EN 17854:2024
(Main)Antimicrobial wound dressings - Requirements and test method
Antimicrobial wound dressings - Requirements and test method
This document specifies minimum requirements and a test method for the antimicrobial (microbicidal or microbistatic) activity of wound dressing products. It applies to all wound dressing products that specifically claim antimicrobial activity according to this document.
Antimikrobielle Wundauflagen - Anforderungen und Prüfverfahren
Dieses Dokument legt Mindestanforderungen und ein Prüfverfahren für die antimikrobielle (mikrobizide oder mikrobiostatische) Wirkung von Wundauflagen fest. Es gilt für alle Wundauflagen, die ausdrücklich eine antimikrobielle Wirkung nach diesem Dokument für sich beanspruchen.
Pansements antimicrobiens - Exigences et méthode d’essai
Le présent document spécifie les exigences minimales et une méthode d’essai pour l’activité antimicrobienne (microbicide ou microbiostatique) des pansements. Il s’applique à tous les pansements qui revendiquent spécifiquement une activité antimicrobienne conformément au présent document.
Protimikrobni sanitetni material - Zahteve in preskusne metode
Ta dokument določa minimalne zahteve in preskusno metodo za antimikrobno (mikrobicidno oziroma mikrostatično) aktivnost sanitetnega materiala. Uporablja se za vse vrste sanitetnega materiala, za katere je izrecno navedena antimikrobna aktivnost v skladu s tem dokumentom.
General Information
- Status
- Published
- Publication Date
- 19-Mar-2024
- Technical Committee
- CEN/TC 205 - Non-active medical devices
- Drafting Committee
- CEN/TC 205/WG 15 - Antimicrobial wound care dressings
- Current Stage
- 6060 - Definitive text made available (DAV) - Publishing
- Start Date
- 20-Mar-2024
- Due Date
- 01-Sep-2023
- Completion Date
- 20-Mar-2024
- Directive
- 93/42/EEC - Medical devices
Relations
- Effective Date
- 28-Jan-2026
Overview
EN 17854:2024 - Antimicrobial wound dressings - Requirements and test method (CEN) specifies minimum requirements and a laboratory test method to assess the antimicrobial activity of wound dressings that claim such properties. The standard defines how to determine whether a dressing is microbicidal (≥ 3‑log reduction of viable cells) or microbistatic (at least a 0‑log change under the test conditions) and sets out test conditions intended to simulate clinical application (test fluids, temperatures, exposure times).
Key topics and technical requirements
- Scope and definitions: Clear terminology for antimicrobial wound dressing, saturation volume (SV), working volume (WV = 80% of SV), simulated wound fluid (SWF), neutralizer, negative control dressing, plate factor and plate count method.
- Performance classification: Criteria for microbicidal vs. microbistatic activity and a performance table to interpret results.
- Test method elements:
- Preparation and cutting of dressing samples and negative controls.
- Calculation of saturation volume and working volume to define fluid exposure.
- Use of simulated wound fluid (SWF) for suspending test organisms (bacteria and yeast).
- Enumeration by plate count method and use of plate factor for CFU calculations.
- Neutralizer selection and neutralization validation (toxicity, efficacy, viability checks) to ensure antimicrobial effects are stopped before enumeration.
- Determination of detection limits, test validity criteria, reporting requirements and example report tables.
- Quality and documentation: Requirements for documentation, training and reproducible inter-laboratory comparison conditions.
- Annexes: Informative annexes provide rationale, neutralizer guidance, replicates, and test illustrations.
Applications
- Laboratory evaluation of dressings that claim antimicrobial activity.
- Comparative testing for product development and quality control.
- Supporting regulatory submissions, product labelling, and clinical procurement decisions.
- Establishing standardized test reports for performance claims.
Who should use this standard
- Medical device manufacturers and R&D teams developing antimicrobial wound dressings.
- Accredited testing laboratories performing antimicrobial efficacy assays.
- Regulatory and compliance professionals evaluating product claims.
- Healthcare procurement and infection control specialists assessing dressing performance.
Related standards
- EN 12353 (referenced normative standard for preservation of test organisms).
- Relevant CEN guidance from CEN/TC 205 on non‑active medical devices and terminology databases (ISO/IEC) for standard terms.
Keywords: EN 17854:2024, antimicrobial wound dressings, test method, microbicidal, microbistatic, simulated wound fluid, saturation volume, neutralization validation, CEN.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
EN 17854:2024 is a standard published by the European Committee for Standardization (CEN). Its full title is "Antimicrobial wound dressings - Requirements and test method". This standard covers: This document specifies minimum requirements and a test method for the antimicrobial (microbicidal or microbistatic) activity of wound dressing products. It applies to all wound dressing products that specifically claim antimicrobial activity according to this document.
This document specifies minimum requirements and a test method for the antimicrobial (microbicidal or microbistatic) activity of wound dressing products. It applies to all wound dressing products that specifically claim antimicrobial activity according to this document.
