.
5.2.2.2.4 Agar for mycobacteria (refer to 5.2.1.7. and 5.2.1.8)
Middlebrook and Cohn 7H10 medium + 10 % oleic acid dextrose-albumin complex (OADC) (hereinafter
referred to as 7H10)
To carry out the counts of viable mycobacteria:
— Middlebrook 7H10 agar 19 g
— glycerol 5 ml
— water (see 5.2.2.2.1) to 895 ml
Heat to boiling point to achieve total dissolution. Sterilize in an autoclave for 10 min at 121 °C and allow
to cool to a temperature of 50 °C to 55 °C in a water bath.
Add 100 ml of Middlebrook OADC enrichment medium under aseptic conditions. Final pH = 6,6 at
(20 ± 1) °C.
5.2.2.2.5 Medium for spores (refer to 5.2.1.9)
Tryptone Soy Agar (TSA) for counting of viable Bacillus spores:
Tryptone, pancreatic digest of casein 15,0 g
Soya peptone, papaic digest of Soybean meal 5,0 g
Sodium Chloride (NaCl) 5,0 g
Agar 15,0 g
Water (see 5.2.2.2.1) to 1 000 ml
Sterilize in the autoclave (5.3.2.1 a)). After sterilization the pH of the medium shall be equivalent to
(7,2 ± 0,2) measured at (20 ± 1) °C.
Other media may be used for spores: see Annex D.
5.2.2.2.6 Malt extract agar (MEA)
For counts on the number of viable yeast and fungal spore cells (5.2.1.10 and 5.2.1.11).
Malt extract (technical grade) 30,0 g
Agar 15,0 g
Water (see 5.2.2.2.1) to 1 000 ml
The malt extract shall be of food grade (e.g. Cristomalt powder) or of equivalent grade, not highly
purified and not containing only maltose.
Sterilize in the autoclave. After sterilization, pH of the medium shall be equivalent to 5,6 ± 0,2 when
measured at (20 ± 1) °C.
If necessary, add a neutralizer to the medium (and record the addition in the test report).
!Deleted text"
5.2.2.2.7 Diluent for microbial suspensions
!Bacteria, yeast, fungi and spores"
Tryptone salt:
— Tryptone, pancreatic digest of casein 1,0 g
— Sodium chloride 8,5 g
— Water (see 5.2.2.2.1) to 1 000 ml
Sterilize in the autoclave. After sterilization, pH of the medium shall be equivalent to (7,2 ± 0,2) when
measured at (20 ± 1) °C.
Mycobacteria: Tryptone salt !(5.2.2.2.7)" or distilled water (5.2.2.2.1).
The diluent shall not induce interference between the test organisms and the product under test. !In
this case, water (5.2.2.2.1) can be used as diluent".
5.2.2.2.8 Liquid for test organism recovery and rinsing liquid for membrane filtration
Composition:
Tryptone, pancreatic digest of casein 1,0 g
Sodium chloride 8,5 g
Water to 1 000 ml
!Polysorbate 80 5,0 g"
Preparation:
Dissolve the sodium chloride, tryptone !and polysorbate" in the water. Add any neutralizing agent
specifically designed for the product under test.
Prepare the diluent in large-volume batches, then distribute into smaller adapted flasks. Sterilize in the
autoclave.
For mycobacteria, water (refer to 5.2.2.2.1) is used instead of diluents.
!For viruses, preservation media (refer to 5.2.2.3) is used instead of diluents."
5.2.2.3 Culture media and reagents for preparation of virus (test organisms 5.2.1.12 to 5.2.1.14.)
!Deleted text"
For viruses, Eagle minimum essential medium (MEM) or equivalent should be used, supplemented with
a suitable concentration of mycoplasm-free inactivated foetal calf serum, and antibiotics and other
growth factors if required !deleted text".
5.2.2.4 Culture media and reagents for preparation of bacteriophages (test organisms 5.2.1.15 to
5.2.1.16.)
5.2.2.4.1 M17 culture broth
For the preservation of the host bacterial strain, bacteriophage multiplication and bacteriophage
diluent preparation:
Phytone peptone (derived from soybean meal) 5,0 g
Polypeptone peptone (derived from casein and animal tissue) 5,0 g
Beef extract powder 5,0 g
Yeast extracts 2,5 g
D(+)-lactose 5,0 g
Ascorbic acid 0,5 g
Sodium -glycerophosphate 19,0 g
Magnesium sulfate, 7 H O 0,2 g
Water (see 5.2.2.2.1) to 1 000 ml
Sterilize by autoclaving. After sterilization, pH of the medium shall be equivalent to (7,0 ± 0,2) when
measured at (20 ± 1) °C.
When M17 broth is the diluent used to prepare the neutralizer (refer to EN 13610), double-
concentrated prepared M17 broth should be used (i.e. the concentration of all the ingredients added to
the 1 000 ml of water should be doubled).
5.2.2.4.2 M17 agar (underlay agar)
Underlay agar for quantitative counting of the lysis zones (plaques) each obtained from a single
infectious bacteriophage particle, formed in the host bacterial lawn.
