EN 14476:2013
(Main)Chemical disinfectants and antiseptics - Quantitative suspension test for the evaluation of virucidal activity in the medical area - Test method and requirements (Phase 2/Step 1)
Chemical disinfectants and antiseptics - Quantitative suspension test for the evaluation of virucidal activity in the medical area - Test method and requirements (Phase 2/Step 1)
This European Standard specifies a test method and the minimum requirements for virucidal activity of chemical disinfectant and antiseptic products that form a homogeneous physically stable preparation when diluted with hard water or in the case of ready-to-use products, i. e, products that are not diluted when applied, with water. Products can only be tested at a concentration of 80 % (97 %, with a modified method for special cases) as some dilution is always produced by adding the test organisms and interfering substance.
This European Standard applies to products that are used in the medical area in the fields of hygienic handrub, hygienic handwash, instrument disinfection by immersion, surface disinfection by wiping, spraying, flooding or other means and textile disinfection.
This European Standard applies to areas and situations where disinfection is medically indicated. Such indications occur in patient care, for example:
- in hospitals, in community medical facilities, and in dental institutions;
- in clinics of schools, of kindergartens, and of nursing homes;
and may occur in the workplace and in the home. It may also include services such as laundries and kitchens supplying products directly for the patients.
NOTE 1 The method described is intended to determine the activity of commercial formulations or active substances under the conditions in which they are used.
NOTE 2 This method corresponds to a phase 2, step 1 test.
NOTE 3 EN 14885 specifies in detail the relationship of the various tests to one another and to "use recommendations".
Chemische Desinfektionsmittel und Antiseptika - Quantitativer Suspensionsversuch zur Bestimmung der viruziden Wirkung im humanmedizinischen Bereich - Prüfverfahren und Anforderungen (Phase 2, Stufe 1)
Dieses Dokument legt ein Prüfverfahren für und die Mindestanforderungen an die viruzide Wirkung von chemischen Desinfektionsmitteln und Antiseptika fest, die bei Verdünnung mit Wasser standardisierter Härte als homogene, physikalisch stabile Zubereitung vorliegen, bzw. bei gebrauchsfertigen Produkten, z. B. Produkte, die bei der Anwendung nicht mit Wasser verdünnt werden. Die Produkte können nur bei einer Konzentration von 80 % (97 % bei einem modifizierten Verfahren für Sonderfälle) geprüft werden, da durch Zugabe der Prüfkeime und der Belastungssubstanz immer eine gewisse Verdünnung bewirkt wird.
Diese Europäische Norm gilt für Produkte, die im medizinischen Bereich auf den Gebieten der hygienischen Händedesinfektion, hygienischen Händewaschung, Instrumentendesinfektion durch Eintauchen und Oberflächendesinfektion durch Abwischen, Besprühen, Überfluten oder auf sonstige Weise sowie für die Wäschedesinfektion verwendet werden.
Diese Europäische Norm gilt für Bereiche und unter Bedingungen, wo eine Desinfektion aus medizinischen Gründen angezeigt ist. Indikationen dieser Art liegen z. B. vor bei der Patientenbetreuung:
in Krankenhäusern, kommunalen medizinischen Einrichtungen und im Dentalbereich;
in medizinischen Bereichen in Schulen, Kindergärten und Heimen
und können auch am Arbeitsplatz oder im privaten Bereich gegeben sein. Eingeschlossen sein können auch Einrichtungen wie Wäschereien und Küchen, die der direkten Versorgung von Patienten dienen.
ANMERKUNG 1 Das beschriebene Verfahren dient zur Bestimmung der Wirksamkeit kommerziell erhältlicher Zuberei¬tungen oder Wirkstoffe unter den Bedingungen, unter denen sie angewendet werden.
ANMERKUNG 2 Dieses Verfahren entspricht einer Prüfung der Phase 2, Stufe 1.
ANMERKUNG 3 EN 14885 legt im Einzelnen die Beziehung der verschiedenen Prüfungen untereinander sowie zu den „Anwendungsempfehlungen“ fest.
Antiseptiques et désinfectants chimiques - Essai quantitatif de suspension pour l’évaluation de l’activité virucide dans le domaine médical - Méthode d’essai et prescriptions (Phase 2/Étape 1)
La présente Norme européenne spécifie une méthode d’essai et les prescriptions minimales relatives à l’activité virucide des produits antiseptiques et désinfectants chimiques qui forment une préparation homogène, physiquement stable, lorsqu’ils sont dilués dans l’eau dure ou – dans le cas de produits prêts à l’emploi, c’est-à-dire de produits qui ne sont pas dilués lors de leur utilisation – dans l’eau. Les produits ne peuvent être soumis à essai qu’à une concentration de 80 % (97 % avec une méthode modifiée dans certains cas particuliers), car l’ajout des microorganismes d’essai et de la substance interférente s’accompagne forcément d’une dilution.
La présente Norme européenne s’applique aux produits utilisés dans le domaine médical pour le traitement hygiénique des mains par frictions, le lavage hygiénique des mains, la désinfection des instruments par immersion, la désinfection des surfaces par essuyage, pulvérisation, inondation ou d’autres moyens, et la désinfection des textiles.