EN 17854:2024 is classified under the following ICS (International Classification for Standards) categories: 11.120.20 - Wound dressings and compresses. The ICS classification helps identify the subject area and facilitates finding related standards.
EN 17854:2024 has the following relationships with other standards: It is inter standard links to EN 12353:2021. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
EN 17854:2024 is associated with the following European legislation: EU Directives/Regulations: 2017/745, 93/42/EEC; Standardization Mandates: M/295. When a standard is cited in the Official Journal of the European Union, products manufactured in conformity with it benefit from a presumption of conformity with the essential requirements of the corresponding EU directive or regulation.
EN 17854:2024 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-junij-2024
Protimikrobni sanitetni material - Zahteve in preskusne metode
Antimicrobial wound dressings - Requirements and test method
Antimikrobielle Wundauflagen - Anforderungen und Prüfverfahren
Pansements antimicrobiens - Exigences et méthode d’essai
Ta slovenski standard je istoveten z: EN 17854:2024
ICS:
11.120.20 Sanitetni materiali, obveze in Wound dressings and
komprese compresses
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
EN 17854
EUROPEAN STANDARD
NORME EUROPÉENNE
March 2024
EUROPÄISCHE NORM
ICS 11.120.20
English Version
Antimicrobial wound dressings - Requirements and test
method
Pansements antimicrobiens - Exigences et méthode Antimikrobielle Wundauflagen - Anforderungen und
d'essai Prüfverfahren
This European Standard was approved by CEN on 14 August 2023.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this
European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references
concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN
member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by
translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management
Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Türkiye and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2024 CEN All rights of exploitation in any form and by any means reserved Ref. No. EN 17854:2024 E
worldwide for CEN national Members.
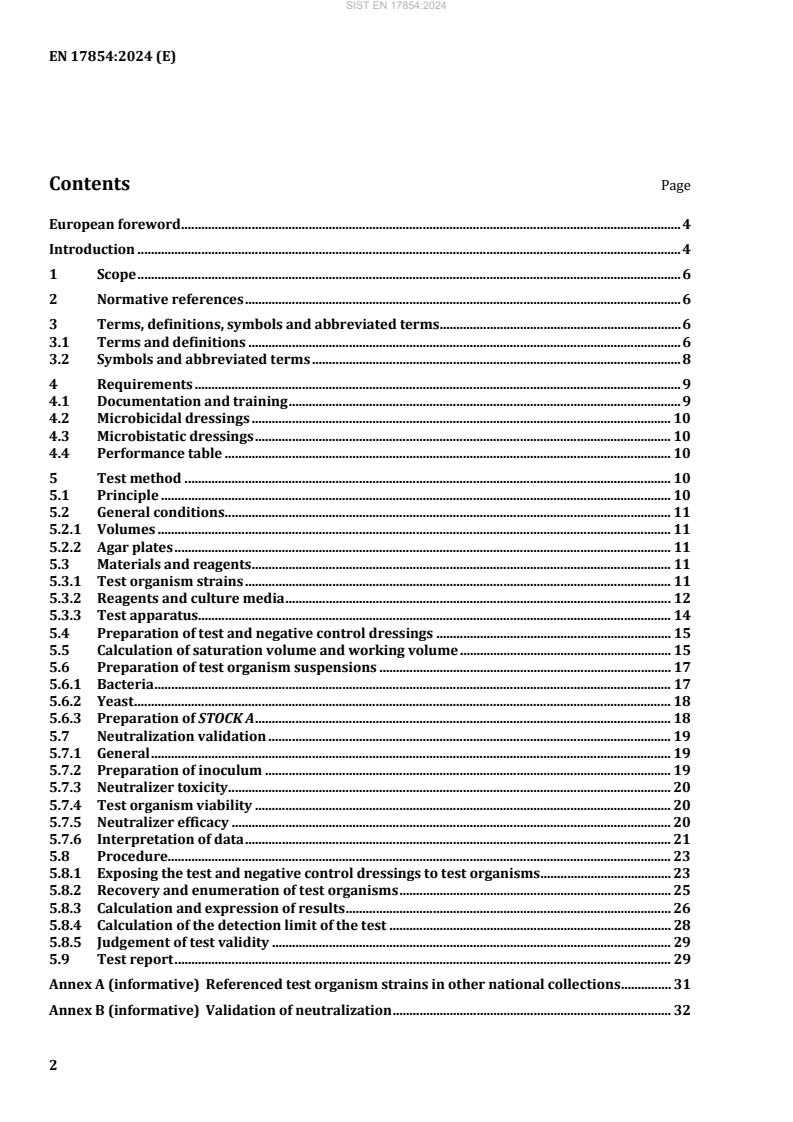
Contents Page
European foreword . 4
Introduction . 4
1 Scope . 6
2 Normative references . 6
3 Terms, definitions, symbols and abbreviated terms . 6
3.1 Terms and definitions . 6
3.2 Symbols and abbreviated terms . 8
4 Requirements . 9
4.1 Documentation and training . 9
4.2 Microbicidal dressings . 10
4.3 Microbistatic dressings . 10
4.4 Performance table . 10
5 Test method . 10
5.1 Principle . 10
5.2 General conditions . 11
5.2.1 Volumes . 11
5.2.2 Agar plates . 11
5.3 Materials and reagents . 11
5.3.1 Test organism strains . 11
5.3.2 Reagents and culture media . 12
5.3.3 Test apparatus. 14
5.4 Preparation of test and negative control dressings . 15
5.5 Calculation of saturation volume and working volume . 15
5.6 Preparation of test organism suspensions . 17
5.6.1 Bacteria . 17
5.6.2 Yeast . 18
5.6.3 Preparation of STOCK A . 18
5.7 Neutralization validation . 19
5.7.1 General . 19
5.7.2 Preparation of inoculum . 19
5.7.3 Neutralizer toxicity . 20
5.7.4 Test organism viability . 20
5.7.5 Neutralizer efficacy . 20
5.7.6 Interpretation of data . 21
5.8 Procedure. 23
5.8.1 Exposing the test and negative control dressings to test organisms . 23
5.8.2 Recovery and enumeration of test organisms . 25
5.8.3 Calculation and expression of results . 26
5.8.4 Calculation of the detection limit of the test . 28
5.8.5 Judgement of test validity . 29
5.9 Test report . 29
Annex A (informative) Referenced test organism strains in other national collections . 31
Annex B (informative) Validation of neutralization . 32
B.1 Principle . 32
B.2 Neutralizer selection . 32
Annex C (informative) Neutralizers . 33
Annex D (informative) Rationale . 34
D.1 General . 34
D.2 Title . 34
D.3 Test organism strains. 34
D.4 Preparation of test organism suspensions . 35
D.5 Cutting dressings . 35
D.6 Positive control . 35
D.7 Performance requirements . 35
D.8 Media . 36
D.9 Incubation temperatures . 36
D.10 Dressing classification . 36
D.11 Saturation volume . 36
D.12 Procedure . 36