Add 15 g of agar to 1 000 ml of M17 culture broth. Dissolve the agar by bringing it to the boil while
stirring continuously.
Sterilize by autoclaving. After sterilization, pH of the medium shall be equivalent to 7,0 ± 0,2 when
measured at (20 ± 1) °C. Once the agar has cooled to (45 ± 1) °C, add 10 ml of sterile 1 mol/l CaCl stock
solution (refer to 5.2.2.4.6). Mix gently and pour 15 ml to 18 ml of agar into Petri dishes.
5.2.2.4.3 Overlay agar (surface agar, soft agar)
For counts of bacteriophages: dissolve 6,5 g of agar in 1 000 ml of M17 culture broth (bring to the boil
while stirring continuously). Distribute the molten agar into test tubes (2,5 ml to 3 ml per tube).
Sterilize by autoclaving.
5.2.2.4.4 Bacteriophage diluent (based on Ringer's solution diluted to 1/4)
To prepare the series of dilutions intended to determine the titre of the bacteriophage suspensions
(counts of bacteriophage-induced lysis zones):
Ringer's solution diluted to 1/4:
— sodium chloride 2 250 g
— potassium chloride 0,105 g
— anhydrous calcium chloride 0,060 g
— sodium hydrogen carbonate 0,050 g
— water (see 5.2.2.2.1) to 1 000 ml
Add 10 ml of M17 culture broth to 90 ml of Ringer's solution diluted to 1/4.
Sterilize by autoclaving. Before use, add 1 ml of 1 mol/l CaCl stock solution to 100 ml of dilution broth.
NOTE Ringer's solution can be prepared using ready-to-use tablets according to the supplier's
recommendations.
5.2.2.4.5 SM buffer
For resuspension and intact preservation of bacteriophage particles:
Tris/HCl 2,4 g
Sodium chloride 5,8 g
Magnesium sulfate, 7 H O 2,5 g
Water (see 5.2.2.2.1) to 1 000 ml.
Adjust the pH of the buffer to (7,4 ± 0,1) when measured at (20 ± 1) °C. Sterilize by autoclaving.
5.2.2.4.6 CaCl stock solutions (1 mol/l and 0,05 mol/l)
In water (refer to 5.2.2.2.1), dissolve 110,99 g or 5,55 g of anhydrous CaCl and make up to 1 000 ml to
obtain the 1,0 mol/l or 0,05 mol/l stock solution, respectively. Sterilize by autoclaving.
5.2.2.4.7 Lactic acid solution (10 % volume fraction)
For the acidification of low-fat milk with a view to preparing the acid whey.
Dilute a 90 % volume fraction lactic acid stock solution in water (refer to 5.2.2.2.1) in order to obtain a
10 % volume fraction working solution. For this purpose, add 8 parts water to 1 part stock solution.
Sterilize by autoclaving.
!
5.2.2.4.8 Bacteriophage and virus recovery and rinsing liquid
For bacteriophage and virus, growth and preservation media (5.2.2.3.1) are used."
5.2.2.5 Interfering substance (See Annex C)
The interfering substance should be selected according to the application area of the process (see
Annex C).
When an excessive drying loss rate is found for sensitive test organisms (for instance Pseudomonas
aeruginosa, Escherichia coli, Candida albicans and/or other additional strains as Proteus hauseri), the
addition to the recommended interfering substance(s) of skimmed milk at the dilution 1/20 is accepted
to limit the drying loss.
The interfering substance shall be sterile and prepared concentrated 10-fold relative to the final
concentration in the test.
!The composition and sterilization method shall be recorded in the test report".
5.2.3 Carriers
5.2.3.1 General
New carriers shall be used for each test.
5.2.3.2 Obligatory carriers
!304" stainless steel disks (EN 10088-1) 3 cm to 4 cm in diameter, rated grade 2B under
EN 10088-2, surface-finished on both sides. The surfaces should be made as flat as possible using a
stainless steel 1,2 mm or 1,5 mm !thick". They shall be used only once, then discarded.
Prior to use the surfaces should be placed in a beaker (minimum size: 50 ml) containing not less than
20 ml of 5 % (V/V) Decon ® for 60 min. Immediately rinse the discs with water (refer to 5.2.2.2.1) for
10 s.
The surface shall not be allowed to dry to any extent. The discs shall only be handled with forceps. Rinse
the discs with water (refer to 5.2.2.2.1) for a further 10 s to ensure complete removal of the surfactant.
To supply a satisfactory flow of water, a sterilized fluid dispensing pressure vessel with suitable hose
and connectors or other suitable method can be used and regulated to supply approximately 2000 ml
per min. Treat the clean disc in a bath containing 70 % (V/V) iso-propanol for 15 min. Remove the disc
and dry by evaporation under laminar air flow.
5.2.3.3 Additional carriers
Any carrier may be used provided it is nonporous and described in detail in the test report.
