ISO 5910:2018
(Main)Cardiovascular implants and extracorporeal systems — Cardiac valve repair devices
Cardiovascular implants and extracorporeal systems — Cardiac valve repair devices
1.1 This document applies to all heart valve repair systems that have an intended use to repair and/or improve the function of native human heart valves by acting either on the valve apparatus or on the adjacent anatomy (e.g. ventricle, coronary sinus). 1.2 This document outlines an approach for verifying/validating the design and manufacture of a heart valve repair system through risk management. The selection of appropriate verification/validation tests and methods are derived from the risk assessment. The tests include assessments of the physical, chemical, biological, and mechanical properties of components and materials of heart valve repair systems. The tests also include preclinical in vivo evaluation and clinical investigation of the finished heart valve repair system to assess the safety and effectiveness of the heart valve repair system. NOTE For the purposes of this document, effectiveness endpoint includes clinical performance and benefits. 1.3 This document defines operational conditions and performance requirements for heart valve repair systems where adequate scientific and/or clinical evidence exists for their justification. 1.4 This document excludes Cardiac Resynchronization Therapy (CRT) devices, paravalvular leakage closure devices, systems that do not leave an implant in place (e.g. ablation, radio frequency annuloplasty), apical conduits and devices with components containing viable cells. This Standard also excludes materials not intended for repairing and/or improving the function of human heart valves according to its intended use (e.g. patch material and sutures used in general surgical practice). NOTE A rationale for the provisions of this document is given in Annex A.
Implants cardiovasculaires et circuits extra-corporels — Dispositifs de réparation de valves cardiaques
General Information
- Status
- Withdrawn
- Publication Date
- 30-May-2018
- Technical Committee
- ISO/TC 150/SC 2 - Cardiovascular implants and extracorporeal systems
- Drafting Committee
- ISO/TC 150/SC 2/WG 1 - Cardiac valves
- Current Stage
- 9599 - Withdrawal of International Standard
- Start Date
- 05-Jul-2024
- Completion Date
- 14-Feb-2026
Relations
- Revised
ISO 5910:2024 - Cardiovascular implants and extracorporeal systems — Cardiac valve repair devices - Effective Date
- 23-Apr-2020
Buy Documents
ISO 5910:2018 - Cardiovascular implants and extracorporeal systems — Cardiac valve repair devices Released:5/31/2018
ISO 5910:2018 - Cardiovascular implants and extracorporeal systems -- Cardiac valve repair devices
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
ISO 5910:2018 is a standard published by the International Organization for Standardization (ISO). Its full title is "Cardiovascular implants and extracorporeal systems — Cardiac valve repair devices". This standard covers: 1.1 This document applies to all heart valve repair systems that have an intended use to repair and/or improve the function of native human heart valves by acting either on the valve apparatus or on the adjacent anatomy (e.g. ventricle, coronary sinus). 1.2 This document outlines an approach for verifying/validating the design and manufacture of a heart valve repair system through risk management. The selection of appropriate verification/validation tests and methods are derived from the risk assessment. The tests include assessments of the physical, chemical, biological, and mechanical properties of components and materials of heart valve repair systems. The tests also include preclinical in vivo evaluation and clinical investigation of the finished heart valve repair system to assess the safety and effectiveness of the heart valve repair system. NOTE For the purposes of this document, effectiveness endpoint includes clinical performance and benefits. 1.3 This document defines operational conditions and performance requirements for heart valve repair systems where adequate scientific and/or clinical evidence exists for their justification. 1.4 This document excludes Cardiac Resynchronization Therapy (CRT) devices, paravalvular leakage closure devices, systems that do not leave an implant in place (e.g. ablation, radio frequency annuloplasty), apical conduits and devices with components containing viable cells. This Standard also excludes materials not intended for repairing and/or improving the function of human heart valves according to its intended use (e.g. patch material and sutures used in general surgical practice). NOTE A rationale for the provisions of this document is given in Annex A.
1.1 This document applies to all heart valve repair systems that have an intended use to repair and/or improve the function of native human heart valves by acting either on the valve apparatus or on the adjacent anatomy (e.g. ventricle, coronary sinus). 1.2 This document outlines an approach for verifying/validating the design and manufacture of a heart valve repair system through risk management. The selection of appropriate verification/validation tests and methods are derived from the risk assessment. The tests include assessments of the physical, chemical, biological, and mechanical properties of components and materials of heart valve repair systems. The tests also include preclinical in vivo evaluation and clinical investigation of the finished heart valve repair system to assess the safety and effectiveness of the heart valve repair system. NOTE For the purposes of this document, effectiveness endpoint includes clinical performance and benefits. 1.3 This document defines operational conditions and performance requirements for heart valve repair systems where adequate scientific and/or clinical evidence exists for their justification. 1.4 This document excludes Cardiac Resynchronization Therapy (CRT) devices, paravalvular leakage closure devices, systems that do not leave an implant in place (e.g. ablation, radio frequency annuloplasty), apical conduits and devices with components containing viable cells. This Standard also excludes materials not intended for repairing and/or improving the function of human heart valves according to its intended use (e.g. patch material and sutures used in general surgical practice). NOTE A rationale for the provisions of this document is given in Annex A.