La présente Norme européenne s’applique aux domaines et situations où la désinfection est indiquée en médecine humaine. De telles indications se produisent pour les soins des patients, par exemple :
dans les hôpitaux, les centres médicaux communautaires et les institutions dentaires ;
dans les cliniques d’écoles, de jardins d’enfants et de maisons de soins infirmiers ;
et peuvent se produire sur le lieu de travail et à la maison. Elles peuvent également inclure les services tels que les blanchisseries et les cuisines fournissant directement des produits aux patients.
NOTE 1 La méthode décrite a pour objet de déterminer l’activité de formulations commerciales ou de substances actives dans leurs conditions d’emploi.
NOTE 2 Cette méthode correspond à un essai de phase 2, étape 1.
NOTE 3 L’EN 14885 spécifie de façon détaillée les relations des différents essais entre eux et avec les «recommandations d’emploi».
Kemična razkužila in antiseptiki - Kvantitativni suspenzijski preskus za vrednotenje virucidnega delovanja v medicini - Preskusna metoda in zahteve (faza 2, stopnja 1)
Ta evropski standard določa preskusno metodo in minimalne zahteve za virucidno delovanje kemičnih razkužil in antiseptikov, ki tvorijo homogen, fizikalno stabilen pripravek, če so razredčeni s trdo vodo ali, pri proizvodih, ki so pripravljeni za uporabo (tj. proizvodih, ki med uporabo niso razredčeni), z vodo. Proizvode je mogoče preskušati samo pri 80-odstotni koncentraciji (s prilagojeno metodo v posebnih primerih 97-odstotni), ker dodajanje preskusnih organizmov in moteče snovi vedno povzroči razredčenje. Ta evropski standard velja za proizvode, ki se uporabljajo na področju zdravstva pri higienskem drgnjenju rok, higienskem umivanju rok, dezinfekciji instrumentov s potapljanjem, površinski dezinfekciji z brisanjem, pršenjem, zalivanjem ali na druge načine in dezinfekciji tekstilij. Ta evropski standard se uporablja za področja in primere, ko obstajajo zdravniške indikacije za dezinfekcijo. Te indikacije se pojavljajo pri negi bolnikov, na primer: v bolnišnicah, skupnih zdravstvenih in zobozdravstvenih ustanovah; v klinikah šol, vrtcev in domov za starejše; in lahko nastanejo na delovnem mestu ali doma. Vključujejo lahko tudi storitve, kot so pralnice in kuhinje, ki proizvode neposredno dostavljajo bolnikom.
General Information
- Status
- Withdrawn
- Publication Date
- 13-Aug-2013
- Withdrawal Date
- 08-Feb-2026
- Technical Committee
- CEN/TC 216 - Chemical disinfectants and antiseptics
- Drafting Committee
- CEN/TC 216/WG 1 - Human medicine
- Current Stage
- 9960 - Withdrawal effective - Withdrawal
- Start Date
- 09-Sep-2015
- Completion Date
- 11-Feb-2026
Relations
- Effective Date
- 28-Aug-2013
- Effective Date
- 18-Jan-2023
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 05-Dec-2014
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
EN 14476:2013 is a standard published by the European Committee for Standardization (CEN). Its full title is "Chemical disinfectants and antiseptics - Quantitative suspension test for the evaluation of virucidal activity in the medical area - Test method and requirements (Phase 2/Step 1)". This standard covers: This European Standard specifies a test method and the minimum requirements for virucidal activity of chemical disinfectant and antiseptic products that form a homogeneous physically stable preparation when diluted with hard water or in the case of ready-to-use products, i. e, products that are not diluted when applied, with water. Products can only be tested at a concentration of 80 % (97 %, with a modified method for special cases) as some dilution is always produced by adding the test organisms and interfering substance. This European Standard applies to products that are used in the medical area in the fields of hygienic handrub, hygienic handwash, instrument disinfection by immersion, surface disinfection by wiping, spraying, flooding or other means and textile disinfection. This European Standard applies to areas and situations where disinfection is medically indicated. Such indications occur in patient care, for example: - in hospitals, in community medical facilities, and in dental institutions; - in clinics of schools, of kindergartens, and of nursing homes; and may occur in the workplace and in the home. It may also include services such as laundries and kitchens supplying products directly for the patients. NOTE 1 The method described is intended to determine the activity of commercial formulations or active substances under the conditions in which they are used. NOTE 2 This method corresponds to a phase 2, step 1 test. NOTE 3 EN 14885 specifies in detail the relationship of the various tests to one another and to "use recommendations".
This European Standard specifies a test method and the minimum requirements for virucidal activity of chemical disinfectant and antiseptic products that form a homogeneous physically stable preparation when diluted with hard water or in the case of ready-to-use products, i. e, products that are not diluted when applied, with water. Products can only be tested at a concentration of 80 % (97 %, with a modified method for special cases) as some dilution is always produced by adding the test organisms and interfering substance. This European Standard applies to products that are used in the medical area in the fields of hygienic handrub, hygienic handwash, instrument disinfection by immersion, surface disinfection by wiping, spraying, flooding or other means and textile disinfection. This European Standard applies to areas and situations where disinfection is medically indicated. Such indications occur in patient care, for example: - in hospitals, in community medical facilities, and in dental institutions; - in clinics of schools, of kindergartens, and of nursing homes; and may occur in the workplace and in the home. It may also include services such as laundries and kitchens supplying products directly for the patients. NOTE 1 The method described is intended to determine the activity of commercial formulations or active substances under the conditions in which they are used. NOTE 2 This method corresponds to a phase 2, step 1 test. NOTE 3 EN 14885 specifies in detail the relationship of the various tests to one another and to "use recommendations".