D.13 Exposure times . 37
D.14 Pre-conditioning and repeat challenge testing. 37
D.15 Humidity . 37
D.16 Recovery of test organisms from dressings . 37
Annex E (informative) Replicates . 38
Annex F (informative) Test method illustrations . 39
Annex G (informative) Example Test Report Tables. 44
Bibliography . 46
European foreword
This document (EN 17854:2024) has been prepared by Technical Committee CEN/TC 205 “Non-active
medical devices” the secretariat of which is held by DIN.
This European Standard shall be given the status of a national standard, either by publication of an
identical text or by endorsement, at the latest by September 2024 and conflicting national standards shall
be withdrawn at the latest by September 2024.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN-CENELEC Internal Regulations, the national standards organizations of the
following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria, Croatia,
Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland,
Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of North
Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Türkiye and the United
Kingdom.
Introduction
This document specifies a test method for establishing whether a wound dressing exerts antimicrobial
activity.
This edition of the document is considered to be most suited for wound dressing types that have been
tested as part of the inter-laboratory comparisons; this means those that have an active antimicrobial
agent incorporated and with at least a small amount of absorbent capacity. No data has currently been
generated on other types of wound dressing (e.g. film, non-absorbing, multi-layered, adhesives, bacteria-
binding dressing, etc.) and therefore it is not known if this document is suitable for these wound dressing
types.
The laboratory test attempts to simulate conditions of application through the use of appropriate test
fluids, temperature, organisms, and exposure times, reflecting the parameters found in clinical situations.
Conditions which can influence the action of wound dressings having antimicrobial properties have been
included.
The conditions are intended to cover general purposes and to allow comparison between laboratories
and product types.
1 Scope
This document specifies minimum requirements and a test method for the antimicrobial (microbicidal or
microbistatic) activity of wound dressings. It applies to all wound dressings that specifically claim
antimicrobial activity according to this document.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
EN 12353, Chemical disinfectants and antiseptics - Preservation of test organisms used for the
determination of bactericidal (including Legionella), mycobactericidal, sporicidal, fungicidal and virucidal
(including bacteriophages) activity
3 Terms, definitions, symbols and abbreviated terms
3.1 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— IEC Electropedia: available at https://www.electropedia.org/
— ISO Online browsing platform: available at https://www.iso.org/obp/
3.1.1
antimicrobial wound dressing
wound dressing which can be shown to exert microbicidal or microbistatic properties
3.1.2
antimicrobial activity
A
capability of a wound dressing to either inhibit the growth or produce a reduction in the number of viable
cells of relevant test organisms under specified conditions, including viable bacterial cells and/or viable
vegetative yeast cells
3.1.3
dressing sample
piece of either the negative control dressing or test dressing that has been cut to the size required in this
document and used during testing
3.1.4
microbicidal
capability of the wound dressing to produce at least a 3-log reduction in the number of viable cells from
the test organisms when tested under the conditions in Clause 5
3.1.5
microbistatic
capability of the wound dressing to produce at least a 0-log reduction in the number of viable cells from
the test organisms when tested under the conditions in Clause 5
3.1.6
negative control dressing
wound dressing which is the same as the dressing to be tested but without the antimicrobial treatment
Note 1 to entry: If no similar wound dressing without the antimicrobial treatment is available, then a sterile gauze
swab shall be used.