ISO 5910:2018 is classified under the following ICS (International Classification for Standards) categories: 11.040.40 - Implants for surgery, prosthetics and orthotics. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO 5910:2018 has the following relationships with other standards: It is inter standard links to ISO 5910:2024. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
ISO 5910:2018 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
INTERNATIONAL ISO
STANDARD 5910
First edition
2018-06
Cardiovascular implants and
extracorporeal systems — Cardiac
valve repair devices
Implants cardiovasculaires et circuits extra-corporels — Dispositifs de
réparation de valves cardiaques
Reference number
©
ISO 2018
© ISO 2018
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting
on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address
below or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Fax: +41 22 749 09 47
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii © ISO 2018 – All rights reserved
Contents Page
Foreword .v
Introduction .vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 2
4 Abbreviations.11
5 Fundamental requirements .12
5.1 General .12
5.2 Risk management .12
6 Device description .13
6.1 Intended use/Indication for use .13
6.2 Design inputs .13
6.2.1 General.13
6.2.2 Operational specifications .13
6.2.3 Functional, performance and safety requirements .14
6.2.4 Usability .15
6.2.5 Packaging, labelling, and sterilization .16
6.3 Design outputs .16
6.4 Design transfer (manufacturing verification/validation) .16
7 Design verification testing and analysis / Design validation .16
7.1 General requirements .16
7.2 In vitro assessment .16
7.2.1 General.16
7.2.2 Test articles, sample selection, test conditions and reporting requirements .17
7.2.3 Device material property assessment .18
7.2.4 Functional performance assessment .19
7.2.5 Device structural performance assessment .19
7.2.6 Device corrosion assessment .20
7.2.7 Delivery system design evaluation requirements .20
7.2.8 Visibility.20
7.2.9 Simulated use assessment .20
7.2.10 Human factors / Usability assessment .21
7.2.11 Device MRI safety .21
7.2.12 Design specific testing .21
7.3 Preclinical in vivo evaluation .21
7.3.1 General.21
7.3.2 Overall requirements .21
7.3.3 Methods .23
7.3.4 Test report .24
7.4 Clinical Investigations .24
7.4.1 General.24
7.4.2 Study considerations .25
7.4.3 Study endpoints .28
7.4.4 Ethical considerations .28
7.4.5 Distribution of subjects and investigators .28
7.4.6 Statistical considerations including sample size and duration .29
7.4.7 Patient selection criteria .31
7.4.8 Clinical data requirements .31
7.4.9 Clinical investigation analysis and reporting .34
7.4.10 Post-market clinical follow-up .34
Annex A (informative) Rationale for the provisions of this document .36
Annex B (informative) Examples of heart valve repair devices and delivery systems .39
Annex C (normative) Packaging .45
Annex D (normative) Product labels, instructions for use, and training .46
Annex E (normative) Sterilization .49
Annex F (informative) Heart valve repair system characteristics .50
Annex G (informative) Heart valve repair system hazards, associated failure modes and
evaluation methods .52
Annex H (informative) In vitro test guidelines for paediatric devices .63
Annex I (informative) Examples and definitions of some physical and material properties
of heart valve repair device components .65
Annex J (informative) Examples of standards applicable to testing of materials and
components of heart valve repair devices .79
Annex K (informative) Considerations for device material properties undergoing
alterations post implantation .85
Annex L (informative) Corrosion assessment .86
Annex M (informative) Guidelines for in vitro evaluation of functional performance of the
repair .89
Annex N (informative) Durability testing .95
Annex O (informative) Fatigue assessment .97
Annex P (informative) Preclinical in vivo evaluation .103
Annex Q (normative) Adverse event classification during clinical investigation .106
Annex R (informative) Imaging protocol .112
Annex S (informative) Clinical investigation endpoints for valve repair devices: Suggestions
for endpoints and their timing .116
Annex T (informative) Additional device design evaluation requirements .120
Annex U (informative) Guidelines for delivery system design evaluation .122
Bibliography .124
iv © ISO 2018 – All rights reserved
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www .iso .org/directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received (see www .iso .org/patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation on the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to the
World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT) see the following
URL: www .iso .org/iso/foreword .html.
This document was prepared by ISO/TC 150, Implants for surgery, Subcommittee SC 2, Cardiovascular
implants and extracorporeal systems.
Introduction
No heart valve repair device is ideal. Therefore, a group of engineers, scientists, and clinicians, experts
well aware of the problems associated with heart valve repair devices and their development, has
prepared this document. This document specifies types of tests, test methods, and requirements for
test apparatus. It requires documentation of test methods and results. This document deals with those
areas that will ensure adequate mitigation of device-associated risks for patients and other users of
the device, facilitate quality assurance, aid the heart team in choosing a heart valve repair device, and
ensure that the device will be provided in a convenient and usable form. This document emphasizes
the need to specify and report types of in vitro testing, preclinical in vivo and clinical evaluations. It
describes the labels and packaging of the device. Such a process involving in vitro, preclinical in vivo
and clinical evaluations is intended to clarify the requirements prior to market release and to enable
prompt identification and management of any subsequent problems.
With regard to in vitro testing and reporting, apart from basic material testing for mechanical, physical,
chemical and biocompatibility characteristics, this document also covers important functional and
durability characteristics of heart valve repair devices and their accessories. This document does not
specify exact test methods for functional and durability testing but it offers guidelines for the test
apparatus.
This document should be revised, updated, and amended as knowledge and techniques in heart valve
repair device technology improve.
vi © ISO 2018 – All rights reserved
INTERNATIONAL STANDARD ISO 5910:2018(E)
Cardiovascular implants and extracorporeal systems —
Cardiac valve repair devices
1 Scope
1.1 This document applies to all heart valve repair systems that have an intended use to repair and/
or improve the function of native human heart valves by acting either on the valve apparatus or on the
adjacent anatomy (e.g. ventricle, coronary sinus).
1.2 This document outlines an approach for verifying/validating the design and manufacture of a
heart valve repair system through risk management. The selection of appropriate verification/validation
tests and methods are derived from the risk assessment. The tests include assessments of the physical,
chemical, biological, and mechanical properties of components and materials of heart valve repair
systems. The tests also include preclinical in vivo evaluation and clinical investigation of the finished
heart valve repair system to assess the safety and effectiveness of the heart valve repair system.
NOTE For the purposes of this document, effectiveness endpoint includes clinical performance and benefits.
1.3 This document defines operational conditions and performance requirements for heart valve
repair systems where adequate scientific and/or clinical evidence exists for their justification.
1.4 This document excludes Cardiac Resynchronization Therapy (CRT) devices, paravalvular
leakage closure devices, systems that do not leave an implant in place (e.g. ablation, radio frequency
annuloplasty), apical conduits and devices with components containing viable cells. This Standard also
excludes materials not intended for repairing and/or improving the function of human heart valves
according to its intended use (e.g. patch material and sutures used in general surgical practice).