EN 14476:2013 is classified under the following ICS (International Classification for Standards) categories: 11.080.20 - Disinfectants and antiseptics. The ICS classification helps identify the subject area and facilitates finding related standards.
EN 14476:2013 has the following relationships with other standards: It is inter standard links to EN 14476:2005+A1:2006, EN 14476:2013+A1:2015, EN 14885:2022, EN 12353:2021, EN ISO 23125:2010, EN 14476:2013/FprA1. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
EN 14476:2013 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.Chemische Desinfektionsmittel und Antiseptika - Quantitativer Suspensionsversuch zur Bestimmung der viruziden Wirkung im humanmedizinischen Bereich - Prüfverfahren und Anforderungen (Phase 2, Stufe 1)Antiseptiques et désinfectants chimiques - Essai quantitatif de suspension pour l’évaluation de l’activité virucide dans le domaine médical - Méthode d’essai et prescriptions (Phase 2/Étape 1)Chemical disinfectants and antiseptics - Quantitative suspension test for the evaluation of virucidal activity in the medical area - Test method and requirements (Phase 2/Step 1)11.080.20Dezinfektanti in antiseptikiDisinfectants and antisepticsICS:Ta slovenski standard je istoveten z:EN 14476:2013SIST EN 14476:2013en,fr,de01-november-2013SIST EN 14476:2013SLOVENSKI
STANDARDSIST EN 14476:2005+A1:20071DGRPHãþD
EUROPEAN STANDARD NORME EUROPÉENNE EUROPÄISCHE NORM
EN 14476
August 2013 ICS 11.080.20 Supersedes EN 14476:2005+A1:2006English Version
Chemical disinfectants and antiseptics - Quantitative suspension test for the evaluation of virucidal activity in the medical area - Test method and requirements (Phase 2/Step 1)
Antiseptiques et désinfectants chimiques - Essai quantitatif de suspension pour l'évaluation de l'activité virucide dans le domaine médical - Méthode d'essai et prescriptions (Phase 2/Étape 1)
Chemische Desinfektionsmittel und Antiseptika - Quantitativer Suspensionsversuch zur Bestimmung der viruziden Wirkung im humanmedizinischen Bereich - Prüfverfahren und Anforderungen (Phase 2, Stufe 1) This European Standard was approved by CEN on 5 July 2013.
CEN members are bound to comply with the CEN/CENELEC Internal Regulations which stipulate the conditions for giving this European Standard the status of a national standard without any alteration. Up-to-date lists and bibliographical references concerning such national standards may be obtained on application to the CEN-CENELEC Management Centre or to any CEN member.
This European Standard exists in three official versions (English, French, German). A version in any other language made by translation under the responsibility of a CEN member into its own language and notified to the CEN-CENELEC Management Centre has the same status as the official versions.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, Former Yugoslav Republic of Macedonia, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION EUROPÄISCHES KOMITEE FÜR NORMUNG
Management Centre:
Avenue Marnix 17,
B-1000 Brussels © 2013 CEN All rights of exploitation in any form and by any means reserved worldwide for CEN national Members. Ref. No. EN 14476:2013: ESIST EN 14476:2013
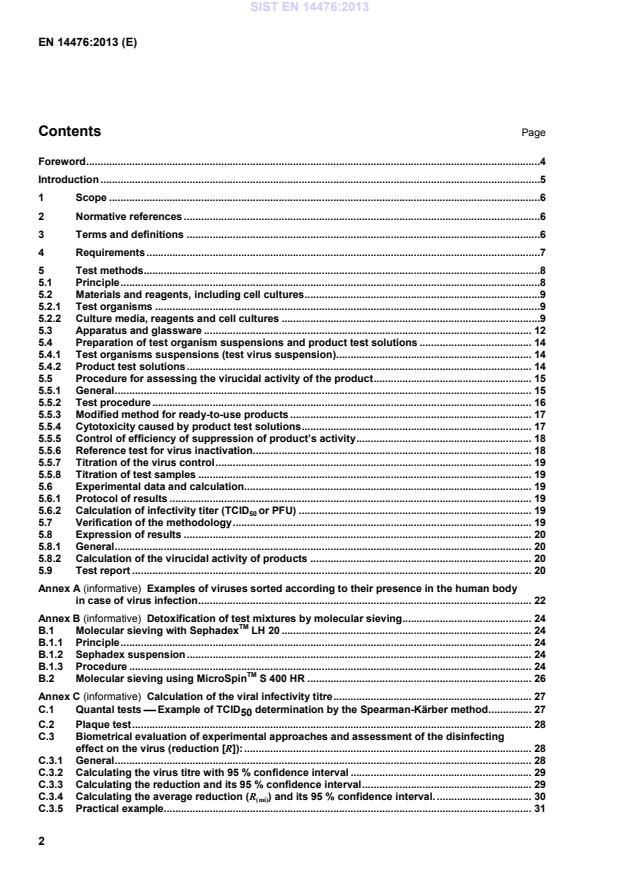
Examples of viruses sorted according to their presence in the human body in case of virus infection . 22 Annex B (informative)
Detoxification of test mixtures by molecular sieving. 24 B.1 Molecular sieving with SephadexTM LH 20 . 24 B.1.1 Principle . 24 B.1.2 Sephadex suspension . 24 B.1.3 Procedure . 24 B.2 Molecular sieving using MicroSpinTM S 400 HR . 26 Annex C (informative)
Calculation of the viral infectivity titre . 27 C.1 Quantal tests Example of TCID50 determination by the Spearman-Kärber method . 27 C.2 Plaque test . 28 C.3 Biometrical evaluation of experimental approaches and assessment of the disinfecting effect on the virus (reduction [R]): . 28 C.3.1 General . 28 C.3.2 Calculating the virus titre with 95 % confidence interval . 29 C.3.3 Calculating the reduction and its 95 % confidence interval . 29 C.3.4 Calculating the average reduction (R(mi)) and its 95 % confidence interval. . 30 C.3.5 Practical example. 31 SIST EN 14476:2013