3.1.7
neutralizer
chemical formulation to stop the antimicrobial effect of antimicrobial agents
3.1.8
plate count method
method in which the number of viable microorganisms present after incubation is calculated by counting
the number of CFU
3.1.9
plate factor
PF
factor used in CFU calculations which accounts for the volume of suspensions plated out onto agar plates
Note 1 to entry: This factor differs depending on choice of pour plates or spread plates.
3.1.10
saturation volume
SV
maximum volume of fluid absorbed by the dressing sample when tested according to the method in 5.5
of this document
3.1.11
simulated wound fluid
SWF
test medium intended to simulate wound exudate, for suspension of test organisms prior to exposure to
the dressing sample
3.1.12
test dressing
antimicrobial wound dressing which is tested to assess its antimicrobial activity
3.1.13
working volume
WV
volume of SWF added to the test or negative control dressing during the test, determined as 80 % of the
saturation volume
3.2 Symbols and abbreviated terms
For the purposes of this document, the following symbols and abbreviated terms apply.
A Antimicrobial activity
CFU Colony forming units
C Viable counts per negative control dressing at T = 0 h
C Viable counts per negative control dressing at T = 24 h
C Viable counts of INOC C
C
Viable counts per dressing sample (CFU / sample) used to calculate INOC C (in
Cs
Table 5)
C Viable counts per dressing sample (C , C , or T )
T 0 24 24
C Viable counts per ml
V
DF Dilution factor
h Hour
INITIAL STOCK Microbial suspension in MRD harvested from agar sub-culture
Inoculum for negative control dressing (prepared from STOCK B and calculated
INOC C
volume of uninoculated SWF equating to WV − 0,5 ml)
C
Inoculum for test dressing (prepared from STOCK B and calculated volume of
INOC T
uninoculated SWF equating to WV − 0,5 ml)
T
LOD Limit of detection
log C is the average logarithmic (log) value for the number of organisms obtained from
three samples of negative control dressing immediately after inoculation
log T is the average log value for the number of organisms obtained from three samples
of test dressing after incubation for 24 h
min Minutes
N Average number of CFU on P and P
1 2
N Undiluted test suspension
NE Neutralization effectiveness (%)
N Average Neutralizer efficacy in neutralization validation (CFU/ml)
EFF
NT Neutralization toxicity (%)
N Average Neutralizer toxicity in neutralization validation (CFU/ml)
TOX
N Average Test organism viability in neutralization validation (CFU/ml)
VIAB
P1 The number of organisms on plate 1 of duplicate agar plates (CFU)
P The number of organisms on plate 2 of duplicate agar plates (CFU)
PF Plate factor (3.1.9)
s Second
Microbial suspension of INITIAL STOCK diluted in MRD to contain 3 × 10 CFU/ml
STOCK A
to 1 × 10 CFU/ml, used to prepare STOCK B and STOCK N
Microbial suspension of STOCK A diluted in SWF to contain 3 × 10 CFU/ml to
STOCK B
1 × 10 CFU/ml
Microbial suspension of STOCK A diluted in MRD to contain 1,5 × 10 CFU/ml to
STOCK N
5,0 × 10 CFU/ml, used in Neutralization Validation when using 1 ml pour plates
SV Saturation volume
SV Average saturation volume of three replicates (g)
A
SV Highest percentage saturation volume of three replicates (%)
HIGH
SV Lowest percentage saturation volume of three replicates (%)
LOW
SV Highest measured saturation volume of three replicates (g)
MAX
SV Lowest measured saturation volume of three replicates (g)
MIN
SV Percentage spread for the three replicates (%)
SPREAD
T Viable counts per test dressing at T = 24 h
V Neutralizer Volume
N
Volume sampled from the paddle blender bag when preparing serial decimal
V
S
dilutions in 5.8.2.4 (ml)
V Test volume = Neutralizer volume (V ) + Working Volume (WV or WV ) (ml)
T N T c
W Average dressing sample mass at T = 0 h (g)
The average fully saturated dressing sample mass (g), as determined when the
W
Te
mass does not change between two time points by more than 5 %
Dressing sample mass following saturation in SWF at each time point as
W
Tv
applicable (g)
Working volume (3.1.13), the volume of SWF added to dressing sample during the
WV
test, determined as 80 % of the saturation volume (ml)
WV Working volume (WV) added to the negative control dressing (ml)
C
WV Working volume (WV) added to the test dressing (ml)
T
4 Requirements
4.1 Documentation and training
Laboratories performing the test in this document should be operating under an appropriate quality
management system (such as EN ISO 13485 [1], EN ISO/IEC 17025 [2] or similar). This ensures that
suitable records are retained by the test laboratory to allow full traceability of all raw data contributing
to the results in the test report (5.9) and competence in microbiological testing has been established.