NOTE A rationale for the provisions of this document is given in Annex A.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 10993-1, Biological evaluation of medical devices — Part 1: Evaluation and testing within a risk
management process
ISO 10993-2, Biological evaluation of medical devices — Part 2: Animal welfare requirements
ISO 11135, Sterilization of health-care products — Ethylene oxide — Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO 11137-1, Sterilization of health care products — Radiation — Part 1: Requirements for development,
validation and routine control of a sterilization process for medical devices
ISO 11137-2, Sterilization of health care products — Radiation — Part 2: Establishing the sterilization dose
ISO 11137-3, Sterilization of health care products — Radiation — Part 3: Guidance on dosimetric aspects of
development, validation and routine control
ISO 11607-1, Packaging for terminally sterilized medical devices — Part 1: Requirements for materials,
sterile barrier systems and packaging systems
ISO 11607-2, Packaging for terminally sterilized medical devices — Part 2: Validation requirements for
forming, sealing and assembly processes
ISO 13485, Medical devices — Quality management systems — Requirements for regulatory purposes
ISO 14155, Clinical investigation of medical devices for human subjects — Good clinical practice
ISO 14160, Sterilization of health care products — Liquid chemical sterilizing agents for single-use medical
devices utilizing animal tissues and their derivatives — Requirements for characterization, development,
validation and routine control of a sterilization process for medical devices
ISO 14630, Non-active surgical implants — General requirements
ISO 14937, Sterilization of health care products — General requirements for characterization of a sterilizing
agent and the development, validation and routine control of a sterilization process for medical devices
ISO 14971, Medical devices — Application of risk management to medical devices
ISO 15223-1, Medical devices — Symbols to be used with medical device labels, labelling and information to
be supplied — Part 1: General requirements
ISO 15223-2, Medical devices — Symbols to be used with medical device labels, labelling, and information
to be supplied — Part 2: Symbol development, selection and validation
ISO/IEC 17025, General requirements for the competence of testing and calibration laboratories
ISO 17664, Processing of health care products — Information to be provided by the medical device
manufacturer for the processing of medical devices
ISO 17665-1, Sterilization of health care products — Moist heat — Part 1: Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO/TS 17665-2, Sterilization of health care products — Moist heat — Part 2: Guidance on the application
of ISO 17665-1
ISO/TS 17665-3, Sterilization of health care products — Moist heat — Part 3: Guidance on the designation
of a medical device to a product family and processing category for steam sterilization
ISO 22442-1, Medical devices utilizing animal tissues and their derivatives — Part 1: Application of risk
management
ISO 22442-2, Medical devices utilizing animal tissues and their derivatives — Part 2: Controls on sourcing,
collection and handling
ISO 22442-3, Medical devices utilizing animal tissues and their derivatives — Part 3: Validation of the
elimination and/or inactivation of viruses and transmissible spongiform encephalopathy (TSE) agents
ISO/TR 22442-4, Medical devices utilizing animal tissues and their derivatives — Part 4: Principles for
elimination and/or inactivation of transmissible spongiform encephalopathy (TSE) agents and validation
assays for those processes
IEC 62366-1, Medical devices — Part 1: Application of usability engineering to medical devices
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— IEC Electropedia: available at http: //www .electropedia .org/
— ISO Online browsing platform: available at https: //www .iso .org/obp
2 © ISO 2018 – All rights reserved
NOTE Additional definitions can be found in the informative annexes.
3.1
abnormal use
act or omission of an act by the operator or user of a medical device as a result of conduct which is
beyond any means of risk control by the manufacturer
3.2
accessory
device-specific tool that is required to assist in the implantation and/or adjustment of the heart valve
repair device, excluding the delivery system
3.3
active comparator
active control
intervention generally accepted or demonstrated to be safe and effective for the condition of interest
that can be used as a basis of comparison of the safety and effectiveness of the heart valve repair device
Note 1 to entry: The active comparator is generally the standard of care for the condition.
3.4
actuarial analysis
statistical technique for calculating event rates over time
Note 1 to entry: Standard actuarial methods calculate the probability of freedom from events within pre-specified
intervals of time. When the intervals approach zero width, the methods are called Kaplan-Meier methods.
3.5
adverse event
AE
untoward medical occurrence, unintended disease or injury, or untoward clinical signs (including
abnormal laboratory findings) in subjects, users or other persons, whether or not related to the heart
valve repair device implantation, adjustment or procedure
3.6
auxiliary device
device used during the procedure, not including accessories (e.g. sheath, guidewire) and delivery system
3.7
back pressure
differential pressure applied across the valve during the closed phase
3.8
body surface area
BSA
total surface area (m ) of the human body
Note 1 to entry: This can be calculated as the square root of product of the weight in kg times the height in cm
divided by 3 600. See Reference [30].
3.9
cardiac index
2 2
cardiac output (3.10) (CO, l/min) divided by the body surface area (3.8) (BSA, m ), with units l/min/m
3.10
cardiac output
CO
stroke volume multiplied by heart rate
3.11
closing volume
portion of the regurgitant volume that is associated with the dynamics of the valve closure during a
single cycle
Note 1 to entry: See Figure 1.
Key
X time
Y flowrate
1 forward flow volume
2 closing volume
3 leakage volume
Figure 1 — Schematic representation of flow waveform and regurgitant volumes for one cycle
3.12
coating
thin-film material that is applied to an element of a heart valve repair device to modify its properties
3.13
compliance
4 © ISO 2018 – All rights reserved
relationship between change in radius and change in pressure of a deformable tubular structure (e.g.
valve annulus, aorta, conduit), defined in this document as:
()rr−×100
C=×100%
rp×−()p
12 1
where
C is the compliance in units of % radial change/100 mmHg;
p is the diastolic pressure, in mmHg;
p is the systolic pressure, in mmHg;
r is the inner radius at p , in millimetres;
1 1
r is the inner radius at p , in millimetres.
2 2
Note 1 to entry: See Reference [7].
3.14
component-joining material
material, such as a suture, adhesive or welding compound, used to assemble the components of a heart
valve repair device, thereby becoming part of the implanted device
3.15
cycle
one complete sequence in the action of a heart valve under pulsatile flow conditions
3.16
cycle rate
number of complete cycles per unit of time, usually expressed as cycles per minute (cycles/min)
3.17
delivery system
system used to deliver, deploy, attach or adjust the device in the implant site
3.18
design validation
establishment by objective evidence that device specifications conform with user needs and intended
use(s) (3.34)
3.19
design verification
establishment by objective evidence that the design output meets the design input requirements
3.20
device embolisation
dislodgement from the intended and documented original position to an unintended and nontherapeutic
location
3.21
device failure
inability of a device to perform its intended function sufficient to cause a hazard
3.22
device migration
unintended movement or displacement of the device from its original position within the implant site,
without embolisation
3.23
effective orifice area
EOA
orifice area that has been derived from flow and pressure or velocity data
Note 1 to entry: For in vitro testing, EOA is defined as:
q
v
RMS
EOA=
Dp
51,6×
ρ
where
EOA is the effective orifice area (cm );
is the root mean square forward flow (ml/s) during the positive differential pressure period;
q
v
RMS
Δp is the mean pressure difference (measured during the positive differential pressure peri-
od) (mmHg);
ρ is the density of the test fluid (g/cm ).
3.24
failure mode
mechanism of device failure (3.21)
3.25
follow-up
continued assessment of subjects who have received the heart valve repair device
3.26
forward flow volume
volume of flow ejected through the heart valve in the forward direction during one cycle, not including
any regurgitant flow through the valve
Note 1 to entry: See Figure 1.
3.27
fracture
complete separation of any part of the heart valve repair device (3.28) that was previously intact
3.28
heart valve repair device
implant (3.31) intended to improve the function of native human heart valves by acting either on the
valve apparatus or on the adjacent anatomy (e.g. ventricle, coronary sinus)
Note 1 to entry: See examples in Annex B.