Presentation of test results of one active concentration . 33 Annex E (informative)
Quantitative determination of formaldehyde concentrations . 36 Bibliography . 37
80 %, i.e. 9 7%. Data obtained using the former version of EN 14476 may still be used. Other methods to evaluate the efficacy of chemical disinfectants and antiseptics for different applications in the medical area are in preparation. According to the CEN/CENELEC Internal Regulations, the national standards organisations of the following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, Former Yugoslav Republic of Macedonia, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and the United Kingdom. SIST EN 14476:2013
3.2
plaque forming units
PFU number of infectious virus particles per unit volume (ml) SIST EN 14476:2013
test with a defined product (e.g. formaldehyde) in parallel with a product under test for the internal control of the test 3.4 TCID50 50 % infecting dose of a virus suspension or that dilution of the virus suspension that induce a CPE (3.5) in 50 % of cell culture units 3.5 viral cytopathic effect
CPE
morphological alteration of cells and/or their destruction as a consequence of virus multiplication 3.6 viral plaque
area of lysis formed in a cell monolayer under semisolid medium due to infection by and multiplication of a single infectious virus particle
3.7 virus titre amount of infectious virus per unit volume present in a cell culture lysate or in a solution 4 Requirements The product shall demonstrate at least a decimal log (lg) reduction of 4 in virus titre when tested in accordance with Table 1 and Clause 5. SIST EN 14476:2013
disinfection
Minimum spectrum of test organisms
Poliovirus Adenovirus Murine Norovirus Limited spectrum virucidal activity a Adenovirus
Murine Norovirus Poliovirus Adenovirus Murine Norovirus
when temperature is
40 °C or higher: only
Parvovirus Poliovirus Adenovirus Murine Norovirus
Parvovirus additional Any relevant test organism Test temperature according to the manufacturer’s recommendation, but at / between
20 °C
20 °C and 70 °C
4 °C and 30 °C
30 °C and 70 °C
Contact time according to the manufacturer’s recommendation
but between
but no longer than
but no longer than
but no longer than
30 s and 120 s 60 min
5 min or
60 min b 20 min Interfering substance
clean conditions
0,3 g/l bovine albumin solution (hygienic handrub) c 0,3 g/l bovine albumin solution
and/or
0,3 g/l bovine albumin solution
and/or
dirty conditions 3,0 g/l bovine albumin solution plus 3,0 ml/l erythrocytes (hygienic handwash) d
3,0 g/l bovine albumin solution plus 3,0 ml/l erythrocytes
3,0 g/l bovine albumin solution plus 3,0 ml/l erythrocytes
3,0 g/l bovine albumin solution plus 3,0 ml/l erythrocytes Additional conditions e clean or dirty c, d;
any relevant substance any relevant substance any relevant substance any relevant substance
a The test for limited spectrum virucidal activity will cover all enveloped viruses (Annex A) and the specified test organisms . b The contact times for surface disinfectants stated in this table are chosen on the basis of the practical conditions of the product. The recommended contact time for the use of the product is within the responsibility of the manufacturer. Products intended to disinfect surfaces that are likely to come into contact with the patient and / or the medical staff and surfaces, which are frequently touched by different people, leading to the transmission of microorganisms to the patient, shall be tested with a contact time of maximum 5 min. The same applies where the contact time of the product shall be limited for practical reasons. Products for other surfaces than stated above may be tested with a contact time of maximum 60 min.
c Hygienic handrub shall be tested as a minimum under clean conditions.
d Hygienic handwash shall be tested as a minimum under dirty conditions.
e For the additional conditions, the concentration defined as a result can be lower than the one obtained under the minimum test conditions.