4.2 Microbicidal dressings
When tested using the test method described in this document, antimicrobial wound dressings shall
demonstrate an antimicrobial activity of at least a 3-log reduction in activity in a valid test (5.8.5) at the
mandatory exposure time of 24 h (T = 24 h) and against all three test organisms (5.3.1).
NOTE 1 Log values in the text and formulae in this document refer to log .
NOTE 2 Rationale for microbicidal requirements is given in Annex D.
4.3 Microbistatic dressings
When tested using the test method described in this document, microbistatic wound dressings shall
demonstrate an antimicrobial activity that prevents further growth of the initial inoculum in a valid test
(5.8.5) at the mandatory exposure time of 24 h (T = 24 h) and against all three test organisms (5.3.1). This
means at least a 0-log reduction is obtained, which represents no increase in test organism numbers at
the mandatory exposure time of 24 h (T = 24 h) against all three test organisms (5.3.1).
4.4 Performance table
Table 1 shows the performance requirements for antimicrobial wound dressings to be classified as
microbicidal or microbistatic.
Table 1 — Performance requirements for antimicrobial wound dressings
Microbicidal Microbistatic
A ≥ 3,0 against all three test organisms A ≥ 0,0 against all three test organisms
A = Antimicrobial activity (5.8.3.5)
If a test dressing does not meet either a microbicidal or microbistatic requirement then it is non-
antimicrobial according to this document.
The test report (5.9) shall be supplied where claims of compliance with this document are made.
If a manufacturer makes a claim for antimicrobial activity for exposure times in addition to the mandatory
exposure time of 24 h (T = 24 h) then those additional time points may be tested using this document.
The viability of the test organism of the negative control dressing shall be validated for the additional
time points. The additional validation data and the test results shall be included in the test report (5.9)
and made available on request.
The test method in this document may be used with additional test organisms, including moulds,
provided that appropriate neutralization validation has been performed. If the results using such
additional test organisms are made publicly available, then the neutralization validation shall be made
available on request.
NOTE Example tables are given in Annex G.
5 Test method
5.1 Principle
A test suspension of bacteria or yeast in a solution of simulated wound fluid is inoculated into a sample
of a wound dressing (test and negative control dressing). The volume of test suspension added is
determined by calculating the saturation volume of the dressing sample prior to inoculation. The dressing
samples are maintained at a specified temperature for a specified exposure time, then transferred to a
previously validated neutralization medium so that the action of the antimicrobial agent is neutralized.
The number of surviving bacteria or yeast, which can be recovered from the test dressing, is then
quantitatively determined, and compared to the number of bacteria or yeast in a negative control
dressing at start of the test. The negative control dressing shall be treated in the same manner in place of
the test dressing during the whole test period.
NOTE Rationale for chosen test parameters is given in Annex D.
Any permitted deviations to this test method shall be suitably validated, documented in the report and
their use justified.
5.2 General conditions
5.2.1 Volumes
Unless otherwise specified, all volumes shall be within ± 5 %.
5.2.2 Agar plates
This document is written with the intention that 1 ml agar pour plates are used for enumeration, which
means 1 ml suspension volume mixed in each 15-20 ml molten agar. However, it is known that some
laboratories only use spread plates for enumeration. The change in volume when spread plates are used
requires accounting for at various points in the method. Therefore, throughout this document
instructions for the adjustments required when using spread plates have been given and users of this
document should ensure the required adjustments are carefully followed. Incubation times may need to
be reduced when using spread plates to prevent over-growth of colonies.
NOTE The use of a very low volume for spread plates will reduce the sensitivity of the test and this can affect
the ability to calculate the required 3 log reduction. Therefore, the use of 1 ml pour plates at all times is encouraged.
5.3 Materials and reagents
5.3.1 Test organism strains
5.3.1.1 Storage of organisms
The organisms shall be stored in accordance with the supplier’s recommendations or EN 12353.
The identification and origin (culture collection) of the organisms as well as the laboratory storage
method shall be recorded.
National collection test organism strains equivalent to those listed in 5.3.1.2 and 5.3.1.3 may be used;
some common alternative references in other national collections are given in Annex A.
5.3.1.2 Bacteria
The following two strains of bacteria shall be evaluated:
Pseudomonas aeruginosa ATCC 9027
Staphylococcus aureus ATCC 6538
5.3.1.3 Yeast
The following strain of yeast shall be evaluated:
Candida albicans ATCC 10231
5.3.1.4 Additional test organism strains
Additional test organism strains to those listed in 5.3.1.2 and 5.3.1.3 may be used for evaluation. Their
suitability for producing inocula of sufficient concentration shall be verified prior to use.