3.29
heart valve repair system
heart valve repair device, delivery system, other accessories as applicable, packaging, labelling, and
instructions
3.30
imaging modality
method used to visualize and assess native anatomy and/or device position, geometry and/or function
3.31
implant
device placed surgically or non-surgically into the human body and intended to remain in place after
the procedure
6 © ISO 2018 – All rights reserved
3.32
implant site
location of heart valve repair device implantation or deployment
3.33
indication for use
clinical condition of the patient population that the heart valve repair device is intended to treat or
improve
3.34
intended use
purpose of a heart valve repair device, in accordance with the specifications, instructions, and
information provided by the manufacturer
3.35
Kaplan-Meier methods
statistical approaches to calculating event rates over time when the actual dates of events for each
person in the population are taken into account
3.36
leakage volume
component of the regurgitant volume that is associated with leakage during closed phase of a valve in a
single cycle
Note 1 to entry: See Figure 1. The point of separation between the closing and leakage volumes is obtained
according to a defined and stated criterion (the linear extrapolation shown in Figure 1 is just an example).
3.37
linearized rate
total number of events divided by the total time under evaluation
Note 1 to entry: Generally, the rate is expressed in terms of percent per patient year.
3.38
mean arterial pressure
time-averaged arithmetic mean value of the arterial pressure during one cycle
3.39
mean pressure difference
time-averaged arithmetic mean value of the pressure difference across a heart valve during the positive
differential pressure period of the cycle
Note 1 to entry: See Figure 2 for representative aortic and mitral flow and pressure waveforms. See Figure 3 for
representative pulmonary and tricuspid flow and pressure waveforms.
3.40
non-structural dysfunction
abnormality extrinsic to the heart valve repair device that results in abnormal function of the device or
causes clinical symptoms
3.41
pannus
ingrowth of tissue onto the heart valve repair device which may interfere with normal functioning
3.42
pull-out
situation in which the suture or anchoring device remains structurally intact but tears through the
tissue in which it is implanted
3.43
reference device
heart valve substitute or heart valve repair device with known clinical history used for comparative
preclinical and clinical evaluations
3.44
regurgitant fraction
regurgitant volume expressed as a percentage of the total ventricular stroke volume
3.45
regurgitant volume
volume of fluid that flows through a heart valve in the reverse direction during one cycle and is the sum
of the closing volume and leakage volume (3.36)
Note 1 to entry: See Figure 1.
3.46
repositioning
intentional change of implant position of a partially or fully deployed heart valve repair device
3.47
retrieval
removal of a partially or fully deployed heart valve repair device
3.48
risk
combination of the probability of occurrence of harm and the severity (3.53) of that harm
Note 1 to entry: See ISO 14971.
3.49
risk analysis
systematic use of available information to identify hazards and to estimate the associated risks (3.48)
Note 1 to entry: See ISO 14971.
3.50
risk assessment
overall process comprising a risk analysis (3.49) and a risk evaluation
Note 1 to entry: See ISO 14971.
3.51
root mean square forward flow
RMS forward flow
square root of the integral of the volume flow rate waveform squared during the positive differential
pressure interval of the forward flow phase used to calculate EOA
Note 1 to entry: Defining the time interval for flow and pressure measurement as the positive pressure period of
the forward flow interval for EOA computation provides repeatable and consistent results for comparison to the
minimum device performance requirements.
Note 2 to entry: This is calculated using the following equation:
t
qt dt
()
v
∫
t
q =
v
RMS
tt−
8 © ISO 2018 – All rights reserved
where
is the root mean square forward flow (ml/s) during the positive differential pressure period;
q
v
RMS
q (t) is the instantaneous flow at time t;
v
t is time at start of positive differential pressure period;
t is time at end of positive differential pressure period.
Note 3 to entry: The rationale for use of q is that the instantaneous pressure difference is proportional to
v
RMS
the square of instantaneous flow rate, and it is the mean pressure difference that is required.
Note 4 to entry: See Figure 2 for representative aortic and mitral flow and pressure waveforms from in vitro
testing. See Figure 3 for representative pulmonary and tricuspid flow and pressure waveforms from in vitro
testing.
Key
1 aortic pressure
2 left ventricular pressure
3 left atrial pressure
4 aortic flow rate
5 mitral flow rate
a
Positive pressure range.
b
q range.
v
RMS
Figure 2 — Schematic representation of aortic and mitral flow and pressure waveforms versus
time from in vitro testing
Key
1 pulmonary pressure
2 right ventricular pressure
3 right atrial pressure
4 pulmonary flow rate
5 tricuspid flow rate
a
Positive pressure range.
b
q range.
v
RMS
Figure 3 — Schematic representation of pulmonary and tricuspid flow and pressure waveforms
versus time from in vitro testing
3.52
safety
freedom from unacceptable risk
Note 1 to entry: See ISO 14971.
3.53
severity
measure of the possible consequences of a hazard
Note 1 to entry: See ISO 14971.
3.54
simulated cardiac output
forward flow volume multiplied by heart rate
Note 1 to entry: Simulated cardiac output applies to in vitro bench testing only in this document.
3.55
special process
process for which the product cannot be fully verified by inspection or test
3.56
sterility assurance level
SAL
probability of a single viable microorganism occurring on an item after sterilization
Note 1 to entry: The term SAL takes a quantitative value, generally 10−6 or 10−3. When applying this quantitative
value to assurance of sterility, an SAL of 10−6 has a lower value but provides a greater assurance of sterility than
an SAL of 10−3.
10 © ISO 2018 – All rights reserved
Note 2 to entry: See Reference [6].
3.57
sterilization
validated process used to render product free from viable microorganisms
Note 1 to entry: In a sterilization process, the nature of microbial inactivation is exponential and thus the survival
of a microorganism on an individual item can be expressed in terms of probability. While this probability can be
reduced to a very low number, it can never be reduced to zero.
Note 2 to entry: See Reference [6].
3.58
stroke volume
SV
volume of blood pumped by a ventricle in one contraction, which is equal to the difference between the
end diastolic ventricular volume and end systolic ventricular volume
3.59
structural device or component failure
degradation of structural integrity of the repair device (e.g. fractures) that results in the functional
performance of the implant no longer being acceptable and/or that results in adverse events (3.5)
3.60
structural native valve deterioration
structural native valve dysfunction
dysfunction or deterioration intrinsic to the native valve, including calcification, leaflet fibrosis, leaflet
tear or flail, resulting in stenosis or intra-prosthetic regurgitation
3.61
systolic duration
portion of cardiac cycle time corresponding to ventricular contraction
Note 1 to entry: For in vitro testing, systolic duration corresponds to the duration of forward flow in a cardiac cycle.
3.62
total product life cycle
period of time over which a product is developed, brought to market and eventually removed from
the market
3.63
usability
characteristic of the user interface that facilitates use and thereby establishes effectiveness, efficiency,
ease of user learning and user satisfaction in the intended use environment
3.64
use error
act or omission of an act that results in a different medical device response than intended by the
manufacturer or expected by the user
Note 1 to entry: Examples of use error include incorrect sizing, suboptimal positioning, structural distortion of
the device.