5 Test methods 5.1 Principle 5.1.1 A sample of the product as delivered and/or diluted with hard water (or water for ready to use products) is added to a test suspension of viruses in a solution of an interfering substance. The mixture is maintained at one of the temperatures and the contact times specified in Clause 4 and 5.5.1.1. At the end of this contact time, an aliquot is taken; the virucidal action in this portion is immediately suppressed by a validated method (dilution of the sample in ice-cold cell maintenance medium). The dilutions are transferred into cell culture units (petri dishes, tubes or wells of microtitre plates) either using monolayer or cell suspension. Infectivity tests are done either by plaque test or quantal tests. After incubation, the titres of infectivity are calculated according to Spearman and Kärber (quantal tests, C.1) or by plaque counting (plaque test, C.2) and evaluated. Reduction of virus infectivity is calculated from differences of lg virus titres before (virus control) and after treatment with the product. SIST EN 14476:2013
a) Non-enveloped RNA virus2)
1) Poliovirus type 1, LSc 2ab (Picornavirus) 2) Murine norovirus, strain S99 Berlin b) Non-enveloped DNA virus 1) Adenovirus type 5, strain Adenoid 75, ATCC VR-5* 2) Murine Parvovirus, minute virus of mice, strain Crawford, ATCC VR-1346 The required incubation temperature for these test organisms is 36 °C ± 1 °C or 37 °C ± 1 °C (5.3.1.3). The same temperature (either 36 °C or 37 °C) shall be used for all incubations performed during a test and its control and validation. If additional test organisms are used, they shall be kept and used under optimum growth conditions (temperature, time, atmosphere, media) noted in the test report. If these additional test organisms are not classified at a reference centre, their identification characteristics shall be stated. In addition, they shall be held by the testing laboratory or national culture collection under a reference for five years. 5.2.2 Culture media, reagents and cell cultures 5.2.2.1 General All weights of chemical substances given in this European Standard refer to the anhydrous salts. Hydrated forms may be used as an alternative, but the weights required shall be adjusted to allow for consequent molecular weight differences. The reagents shall be of analytical grade and/or appropriate for microbiological purposes. They shall be free from substances that are toxic or inhibitory to the test organisms.
1) The ATCC numbers are the collection numbers of strains supplied by these culture collections. This information is given for the convenience of users of this European Standard and does not constitute an endorsement by CEN of the product named. 2) Virus strains may be obtained from a national or international culture collection. Regarding Poliovirus only virus material that passed the requirements for the production of oral polio vaccine of the World Health Organisation (WHO) shall be used (Other stocks derived from LSc-2ab cannot be used any longer). LSc-2ab can be obtained from NIBSC (www.nibsc.ac.uk: contact Dr. Javier Martin) or from Eurovir Hygiene Institut (www.eurovir.de: contact Dr. Jursch). Murine Norovirus may be obtained from Friedrich-Loeffler-Insitut Bundesforschunsinstitut für Tiergesundheit, Hauptsitz Insel Riems Südufer 10, 17493, Greifswald-Insel Riems; phone: +49 38351 7-0, fax: +49 038351 7-121. http://www.fli.bund.de. SIST EN 14476:2013
For each culture medium and reagent, a time limitation for use should be fixed.
All specified pH values are measured at 20 °C ± 1 °C. 5.2.2.2 Water The water shall be freshly glass-distilled water and not demineralised water. If distilled water of adequate quality is not available, water for injections (see bibliographic reference [1]) may be used. Sterilise in the autoclave [5.3.1.1 a)]. Sterilisation is not necessary if the water is used e.g. for preparation of culture media and subsequently sterilised.
See 5.2.2.7 for the procedure to prepare hard water. 5.2.2.3 Phosphate buffered saline (PBS) Sodium chloride (NaCl) 8,00 g Potassium chloride (KCl) 0,20 g Disodium hydrogen phosphate, 12-hydrate (Na2HPO4 x 12H2O) 2,89 g Potassium phosphate, monobasic (KH2PO4) 0,20 g Water (5.2.2.2) to 1 000,0 ml 5.2.2.4 Neutral Red (1:1000 solution) Prepare neutral red (Sigma N7005) stock solution at 0,1 mg/ml in water (5.2.2.2). Filter through a 0,40 µm pore size filter and store 4 °C in the dark. 5.2.2.5 Foetal calf serum (FCS) FCS has to be certified free of viruses and mycoplasma. Extraneous viruses and mycoplasma may interfere with cell and virus growth resulting in false results. For RAW 264.7 cells, special FCS has to be used due to the cells’ high sensitivity to endotoxins. 5.2.2.6 Trichloroacetic acid (10 % solution) (TCA) Dissolve 10 g of TCA crystals in 80 ml of water (5.2.2.2), then adjust the volume to 100 ml with water. Stir to complete solution.
5.2.2.7 Hard water for dilution of products For the preparation of 1 l of hard water, the procedure is as follows: prepare solution A: dissolve 19,84 g magnesium chloride (MgCl2) and 46,24 g calcium chloride (CaCl2) in water (5.2.2.2) and dilute to 1 000 ml. Sterilise by membrane filtration (5.3.1.7) or in the autoclave [5.3.1.1 a)]. Autoclaving – if used - may cause a loss of liquid. In this case make up to 1 000 ml with water (5.2.2.2) under aseptic conditions. Store the solution in the refrigerator (5.3.1.8) for no longer than one month; prepare solution B: dissolve 35,02 g sodium bicarbonate (NaHCO3) in water (5.2.2.2) and dilute to 1000 ml. Sterilise by membrane filtration (5.3.1.7). Store the solution in the refrigerator (5.3.1.8) for no longer than one week; place 600 ml to 700 ml of water (5.2.2.2) in a 1 000 ml volumetric flask (5.3.1.12) and add 6,0 ml (5.3.1.9) of solution A, then 8,0 ml of solution B. Mix and dilute to 1 000 ml with water (5.2.2.2). The pH (5.3.1.4) of the hard water shall be 7,0 ± 0,2. (5.3.1.4). If necessary, adjust the pH by using a solution of SIST EN 14476:2013
The hard water shall be freshly prepared under aseptic conditions and used within 12 h. NOTE When preparing the product test solutions (5.4.2), the addition of the product to the hard water produces different final water hardness in each test tube. In any case, the final hardness in the test tube expressed as calcium carbonate (CaCO3) is lower than 375 mg/l. 5.2.2.8 Interfering substance 5.2.2.8.1 General The interfering substance shall be chosen according to the conditions of use laid down for the product.