If the additional strains are not classified in a reference collection (e.g. clinical isolates), their
identification characteristics should be stated in the report and they should be held by the testing
laboratory for a minimum of five years to allow repeat testing if necessary.
5.3.2 Reagents and culture media
5.3.2.1 General
Reagents used in tests shall be of analytical quality and/or suited for microbiological purposes.
Dehydrated or ready-prepared products available on the commercial market are recommended for use
in preparing the culture media. The manufacturer’s instructions for the preparation, sterilization and
storage of culture media shall be strictly followed. Unless otherwise specified, all reagents shall be
equilibrated at ambient temperature (15 °C to 25 °C) before use.
Alternative media to those listed may be used, provided they have been suitably validated for use. The
TM TM1
use of alternative agar technologies, e.g. Petrifilm or Compact Dry plates, is also acceptable, provided
their use has been suitably validated and used to perform Neutralization Validation (5.7). Any alternative
media or media technologies shall be documented in the report as a deviation (5.9).
Substitution of Fetal Calf Serum (FCS), also known as Fetal Bovine Serum, in the SWF (5.3.2.5) is not
recommended (see Annex D, D.8).
5.3.2.2 Water
Purified water shall be used for the preparation of culture media, i.e. distilled, demineralized, deionized
or produced by reverse osmosis, or of equivalent quality free from substances likely to inhibit or influence
the growth of the microorganisms under the test conditions, e.g. traces of chlorine, traces of ammonia
and traces of metal ions.
NOTE See EN ISO 11133 [3] for more information on culture media preparation.
5.3.2.3 Tryptone Soya Broth (TSB)
For the maintenance of bacteria and performance of viable counts.
Tryptone, pancreatic digest of casein 15,0 g
Soya peptone, papaic digest of soya 5,0 g
NaCl 5,0 g
Water to 1 000 ml
Sterilize in the autoclave. After sterilization, the pH shall be between 7,1 to 7,5.
1 TM TM
Petrifilm and Compact Dry are examples of alternative agar products available commercially. This
information is given for the convenience of the users of this document and does not constitute an endorsement
by CEN or CENELEC of these products.
5.3.2.4 Tryptone Soya Agar (TSA)
For the maintenance of bacteria and performance of viable counts.
Tryptone, pancreatic digest of casein 15,0 g
Soya peptone, papaic digest of soya 5,0 g
NaCl 5,0 g
Agar 15,0 g
Water to 1 000 ml
Sterilize in the autoclave. After sterilization, the pH shall be between 7,1 to 7,5.
5.3.2.5 Simulated Wound Fluid (SWF)
For suspension of test organisms prior to exposure to dressing sample.
Maximum Recovery Diluent (5.3.2.6) 50 %
FCS; sterile, heat inactivated 50 %
The FCS shall be heat inactivated to remove complement activity either by the supplier or by the
laboratory prior to use. Mix MRD and FCS under aseptic conditions.
5.3.2.6 Maximum recovery diluent (MRD)
For preparation of SWF and test organism suspensions.
Peptone 1,0 g
NaCl 8,5 g
Water to 1 000 ml
Sterilize in the autoclave. After sterilization, the pH shall be between 6,8 to 7,2.
5.3.2.7 Sabouraud broth (SAB)
For the maintenance of yeast and performance of viable counts.
Peptone Neutral Bact. Peptone 10 g
Distilled water 1 000 ml
Heat to boiling to dissolve the peptone completely. Then add:
Glucose puriss (dextrose) 20 g
Dissolve the glucose by hand as soon as possible in the hot, but not boiling broth, and mix.
Sterilize in the autoclave. After sterilization, the pH shall be between 5,8 to 6,0.
5.3.2.8 Sabouraud agar (SAA)
For the maintenance of yeast and performance of viable counts.
Peptone Neutral Bact. Peptone 10 g
Agar bacteriological 18 g
Distilled water 1 000 ml
Heat to boiling to dissolve the peptone completely. Then add:
Glucose puriss (dextrose) 20 g
Dissolve the glucose by hand as soon as possible in the hot, but not boiling agar, and mix.
Sterilize in the autoclave. After sterilization, the pH shall be between 5,8 to 6,0.
5.3.2.9 Neutralizer
The neutralizing solution shall be validated for the active substance in the product under test in
accordance with 5.7. The neutralizer shall be sterile prior to use.
NOTE Information on neutralizers that have been found to be suitable for some categories of antimicrobials is
given in 5.7.5.2 and Annex C.
5.3.3 Test apparatus
Usual microbiological laboratory apparatus shall be required and in particular the following:
5.3.3.1 Spectrophotometer, capable of measuring at a 600 nm to 660 nm wavelength, or
McFarland’s nephelometer.