Note 2 to entry: An unexpected physiological response of the patient is not by itself considered use error.
4 Abbreviations
For the purposes of this document, the following abbreviations apply.
AE adverse event
AWT accelerated wear testing
CO cardiac output
CT computed tomography
CIP clinical investigation plan
CFD computational fluid dynamics
ECG electrocardiogram
EOA effective orifice area
FEA finite element analysis
IFU instructions for use
INR international normalized ratio
LV left ventricle, left ventricular
MAP mean arterial pressure
MRI magnetic resonance imaging
PET positron emission tomography
PMCF post-market clinical follow-up
SV stroke volume
TEE transoesophageal echocardiography
TTE transthoracic echocardiography
5 Fundamental requirements
5.1 General
The manufacturer shall determine, at all stages of the total product life cycle, the acceptability of the
product for clinical use.
5.2 Risk management
Risk management is the essential element for design and verification of medical devices. A risk-based
methodology challenges the manufacturer to continually evaluate known and theoretical risks of the
device, to develop the most appropriate methods for mitigating the risks of the device, and to implement
the appropriate test and analysis methods to demonstrate that the risks have been mitigated. The
manufacturer shall define, implement and document risk management activities in accordance
with ISO 14971. The risk analysis shall be an iterative process over the total product life cycle of the
device based on evolving knowledge of device performance. Annex G outlines a risk management
approach relevant to heart valve repair devices, and provides examples of potential approaches to risk
management. In addition, a list of potential hazards specific to the various types of heart valve repair
devices that can serve as the basis for a risk analysis is also provided.
12 © ISO 2018 – All rights reserved
6 Device description
6.1 Intended use/Indication for use
The manufacturer shall identify the pathophysiological condition(s) to be treated, the intended patient
population, and intended claims.
6.2 Design inputs
6.2.1 General
The design attribute requirements of ISO 14630 shall apply.
6.2.2 Operational specifications
The manufacturer shall define the operational specifications for the system, including the principles of
operation, intended device delivery approach if applicable, expected device lifetime, shelf life, shipping/
storage limits, and the physiological environment in which it is intended to function. The manufacturer
shall define all relevant dimensional parameters that will be required to accurately select the size of
device to be implanted, if applicable. Table 1 and Table 2 define the expected physiological parameters
of the intended adult patient population for heart valve repair devices for both normal and pathological
patient conditions. See Annex H for guidelines regarding suggested test conditions for the paediatric
population.
Table 1 — Heart valve repair device operational environment for left side of heart — Adult
population
Parameter General Condition
Surrounding medium Human heart/Human blood
Temperature 34 °C to 42 °C
Heart rate 30 bpm to 200 bpm
Cardiac output 3 l/min to 15 l/min
Forward flow volume 25 ml to 100 ml
Peak differential pressure across
Aortic peak Aortic end
a
Pressures and result- closed valve
systolic diastolic
ant pressure loads by
pressure pressure
Aortic ΔP Mitral ΔP
A M
patient condition
mmHg mmHg
mmHg mmHg
Normotensive 90 to 140 60 to 90 80 to 115 90 to 140
Hypotensive <90 <60 <80 <90
Mild hypertensive 140 to 159 90 to 99 115 to 129 140 to 159
Moderate hypertensive 160 to 179 100 to 109 130 to 144 160 to 179
Severe hypertensive 180 to 209 110 to 119 145 to 164 180 to 209
Very severe hypertensive ≥210 ≥120 ≥165 ≥210
a
Peak differential pressure across closed aortic valve estimated using the following relationship:
— ΔP ≈ pressure associated with dicrotic notch assuming LV pressure is zero ≈ Aortic end diastolic
A
pressure + ½(Aortic peak systolic pressure – Aortic end diastolic pressure).
Peak differential pressure across closed mitral valve estimated to be equivalent to Aortic peak
systolic pressure.
Pressure values obtained from references (See references [28], [33]).
Table 2 — Heart valve repair devices operational environment for right side of heart – Adult
population
Parameter General Condition
Surrounding medium Human heart/Human blood
Temperature 34 °C to 42 °C
Heart rate 30 bpm to 200 bpm
Cardiac output 3 l/min to 15 l/min
Forward flow volume 25 ml to 100 ml
Pulmonary Peak differential pressure across
Pulmonary ar-
a
artery end closed valve
Pressures and resultant
tery peak sys-
diastolic
pressure loads by patient
tolic pressure
Pulmonary ΔP Tricuspid ΔP
P T
pressure
condition
mmHg
mmHg mmHg
mmHg
Normotensive 18 to 35 8 to 15 13 to 28 18 to 35
Hypotensive <18 <8 <13 <18
Mild hypertensive 35 to 49 15 to 19 28 to 34 35 to 49
Moderate hypertensive 50 to 59 20 to 24 35 to 42 50 to 59
Severe hypertensive 60 to 84 25 to 34 43 to 59 60 to 84
Very severe hypertensive ≥85 ≥35 ≥60 ≥85
a
Peak differe
...