The interfering substance shall be sterile and prepared at 10 times its final concentration in the test (50 times in the case of the modified method, 5.2.2.8.4). The ionic composition (e.g. pH, calcium and/or magnesium hardness) and chemical composition (e.g. mineral substances, protein, carbohydrates, lipids and detergents) shall be defined. “Diluent” is generally used in the other European Standards in the medical area to prepare the interfering substance. Since there is no experience in virucidal testing with diluent, water (5.2.2.2) is used instead.
NOTE The term “interfering substance” is used even if it contains more than one substance. 5.2.2.8.2 Clean conditions (bovine albumin solution – low concentration) Dissolve 0,30 g of bovine albumin fraction V (suitable for microbiological purposes) in 100 ml of water (5.2.2.2). Sterilise by membrane filtration (5.3.1.7), keep in a refrigerator (5.3.1.8) and use within one month. The final concentration of the bovine albumin in the test procedure (5.5) shall be 0,3 g/l ; 5.2.2.8.3 Dirty conditions (Mixture of bovine albumin solution – high concentration with sheep erythrocytes) Dissolve 3,00 g of bovine albumin fraction V (suitable for microbiological purposes) in 97 ml of water (5.2.2.2). Sterilise by membrane filtration (5.3.1.7). Prepare at least 8,0 ml fresh defibrinated sheep blood (5.2.2.9). Centrifuge the erythrocytes at 800 gN for 10 min (5.3.1.13). After discarding the supernatant, resuspend erythrocytes in water (5.2.2.2). Repeat this procedure at least 3 times, until the supernatant is colourless.
Resuspend 3 ml of the packed sheep erythrocytes in the 97 ml of sterilised bovine albumin solution (see above). To avoid later contamination this mixture should be split in portions probably needed per day. Keep the mixture in separate containers for a maximum of 7 d in a refrigerator (5.3.1.8). The final concentration of bovine albumin and sheep erythrocytes in the test procedure (5.5) shall be 3 g/l and 3 ml/l respectively. 5.2.2.8.4 Clean and dirty conditions for the modified method for ready-to-use products (5.5.4) Follow the procedures for preparation according to 5.2.2.8.2 and 5.2.2.8.3, but prepare the interfering substance in fivefold higher concentrations, for the dirty conditions maximum 50 ml to avoid problems with the filtration. SIST EN 14476:2013
a) A growth medium for cell multiplication is supplemented with 10 % FCS. Add 10 parts of FCS (5.2.2.5) to 90 parts of MEM. b) A maintenance medium to maintain the cell culture metabolism without stimulation of cell proliferation is supplemented with 2 % FCS. Add 2 parts of FCS (5.2.2.5) to 98 parts of MEM. Other media may be used if appropriate for certain cell lines. See also bibliographic reference [2]. See EN 12353 for a detailed description. 5.2.2.11 Cell cultures Cell monolayers shall be >90 % confluent before inoculation. Cell lines are selected in accordance with their sensitivity to the test organisms (5.2.1). Cells for virus titration, if used as suspensions in quantal tests, shall be added to the dilutions of the test mixture (5.5.2) in such a density as to enable the formation of a monolayer in at least two days in the cell control. Cell cultures can be used as cell monolayers or in suspensions for quantal tests. For details of cell lines see 5.5.1.1 e). 5.3 Apparatus and glassware Sterilise all glassware and parts of the apparatus that will come into contact with the culture media and reagents or the sample, except those which are supplied sterile, by one of the following methods: a) by moist heat, in the autoclave [5.3.1.1 a)]; b) by dry heat, in the hot air oven [5.3.1.1 b)]. 5.3.1 Usual microbiological laboratory equipment3) and, in particular, the following: 5.3.1.1 Apparatus for sterilisation (moist and dry heat): a) For moist heat sterilisation, an autoclave capable of being maintained at (30121+) °C for a minimum holding time of 15 min;
b) for dry heat sterilisation, a hot air oven capable of being maintained at (50180+) °C for a minimum holding time of 30 min, at (50170+) °C for a minimum holding time of 1 h or at (50160+) °C for a minimum holding time of 2 h.
3) Disposable sterile equipment is an acceptable alternative to reusable glassware. SIST EN 14476:2013
5.3.1.4 pH-meter, having an inaccuracy of calibration of no more than ± 0,1 pH units at 20 °C ± 1 °C.