5.3.3.2 Incubators, capable of maintaining the following ranges: 20 °C to 25 °C, 30 °C to 34 °C and
30 °C to 35 °C.
5.3.3.3 Paddle blender, small size capable of handling volume up to 100 ml (e.g. Stomacher 80,
Biomaster or Neutec Masticator 2 Compact model – 80 ml) .
5.3.3.4 Sterile paddle blender bags.
® 3
5.3.3.5 Mixer, electromechanical agitator (e.g. Vortex mixer) .
5.3.3.6 Various sterile containers, test tubes, bottles and flasks of suitable capacity including 60 ml.
5.3.3.7 Sterile Petri dishes, 55 mm diameter and 90 mm diameter.
5.3.3.8 Forceps, sterile.
5.3.3.9 pH meter, suitably calibrated and capable of measuring the pH to ± 0,1 pH units at
19 °C to 21 °C.
5.3.3.10 Autoclave, capable of being maintained at 121 °C to 124 °C for a minimum holding time of
15 min.
5.3.3.11 Pipettes, calibrated of nominal capacities 10 ml, 1 ml and 0,1 ml. Automatic pipettes may be
used.
5.3.3.12 Cutting equipment, to provide dressing samples as specified in 5.4.3 (e.g. biopsy punch or
equivalent cutter).
5.3.3.13 Timer or stopwatch, calibrated.
Stomacher 80 Biomaster and Neutec Masticator 2 Compact model – 80 ml are examples of suitable products
available commercially. This information is given for the convenience of the users of this document and does not
constitute an endorsement by CEN or CENELEC of these products.
Vortex® mixer is an example of a suitable product available commercially. This information is given for the
convenience of the users of this document and does not constitute an endorsement by CEN or CENELEC of this
product.
5.3.3.14 Glass beads 3-4 mm, sterile.
5.4 Preparation of test and negative control dressings
5.4.1 Details of the negative control and test dressings to be tested shall be recorded per the
requirements of the test report (5.9).
5.4.2 Negative control dressings (3.1.6) and test dressings (3.1.12) shall be prepared as detailed in
5.4.3. If no negative control dressing is available, then a sterile gauze swab shall be used. The gauze shall
be cut to the same size as the test dressing and layered such that the mass allows the same saturation
volume as the test dressing (see 5.5) to be added.
5.4.3 Cut samples of test and negative control dressings with an area equivalent to 284 mm to
346 mm under aseptic conditions by using a sterile cutter e.g. a 20 mm diameter circular sample has an
area of 314,2 mm . Prior to cutting any dressings, remove the release liner if one is present.
5.5 Calculation of saturation volume and working volume
5.5.1 Saturation volume (SV) shall be determined for both the test and negative control dressings.
Determination of the saturation volume (SV) shall be carried out at 30 °C to 34 °C. Timings stated in this
clause shall be ± 30 s.
NOTE Saturation volume is initially determined by mass (g) then converted to volume (ml) when calculating
the working volume (5.5.13).
5.5.2 Weigh three replicates of each test and negative control dressing in empty 55 mm petri dishes
and record the mass to two decimal places (W ).
Alternative sterile containers to 55 mm Petri dishes may be used providing they are of a suitable size for
the dressing samples.
NOTE 55 mm Petri dishes were used during the development of this document.
5.5.3 Add aliquots of 12 ml SWF (an excess of SWF is required when determining SV) into six Petri
dishes with diameter of 55 mm in diameter. Allow the SWF to adjust to the incubator temperature
(30 °C to 34 °C).
NOTE The volumes do not have to be exact.
5.5.4 After being weighed, transfer each dressing sample into the Petri dish (5.5.3) containing SWF
using forceps. Test and negative control dressings that have a wound contact surface shall be placed with
the wound contact surface facing downwards onto the bottom of the petri dish. Place in the incubator for
30 min at 30 °C to 34 °C.
5.5.5 Gently remove dressing sample from the SWF using forceps without squeezing and allow any
excess fluid to drain for 5 s to 10 s. Thereafter, tap the dressing sample once on the side of the Petri dish
to remove any drops of SWF. Transfer the dressing sample to an empty petri dish that is already on a
balance that has been tared, and weigh. Record the mass of all replicate dressing samples to two decimal
places. These masses are denoted W . Tare the balance with the Petri dish; it is the mass of the dressing
Tv
sample that should be recorded. Residual fluid will thereby have no effect on the saturation volume.
For a graphical representation of Calculation of Saturation Volume and Working Volume, see Figure F.1 in
Annex F.
5.5.6 After weighing, return replicate to the same SWF-containing Petri dish as before (5.5.4) and
continue to incubate at 30 °C to 34 °C.
5.5.7 Repeat the weighing of the dressing samples at further time points until full saturation is achieved
(5.5.8)
NOTE It is not possible to specify the time points to be used in this step due to the variations between dressing
types. It is suggested 30 min time points can be used if there is no previous knowledge of the likely time the dressing
will take to reach full saturation. During development of this document the working group found that full saturation
of the dressing samples tested occurred within 4 h.