INTERNATIONAL ISO
STANDARD 5910
First edition
2018-06
Cardiovascular implants and
extracorporeal systems — Cardiac
valve repair devices
Implants cardiovasculaires et circuits extra-corporels — Dispositifs de
réparation de valves cardiaques
Reference number
©
ISO 2018
© ISO 2018
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting
on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address
below or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Fax: +41 22 749 09 47
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii © ISO 2018 – All rights reserved
Contents Page
Foreword .v
Introduction .vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 2
4 Abbreviations.11
5 Fundamental requirements .12
5.1 General .12
5.2 Risk management .12
6 Device description .13
6.1 Intended use/Indication for use .13
6.2 Design inputs .13
6.2.1 General.13
6.2.2 Operational specifications .13
6.2.3 Functional, performance and safety requirements .14
6.2.4 Usability .15
6.2.5 Packaging, labelling, and sterilization .16
6.3 Design outputs .16
6.4 Design transfer (manufacturing verification/validation) .16
7 Design verification testing and analysis / Design validation .16
7.1 General requirements .16
7.2 In vitro assessment .16
7.2.1 General.16
7.2.2 Test articles, sample selection, test conditions and reporting requirements .17
7.2.3 Device material property assessment .18
7.2.4 Functional performance assessment .19
7.2.5 Device structural performance assessment .19
7.2.6 Device corrosion assessment .20
7.2.7 Delivery system design evaluation requirements .20
7.2.8 Visibility.20
7.2.9 Simulated use assessment .20
7.2.10 Human factors / Usability assessment .21
7.2.11 Device MRI safety .21
7.2.12 Design specific testing .21
7.3 Preclinical in vivo evaluation .21
7.3.1 General.21
7.3.2 Overall requirements .21
7.3.3 Methods .23
7.3.4 Test report .24
7.4 Clinical Investigations .24
7.4.1 General.24
7.4.2 Study considerations .25
7.4.3 Study endpoints .28
7.4.4 Ethical considerations .28
7.4.5 Distribution of subjects and investigators .28
7.4.6 Statistical considerations including sample size and duration .29
7.4.7 Patient selection criteria .31
7.4.8 Clinical data requirements .31
7.4.9 Clinical investigation analysis and reporting .34
7.4.10 Post-market clinical follow-up .34
Annex A (informative) Rationale for the provisions of this document .36
Annex B (informative) Examples of heart valve repair devices and delivery systems .39
Annex C (normative) Packaging .45
Annex D (normative) Product labels, instructions for use, and training .46
Annex E (normative) Sterilization .49
Annex F (informative) Heart valve repair system characteristics .50
Annex G (informative) Heart valve repair system hazards, associated failure modes and
evaluation methods .52
Annex H (informative) In vitro test guidelines for paediatric devices .63
Annex I (informative) Examples and definitions of some physical and material properties
of heart valve repair device components .65
Annex J (informative) Examples of standards applicable to testing of materials and
components of heart valve repair devices .79
Annex K (informative) Considerations for device material properties undergoing
alterations post implantation .85
Annex L (informative) Corrosion assessment .86
Annex M (informative) Guidelines for in vitro evaluation of functional performance of the
repair .89
Annex N (informative) Durability testing .95
Annex O (informative) Fatigue assessment .97
Annex P (informative) Preclinical in vivo evaluation .103
Annex Q (normative) Adverse event classification during clinical investigation .106
Annex R (informative) Imaging protocol .112
Annex S (informative) Clinical investigation endpoints for valve repair devices: Suggestions
for endpoints and their timing .116
Annex T (informative) Additional device design evaluation requirements .120
Annex U (informative) Guidelines for delivery system design evaluation .122
Bibliography .124
iv © ISO 2018 – All rights reserved
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www .iso .org/directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received (see www .iso .org/patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation on the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to the
World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT) see the following
URL: www .iso .org/iso/foreword .html.
This document was prepared by ISO/TC 150, Implants for surgery, Subcommittee SC 2, Cardiovascular
implants and extracorporeal systems.
Introduction
No heart valve repair device is ideal. Therefore, a group of engineers, scientists, and clinicians, experts
well aware of the problems associated with heart valve repair devices and their development, has
prepared this document. This document specifies types of tests, test methods, and requirements for
test apparatus. It requires documentation of test methods and results. This document deals with those
areas that will ensure adequate mitigation of device-associated risks for patients and other users of
the device, facilitate quality assurance, aid the heart team in choosing a heart valve repair device, and
ensure that the device will be provided in a convenient and usable form. This document emphasizes
the need to specify and report types of in vitro testing, preclinical in vivo and clinical evaluations. It
describes the labels and packaging of the device. Such a process involving in vitro, preclinical in vivo
and clinical evaluations is intended to clarify the requirements prior to market release and to enable
prompt identification and management of any subsequent problems.
With regard to in vitro testing and reporting, apart from basic material testing for mechanical, physical,
chemical and biocompatibility characteristics, this document also covers important functional and
durability characteristics of heart valve repair devices and their accessories. This document does not
specify exact test methods for functional and durability testing but it offers guidelines for the test
apparatus.
This document should be revised, updated, and amended as knowledge and techniques in heart valve
repair device technology improve.
vi © ISO 2018 – All rights reserved
INTERNATIONAL STANDARD ISO 5910:2018(E)
Cardiovascular implants and extracorporeal systems —
Cardiac valve repair devices
1 Scope
1.1 This document applies to all heart valve repair systems that have an intended use to repair and/
or improve the function of native human heart valves by acting either on the valve apparatus or on the
adjacent anatomy (e.g. ventricle, coronary sinus).
1.2 This document outlines an approach for verifying/validating the design and manufacture of a
heart valve repair system through risk management. The selection of appropriate verification/validation
tests and methods are derived from the risk assessment. The tests include assessments of the physical,
chemical, biological, and mechanical properties of components and materials of heart valve repair
systems. The tests also include preclinical in vivo evaluation and clinical investigation of the finished
heart valve repair system to assess the safety and effectiveness of the heart valve repair system.
NOTE For the purposes of this document, effectiveness endpoint includes clinical performance and benefits.
1.3 This document defines operational conditions and performance requirements for heart valve
repair systems where adequate scientific and/or clinical evidence exists for their justification.
1.4 This document excludes Cardiac Resynchronization Therapy (CRT) devices, paravalvular
leakage closure devices, systems that do not leave an implant in place (e.g. ablation, radio frequency
annuloplasty), apical conduits and devices with components containing viable cells. This Standard also
excludes materials not intended for repairing and/or improving the function of human heart valves
according to its intended use (e.g. patch material and sutures used in general surgical practice).
NOTE A rationale for the provisions of this document is given in Annex A.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 10993-1, Biological evaluation of medical devices — Part 1: Evaluation and testing within a risk
management process
ISO 10993-2, Biological evaluation of medical devices — Part 2: Animal welfare requirements
ISO 11135, Sterilization of health-care products — Ethylene oxide — Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO 11137-1, Sterilization of health care products — Radiation — Part 1: Requirements for development,
validation and routine control of a sterilization process for medical devices
ISO 11137-2, Sterilization of health care products — Radiation — Part 2: Establishing the sterilization dose
ISO 11137-3, Sterilization of health care products — Radiation — Part 3: Guidance on dosimetric aspects of
development, validation and routine control
ISO 11607-1, Packaging for terminally sterilized medical devices — Part 1: Requirements for materials,
sterile barrier systems and packaging systems
ISO 11607-2, Packaging for terminally sterilized medical devices — Part 2: Validation requirements for
forming, sealing and assembly processes
ISO 13485, Medical devices — Quality management systems — Requirements for regulatory purposes
ISO 14155, Clinical investigation of medical devices for human subjects — Good clinical practice
ISO 14160, Sterilization of health care products — Liquid chemical sterilizing agents for single-use medical
devices utilizing animal tissues and their derivatives — Requirements for characterization, development,
validation and routine control of a sterilization process for medical devices
ISO 14630, Non-active surgical implants — General requirements
ISO 14937, Sterilization of health care products — General requirements for characterization of a sterilizing
agent and the development, validation and routine control of a sterilization process for medical devices
ISO 14971, Medical devices — Application of risk management to medical devices
ISO 15223-1, Medical devices — Symbols to be used with medical device labels, labelling and information to
be supplied — Part 1: General requirements
ISO 15223-2, Medical devices — Symbols to be used with medical device labels, labelling, and information
to be supplied — Part 2: Symbol development, selection and validation
ISO/IEC 17025, General requirements for the competence of testing and calibration laboratories
ISO 17664, Processing of health care products — Information to be provided by the medical device
manufacturer for the processing of medical devices
ISO 17665-1, Sterilization of health care products — Moist heat — Part 1: Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO/TS 17665-2, Sterilization of health care products — Moist heat — Part 2: Guidance on the application
of ISO 17665-1
ISO/TS 17665-3, Sterilization of health care products — Moist heat — Part 3: Guidance on the designation
of a medical device to a product family and processing category for steam sterilization
ISO 22442-1, Medical devices utilizing animal tissues and their derivatives — Part 1: Application of risk
management
ISO 22442-2, Medical devices utilizing animal tissues and their derivatives — Part 2: Controls on sourcing,
collection and handling
ISO 22442-3, Medical devices utilizing animal tissues and their derivatives — Part 3: Validation of the
elimination and/or inactivation of viruses and transmissible spongiform encephalopathy (TSE) agents
ISO/TR 22442-4, Medical devices utilizing animal tissues and their derivatives — Part 4: Principles for
elimination and/or inactivation of transmissible spongiform encephalopathy (TSE) agents and validation
assays for those processes
IEC 62366-1, Medical devices — Part 1: Application of usability engineering to medical devices
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— IEC Electropedia: available at http: //www .electropedia .org/
— ISO Online browsing platform: available at https: //www .iso .org/obp
2 © ISO 2018 – All rights reserved
NOTE Additional definitions can be found in the informative annexes.