5.3.1.5 Stopwatch. 5.3.1.6 Shakers. a) Electromechanical agitator, e.g. Vortex® mixer4); b) Mechanical shaker. 5.3.1.7 Membrane filtration apparatus, constructed of a material compatible with the substances to be filtered, with a filter holder of at least 50 ml volume, and suitable for use of filters of diameter 47 mm to 50 mm and 0,22 µm pore size for sterilisation of hard water (5.2.2.7) and bovine albumin (5.2.2.8.2, 5.2.2.8.3 and 5.2.2.8.4). The vacuum source used shall give an even filtration flow rate. In order to obtain a uniform distribution of the micro-organisms over the membrane and to prevent overlong filtration, the device shall be set so as to obtain the filtration of 100 ml in 20 s to 40 s. The filtration of the interfering substance (5.2.2.8) for the modified method (5.5.3) may take a longer time. 5.3.1.8 Refrigerator, capable of being controlled at 2 °C to 8 °C. 5.3.1.9 Graduated pipettes, of nominal capacities 10 ml, 1 ml, 100 µl, 10 µl or calibrated automatic pipettes. 5.3.1.10
Ice producing machine or commercially available ice to cool the cell maintenance medium and the reaction mixtures during the test. 5.3.1.11 Basin as ice bath with ice and water. 5.3.1.12 Volumetric flasks. 5.3.1.13 Centrifuge (400 gN to 1000 gN). 5.3.1.14 Microtitre plates or tubes, petri dishes and flasks for cell culture use. 5.3.1.15 Magnetic stirrer for keeping cells in suspension before seeding. 5.3.1.16 Inverted microscope for reading cell cultures microscopically. 5.3.1.17 Container: sterile test tubes, culture bottles or flasks of suitable capacity. 5.3.1.18 Biological safety cabinet, class II. 5.3.1.19 Freezer, -70 °C or less.
4) Vortex® is an example of a suitable product available commercially. This information is given for the convenience of users of this European Standard and does not constitute an endorsement by CEN of this product. SIST EN 14476:2013
In exceptional cases the test suspension may be concentrated by appropriate methods (e.g. ultracentrifugation). The test suspension is kept in small volumes below -70 °C or preferably at -196 °C under nitrogen. Due to safety reasons, and – in some cases – to limit the possibility of genetic mutations, only 10 passages from the original seed (e.g. virus from culture collection) are allowed. The test suspension is used undiluted for the test procedure (5.5.2 or 5.5.3). 5.4.2 Product test solutions The concentration of a product test solution shall be 1,25 times the desired test concentration (= real test concentration) because it is diluted to 80 % during the test (5.5.2). Product test solutions shall be prepared in hard water (5.2.2.7) at minimum three different concentrations to include one concentration in the active range and one concentration in the non-active range (5.7). The product as received may be used as one of the product test solutions, in this case the highest tested concentration is 80 %. Ready-to-use products may be tested at 97 % [modified method (5.5.3)]. In this case, the “real test concentration” is 97 %. Dilutions of ready-to-use products shall be prepared in water (5.2.2.2) instead of hard water. Handwash products are always prediluted with hard water (5.2.2.7) to achieve a 62,5 % solution. This solution simulates the addition of tap water in practice (1:1). Such a product is nevertheless regarded as a “ready-to-use product”. The modified method (5.5.3) cannot be used, since 62,5 % represents the highest accepted concentration (50 %), multiplied by 1,25. For solid products, dissolve the product as received by weighing at least 1,0 g ± 10 mg of the product in a volumetric flask and filling up with hard water (5.2.2.7). Subsequent dilutions (= lower concentrations) shall be prepared in volumetric flasks (5.3.1.12) on a volume/volume basis in hard water (5.2.2.7).
For liquid products, dilutions of the product shall be prepared with hard water in volumetric flasks (5.3.1.12) on a volume/volume basis. The product test solutions shall be prepared freshly and used in the test within 2 h. They shall give a physically homogenous preparation, stable during the whole procedure. If during the procedure a visible inhomogeneity appears due to the formation of a precipitate or flocculate (for example, through the addition of the interfering substance), it shall be recorded in the test report. The concentration of the product stated in the test report shall be the desired test concentration. Record the test concentration in terms of mass per volume or volume per volume and details of the product sample as received. SIST EN 14476:2013
The experimental conditions may be selected according to the practical use considered for the product (Clause 4): a) temperature θ (in °C): The temperatures to be tested are specified in Clause 4, Table 1. The allowed deviation for each chosen temperature is ± 1 °C.