The carriers shall be suitable for spreading a 50 µl inoculum on a surface in the region of 3 cm (2 cm in
diameter). Verify the spreading feasibility on this carrier. They shall then be suitable for introduction
into a 150 ml to 500 ml recipient and into a Petri dish for plating.
Cleaning, disinfection and/or sterilization requirements shall be determined according to carrier format
and type of materials and detailed in the test report.
5.3 Apparatus and glassware
5.3.1 General
Sterilize all glassware and parts of apparatus that will come into contact with the culture media and
reagents or the sample, except those which are supplied sterile, by one of the following methods:
— by moist heat, in the autoclave (5.3.2.1 a)
— by dry heat, in a hot-air oven (5.3.2.1 b).
5.3.2 Usual microbiological laboratory equipment, and in particular, the following:
5.3.2.1 Apparatus for sterilization
Decon® is an example of a suitable product available commercially. This information is given for the
convenience of users of this document and does not constitute an endorsement by CEN of this product.
a) For moist heat sterilization, an autoclave capable of being held at (121 ± 3) °C for a minimum
holding time of at least 15 min;
b) for dry heat sterilization, a hot air oven capable of being held at (180 ± 5) °C for a minimum holding
time of 30 min, at (170 ± 5) °C for a minimum holding time of 1 h, or at (160 ± 5) °C for a minimum
holding time of 2 h.
5.3.2.2 Water bath, capable of being controlled at (45 ± 1) °C.
5.3.2.3 Incubators
— Incubator, for drying the contaminated carriers in less than 2 h with or without air exchange,
controlled at (37 ± 1) °C.
— Incubator (for bactericidal, mycobactericidal, sporicidal, virucidal, phagocidal activity), capable of
being held at (36 ± 1) °C or at (37 ± 1) °C. Incubator (for fungicidal and yeasticidal activity), capable
of being held at (30 ± 1) °C.
— CO incubator (95 % air, 5 % CO ), capable of being held at (36 ± 1) °C or at (37 ± 1) °C for cell
2 2
culture and virus incubation.
5.3.2.4 pH-meter accurate to ± 0,1 pH units at (20 ± 1) °C, for measuring the pH of the agar media.
A puncture electrode or a flat membrane electrode should be used.
5.3.2.5 Stopwatch
5.3.2.6 Mechanical or electromechanical shaker
5.3.2.7 Membrane filtration apparatus, built in a material compatible with the filtrate substances.
The apparatus shall be equipped with an analytical filter funnel with a capacity of at least 50 ml. It shall
be suitable for use with 47 mm to 50 mm-diameter, 0,45 µm pore-size filters.
The vacuum source used shall give an even filtration flow rate. In order to obtain a uniform distribution
of the microorganisms over the membrane and prevent overlong filtration, the device shall be set to
filter 100 ml of rinsing liquid in 20 s to 40 s.
5.3.2.8 Refrigerator, temperature-controllable to between 2 °C and 8 °C
5.3.2.9 Graduated, pipettes of nominal capacities of 10 ml, 2 ml, 1 ml and 0,1 ml. Calibrated
automated pipettes may be used.
5.3.2.10 Petri dishes of size 90 mm to 100 mm in diameter and 55 mm for the membranes
5.3.2.11 Glass beads (diameter: 3 mm to 4 mm)
5.3.2.12 Fritted glass filter, pore size in the range 40 µm to 100 µm (ISO 4793) = pore size 2
5.3.2.13 Laboratory centrifuge, capable of 2 000 g acceleration (4 000g for bacteriophages)
N N
5.3.2.14 Roux flask, straight-necked
5.3.2.15 Analytical balance of adapted operating range
5.3.2.16 Spectrophotometer fitted with a monochromator
5.3.2.17 Vacuum pump
5.3.2.18 Hydrophobic-grid 0,45 µm pore-size sterile filter membranes (diameter 47 mm to 50 mm)
in cellulose ester or any other material adapted to the test product.
5.3.2.19 System for holding the test-carriers at a set distance from the source
5.3.2.20 Microscope, preferably a phase-contrast microscope (for the sporicidal activity tests) and
inverse microscope for virucidal activity
5.3.2.21 Forceps
5.3.2.22 Test tubes with screw top (diameter 18 mm or 20 mm)
5.3.2.23 Recipients: flasks or vials of adequate capacity
5.3.2.24 Conical flasks, larger-rimmed, 250 ml or 500 ml capacity
5.3.2.25 Screw-capped flasks
5.3.2.26 Micropipettes with disposable tips, dispensing 0,05 ml = 50 µl for depositing the inoculum
5.3.2.27 Ultrasonic vibrator, between 30 kHz and 43 kHz
5.3.2.28 Magnetic stirrer to keep the cells suspended prior to inoculation
5.3.2.29 Petri dishes, sterile test tubes, culture vials of suitable capacity
5.3.2.30 Volumetric flask calibrated at 20°C
5.3.2.31 96-well sterile micro-titre plates, six- to eight-well plates for cell culture and vials of cell
cult
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...