3.1
abnormal use
act or omission of an act by the operator or user of a medical device as a result of conduct which is
beyond any means of risk control by the manufacturer
3.2
accessory
device-specific tool that is required to assist in the implantation and/or adjustment of the heart valve
repair device, excluding the delivery system
3.3
active comparator
active control
intervention generally accepted or demonstrated to be safe and effective for the condition of interest
that can be used as a basis of comparison of the safety and effectiveness of the heart valve repair device
Note 1 to entry: The active comparator is generally the standard of care for the condition.
3.4
actuarial analysis
statistical technique for calculating event rates over time
Note 1 to entry: Standard actuarial methods calculate the probability of freedom from events within pre-specified
intervals of time. When the intervals approach zero width, the methods are called Kaplan-Meier methods.
3.5
adverse event
AE
untoward medical occurrence, unintended disease or injury, or untoward clinical signs (including
abnormal laboratory findings) in subjects, users or other persons, whether or not related to the heart
valve repair device implantation, adjustment or procedure
3.6
auxiliary device
device used during the procedure, not including accessories (e.g. sheath, guidewire) and delivery system
3.7
back pressure
differential pressure applied across the valve during the closed phase
3.8
body surface area
BSA
total surface area (m ) of the human body
Note 1 to entry: This can be calculated as the square root of product of the weight in kg times the height in cm
divided by 3 600. See Reference [30].
3.9
cardiac index
2 2
cardiac output (3.10) (CO, l/min) divided by the body surface area (3.8) (BSA, m ), with units l/min/m
3.10
cardiac output
CO
stroke volume multiplied by heart rate
3.11
closing volume
portion of the regurgitant volume that is associated with the dynamics of the valve closure during a
single cycle
Note 1 to entry: See Figure 1.
Key
X time
Y flowrate
1 forward flow volume
2 closing volume
3 leakage volume
Figure 1 — Schematic representation of flow waveform and regurgitant volumes for one cycle
3.12
coating
thin-film material that is applied to an element of a heart valve repair device to modify its properties
3.13
compliance
4 © ISO 2018 – All rights reserved
relationship between change in radius and change in pressure of a deformable tubular structure (e.g.
valve annulus, aorta, conduit), defined in this document as:
()rr−×100
C=×100%
rp×−()p
12 1
where
C is the compliance in units of % radial change/100 mmHg;
p is the diastolic pressure, in mmHg;
p is the systolic pressure, in mmHg;
r is the inner radius at p , in millimetres;
1 1
r is the inner radius at p , in millimetres.
2 2
Note 1 to entry: See Reference [7].
3.14
component-joining material
material, such as a suture, adhesive or welding compound, used to assemble the components of a heart
valve repair device, thereby becoming part of the implanted device
3.15
cycle
one complete sequence in the action of a heart valve under pulsatile flow conditions
3.16
cycle rate
number of complete cycles per unit of time, usually expressed as cycles per minute (cycles/min)
3.17
delivery system
system used to deliver, deploy, attach or adjust the device in the implant site
3.18
design validation
establishment by objective evidence that device specifications conform with user needs and intended
use(s) (3.34)
3.19
design verification
establishment by objective evidence that the design output meets the design input requirements
3.20
device embolisation
dislodgement from the intended and documented original position to an unintended and nontherapeutic
location
3.21
device failure
inability of a device to perform its intended function sufficient to cause a hazard
3.22
device migration
unintended movement or displacement of the device from its original position within the implant site,
without embolisation
3.23
effective orifice area
EOA
orifice area that has been derived from flow and pressure or velocity data
Note 1 to entry: For in vitro testing, EOA is defined as:
q
v
RMS
EOA=
Dp
51,6×
ρ
where
EOA is the effective orifice area (cm );
is the root mean square forward flow (ml/s) during the positive differential pressure period;
q
v
RMS
Δp is the mean pressure difference (measured during the positive differential pressure peri-
od) (mmHg);
ρ is the density of the test fluid (g/cm ).
3.24
failure mode
mechanism of device failure (3.21)
3.25
follow-up
continued assessment of subjects who have received the heart valve repair device
3.26
forward flow volume
volume of flow ejected through the heart valve in the forward direction during one cycle, not including
any regurgitant flow through the valve
Note 1 to entry: See Figure 1.
3.27
fracture
complete separation of any part of the heart valve repair device (3.28) that was previously intact
3.28
heart valve repair device
implant (3.31) intended to improve the function of native human heart valves by acting either on the
valve apparatus or on the adjacent anatomy (e.g. ventricle, coronary sinus)
Note 1 to entry: See examples in Annex B.
3.29
heart valve repair system
heart valve repair device, delivery system, other accessories as applicable, packaging, labelling, and
instructions
3.30
imaging modality
method used to visualize and assess native anatomy and/or device position, geometry and/or function
3.31
implant
device placed surgically or non-surgically into the human body and intended to remain in place after
the procedure
6 © ISO 2018 – All rights reserved
3.32
implant site
location of heart valve repair device implantation or deployment
3.33
indication for use
clinical condition of the patient population that the heart valve repair device is intended to treat or
improve
3.34
intended use
purpose of a heart valve repair device, in accordance with the specifications, instructions, and
information provided by the manufacturer
3.35
Kaplan-Meier methods
statistical approaches to calculating event rates over time when the actual dates of events for each
person in the population are taken into account
3.36
leakage volume
component of the regurgitant volume that is associated with leakage during closed phase of a valve in a
single cycle
Note 1 to entry: See Figure 1. The point of separation between the closing and leakage volumes is obtained
according to a defined and stated criterion (the linear extrapolation shown in Figure 1 is just an example).