b) contact time t (in min): The contact times to be tested are specified in Clause 4, Table 1. The allowed deviation for each chosen contact time is ± 10 s, except for 1 min or less where it is ± 5 s. c) interfering substance: The interfering substance to be tested is either 0,30 g/l bovine albumin (5.2.2.8.2) representing clean conditions or a mixture of 3 ml/l sheep erythrocytes and 3,0 g/l bovine albumin (5.2.2.8.3) representing dirty conditions – according to Clause 4, Table 1 and practical applications. Additional interfering substances may be tested according to specific fields of application. d) test organisms: The test organisms to be tested are specified in Clause 4, Table 1 and 5.2.1. Additional test organisms may be tested. e) cell line(s):
Adenovirus is multiplied in HeLa cells or other cell lines of appropriate sensitivity
Poliovirus is multiplied in HeLa cells or other cell lines of appropriate sensitivity
Norovirus is multiplied in RAW 264.7 cells (ATCC TIB-71) or other cell lines of appropriate sensitivity
Parvovirus is multiplied in A9 cells (ATCC CCL-1.4) or other cell lines of appropriate sensitivity. 5.5.1.2 Preparation Tubes are filled with ice-cold maintenance medium (5.2.2.10 b)) for the various titrations that have to be performed after the different contact times and placed in an ice bath. Microtitre plates are labelled for identification. The procedures described under 5.5.4 to 5.5.8 are always carried out in parallel with the test procedure (5.5.2). 5.5.1.3 Special instruction for ready-to-use products In the case of ready-to-use products use water (5.2.2.2) instead of hard water, but observe the exception with handwash products (5.1.1, NOTE). 5.5.1.4 Equilibration of temperature Prior to testing, equilibrate all reagents [product test solutions (5.4.2), PBS (5.2.2.3), cell culture (5.2.2.11), water (5.2.2.2), hard water (5.2.2.7) and interfering substance (5.2.2.8)] to the test temperature of θ (5.5.1.1 a)) using the water bath (5.3.1.2) controlled at θ. Check that the temperature of the reagents is stabilised at θ. The test suspension (5.4.1.1) is kept in the ice bath (5.3.1.11) to avoid titre loss. Water (5.2.2.2) shall be equilibrated at a temperature of 20 °C ± 1 °C. In the case of ready-to-use-products, water (5.2.2.2) shall be additionally equilibrated to θ.
Pipette 1 ml of interfering substance (5.2.2.8) into a container of suitable capacity for appropriate mixing. Add 1 ml of the virus test suspension (5.4.1) to the container, carefully avoiding the upper part of the sides. Mix [5.3.1.6 a)]. Add 8 ml of the product test solution (5.4.2) to the container. Mix [5.3.1.6 a)], start a stopwatch at once and place the container in a water bath (5.3.1.2) controlled at the chosen test temperature [5.5.1.1a)]. The activity of the product shall be determined for the contact time(s) according to Clause 4, Table 1. Immediately at the end of the chosen contact time, mix [5.3.1.6 a)], pipette 0,5 ml of the test mixture into 4,5 ml ice-cold maintenance medium [5.2.2.10 b)] and put into an ice bath (5.3.1.11). Within 30 min prepare a series of ten-fold dilutions of this mixture (test mixture + maintenance medium). Pipette tips shall be changed after each dilution to avoid carry-over of viruses. After incubation, the virus titre is calculated, reduction of virus infectivity is determined from differences of lg virus titres before (see 5.5.7) and after treatment with the product.
After treatment with the product the infectivity is tested with one of the following procedures: a) Quantal tests (endpoint titration) – [the procedures 1) to 3) are alternatives] 1) Virus titration on cells in suspension on microtitre plates: Transfer 0,1 ml of each dilution into six or eight wells of a microtitre plate (5.3.1.14), beginning with the highest dilution. Add 0,1 ml of cell culture suspension (5.2.2.11) in such a density as to enable the formation of a monolayer (> 90 %) in at least 2 d in the cell control. In parallel six or eight wells do not receive any viral suspension and will serve as the cell control. The viral cytopathic effect (CPE) is read by using an inverted microscope after the appropriate incubation time (according to the virus type). 2) Virus titration on monolayers of cells on microtitre plates: Transfer 0,1 ml of each dilution into six or eight wells of a microtitre plate (5.3.1.14) containing a confluent (> 90 %) cell monolayer (5.2.2.11) without any medium. The last row of six or eight wells will receive 0,1 ml of culture medium (5.2.2.10) and will serve as the cell control. After 1 h of incubation at 37 °C, 0,1 ml of cell culture medium (5.2.2.10) is added to each well. Change pipettes for tubes or wells when adding medium. 3) Virus titration on monolayers of cells (5.2.2.11) in cell culture tubes or flasks: Item 2) applies with the modification that the volumes are multiplied by 5 to 10. b) Plaque assay (for poliovirus) Plastic tray wells (surface diameter 30 mm to 35 mm) with confluent cell monolayers (5.2.2.11) are washed once with PBS (5.2.2.3) and inoculated with 0,2 ml of serial dilutions of virus in maintenance medium [(5.2.2.10 b)]. Three wells are generally used per dilution. After an absorption period of 1 h at 37 °C, during which the cell monolayers are kept moist by tilting the dishes every 8 min to 10 min, the inoculum is removed and the cell monolayers are washed once with PBS (5.2.2.3). Subsequently, the wells are overlaid with 3 ml of a mixture consisting of melted agarose or another appropriate semisolid medium and 2 times concentrated MEM with 4 % FCS (5.2.2.5). The cultures are incubated for 2 to 3 d at 37 °C in a CO2 incubator (5.3.1.3). Plaques can be counted (C.2) after addition of 2 ml of a second overlay with the same composition of the first and also containing 5 % of a 1:1000 solution of neutral red (5.2.2.4) and further incubation (in the dark) at 37 °C for 24 h to 48 h in a CO2 incubator (5.3.1.3). Counting can be performed also after addition of crystal violet. The cell monolayers are fixed by adding 2 ml of 10 % TCA (5.2.2.6) over the agar overlay for 10 min to 15 min at room temperature. The agar overlay is then removed and 2 ml of 0,1 % crystal violet in 20 % ethanol are added. After 10 min to 15
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...