5.5.8 The mass determined at the first time point where there was ≤ 5 % change in mass from the
previous reading is denoted W . Dressing samples are considered fully saturated when the mass does
Te
not change between two time points by more than 5 %. An example of masses and calculations to
determine W is given in Table 2.
Te
Table 2 — Example calculation of W
Te
Dressing sample mass
Average dressing Average
sample mass change
W
Time point Tv
g g %
0 h 0 min (5.5.2) 0,13, 0,13, 0,13 0,13 (W ) N/A
a
0 h 30 min 2,36, 2,07, 2,01 2,15 (W ) N/A
Te
1 h 00 min 2,32, 2,04, 2,12 2,16 0,62
1 h 30 min 2,13, 2,37, 2,01 2,17 0,46
2 h 00 min 2,12, 2,09, 2,37 2,19 1,08
a
In this example, although mass (W ) were taken every 30 min up to 2 h, the mass did not change by more
Tv
than 5 % between 30 min and 60 min. Therefore, the mass when the dressing sample was considered fully
saturated (WTe) was the average mass at 30 min – 2,15 g.
5.5.9 Use the following formula to calculate the SV for each test and negative control dressings:
SV W− W
Te 0
where
SV is the saturation volume (g);
is the average dressing sample mass at T = 0 h (g);
W0
W is the average fully saturated dressing sample mass (g), as determined by the mass not
Te
changing between two time points by more than 5 %.
5.5.10 Calculate the average saturation volume (SV ) for the test and negative control dressings.
A
5.5.11 Use the following formulae to calculate the spread for the replicates:
SV − SV
A MIN
SV × 100
LOW
SV
A
=
=
SV − SV
MAX A
SV × 100
HIGH
SV
A
SV SV− SV
SPREAD HIGH LOW
where
SV is the average saturation volume of three replicates (g);
A
SV is the lowest measured saturation volume of three replicates (g);
MIN
SV is the highest measured saturation volume of three replicates (g);
MAX
SV is the percentage spread for the three replicates (%);
SPREAD
SV is the lowest percentage saturation volume of three replicates (%);
LOW
SV is the highest percentage saturation volume of three replicates (%).
HIGH
5.5.12 SV is acceptable if it is ≤ 20 %. If SV is > 20 % then the test shall be repeated using an
SPREAD SPREAD
increased number of replicates to confirm the result. If SV is confirmed to be > 20 % after the repeat
SPREAD
test (i.e. variable) then the use of this value shall be documented and justified in the report.
5.5.13 Convert SV for both test and negative control dressings from mass (g) to volume (ml), assuming
A
equivalency between 1 g = 1 ml.
5.5.14 Calculate the WORKING VOLUME (WV) to be added (WV for test dressings or WV for negative
T C
control dressings) when exposing dressing samples to test organisms (5.8.1).
WV 08,× SV
C A
WV 08,× SV
T A
where
SV is average saturation volume of three replicates (ml);
A
WV is working volume (3.1.13), the volume of SWF added to the test or control dressing
during the test, determined as 80 % of the saturation volume (ml);
WV is working volume (WV) added to the negative control dressing (ml);
C
WV is working volume (WV) added to the test dressing (ml).
T
5.5.15 Record the WV and WV results, rounded to one decimal place.
C T
5.6 Preparation of test organism suspensions
5.6.1 Bacteria
5.6.1.1 The test organisms and their stock cultures shall be prepared and kept in accordance with
EN 12353.
5.6.1.2 Prepare a subculture from the stock culture by streaking onto TSA slopes (also known as
slants) or TSA plates and incubate at 30 °C to 35 °C.
=
=
=
=
5.6.1.3 After 18 h to 24 h prepare a second subculture from the first subculture in the same way and
incubate for 18 h to 24 h.
5.6.1.4 From this second subculture, a third subculture may be produced in the same way. The
second and (if produced) third subculture are the working cultures.
If it is not possible to prepare the second subculture on a particular day, a 48 h subculture may be used,
provided that the subculture has been kept in the incubator at 30 °C to 35 °C during the 48 h period.
Only second or third subcultures shall be used.
5.6.2 Yeast
5.6.2.1 The test organisms and their stock cultures shall be prepared and kept in accordance with
EN 12353.
5.6.2.2 Prepare a subculture from the stock culture by streaking onto SAA slopes (also known as
slants) or SAA plates and incubate at 30 °C to 35 °C.
5.6.2.3 After 24 h to 48 h, prepare a second subculture from the first subculture in the same way and
incubate for 24 h to 48 h.
NOTE C. albicans ATCC 10231 usually grows sufficiently well within 24 h to 48 h at 30 °C to 35 °C.
5.6.2.4 From this second subculture, a third subculture may be produced in the same way. The
second and (if produced) third subculture are the working cultures.
If it is not possible to prepar
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...