3.37
linearized rate
total number of events divided by the total time under evaluation
Note 1 to entry: Generally, the rate is expressed in terms of percent per patient year.
3.38
mean arterial pressure
time-averaged arithmetic mean value of the arterial pressure during one cycle
3.39
mean pressure difference
time-averaged arithmetic mean value of the pressure difference across a heart valve during the positive
differential pressure period of the cycle
Note 1 to entry: See Figure 2 for representative aortic and mitral flow and pressure waveforms. See Figure 3 for
representative pulmonary and tricuspid flow and pressure waveforms.
3.40
non-structural dysfunction
abnormality extrinsic to the heart valve repair device that results in abnormal function of the device or
causes clinical symptoms
3.41
pannus
ingrowth of tissue onto the heart valve repair device which may interfere with normal functioning
3.42
pull-out
situation in which the suture or anchoring device remains structurally intact but tears through the
tissue in which it is implanted
3.43
reference device
heart valve substitute or heart valve repair device with known clinical history used for comparative
preclinical and clinical evaluations
3.44
regurgitant fraction
regurgitant volume expressed as a percentage of the total ventricular stroke volume
3.45
regurgitant volume
volume of fluid that flows through a heart valve in the reverse direction during one cycle and is the sum
of the closing volume and leakage volume (3.36)
Note 1 to entry: See Figure 1.
3.46
repositioning
intentional change of implant position of a partially or fully deployed heart valve repair device
3.47
retrieval
removal of a partially or fully deployed heart valve repair device
3.48
risk
combination of the probability of occurrence of harm and the severity (3.53) of that harm
Note 1 to entry: See ISO 14971.
3.49
risk analysis
systematic use of available information to identify hazards and to estimate the associated risks (3.48)
Note 1 to entry: See ISO 14971.
3.50
risk assessment
overall process comprising a risk analysis (3.49) and a risk evaluation
Note 1 to entry: See ISO 14971.
3.51
root mean square forward flow
RMS forward flow
square root of the integral of the volume flow rate waveform squared during the positive differential
pressure interval of the forward flow phase used to calculate EOA
Note 1 to entry: Defining the time interval for flow and pressure measurement as the positive pressure period of
the forward flow interval for EOA computation provides repeatable and consistent results for comparison to the
minimum device performance requirements.
Note 2 to entry: This is calculated using the following equation:
t
qt dt
()
v
∫
t
q =
v
RMS
tt−
8 © ISO 2018 – All rights reserved
where
is the root mean square forward flow (ml/s) during the positive differential pressure period;
q
v
RMS
q (t) is the instantaneous flow at time t;
v
t is time at start of positive differential pressure period;
t is time at end of positive differential pressure period.
Note 3 to entry: The rationale for use of q is that the instantaneous pressure difference is proportional to
v
RMS
the square of instantaneous flow rate, and it is the mean pressure difference that is required.
Note 4 to entry: See Figure 2 for representative aortic and mitral flow and pressure waveforms from in vitro
testing. See Figure 3 for representative pulmonary and tricuspid flow and pressure waveforms from in vitro
testing.
Key
1 aortic pressure
2 left ventricular pressure
3 left atrial pressure
4 aortic flow rate
5 mitral flow rate
a
Positive pressure range.
b
q range.
v
RMS
Figure 2 — Schematic representation of aortic and mitral flow and pressure waveforms versus
time from in vitro testing
Key
1 pulmonary pressure
2 right ventricular pressure
3 right atrial pressure
4 pulmonary flow rate
5 tricuspid flow rate
a
Positive pressure range.
b
q range.
v
RMS
Figure 3 — Schematic representation of pulmonary and tricuspid flow and pressure waveforms
versus time from in vitro testing
3.52
safety
freedom from unacceptable risk
Note 1 to entry: See ISO 14971.
3.53
severity
measure of the possible consequences of a hazard
Note 1 to entry: See ISO 14971.
3.54
simulated cardiac output
forward flow volume multiplied by heart rate
Note 1 to entry: Simulated cardiac output applies to in vitro bench testing only in this document.
3.55
special process
process for which the product cannot be fully verified by inspection or test
3.56
sterility assurance level
SAL
probability of a single viable microorganism occurring on an item after sterilization
Note 1 to entry: The term SAL takes a quantitative value, generally 10−6 or 10−3. When applying this quantitative
value to assurance of sterility, an SAL of 10−6 has a lower value but provides a greater assurance of sterility than
an SAL of 10−3.
10 © ISO 2018 – All rights reserved
Note 2 to entry: See Reference [6].
3.57
sterilization
validated process used to render product free from viable microorganisms
Note 1 to entry: In a sterilization process, the nature of microbial inactivation is exponential and thus the survival
of a microorganism on an individual item can be expressed in terms of probability. While this probability can be
reduced to a very low number, it can never be reduced to zero.
Note 2 to entry: See Reference [6].
3.58
stroke volume
SV
volume of blood pumped by a ventricle in one contraction, which is equal to the difference between the
end diastolic ventricular volume and end systolic ventricular volume
3.59
structural device or component failure
degradation of structural integrity of the repair device (e.g. fractures) that results in the functional
performance of the implant no longer being acceptable and/or that results in adverse events (3.5)
3.60
structural native valve deterioration
structural native valve dysfunction
dysfunction or deterioration intrinsic to the native valve, including calcification, leaflet fibrosis, leaflet
tear or flail, resulting in stenosis or intra-prosthetic regurgitation
3.61
systolic duration
portion of cardiac cycle time corresponding to ventricular contraction
Note 1 to entry: For in vitro testing, systolic duration corresponds to the duration of forward flow in a cardiac cycle.
3.62
total product life cycle
period of time over which a product is developed, brought to market and eventually removed from
the market
3.63
usability
characteristic of the user interface that facilitates use and thereby establishes effectiveness, efficiency,
ease of user learning and user satisfaction in the intended use environment
3.64
use error
act or omission of an act that results in a different medical device response than intended by the
manufacturer or expected by the user
Note 1 to entry: Examples of use error include incorrect sizing, suboptimal positioning, structural distortion of
the device.
Note 2 to entry: An unexpected physiological response of the patient is not by itself considered use error.
4 Abbreviations
For the purposes of this document, the following abbreviations apply.
AE adverse event
AWT accelerated wear testing
CO cardiac output
CT computed tomography
CIP clinical investigation plan
CFD computational fluid dynamics
ECG electrocardiogram
EOA effective orifice area
FEA finite element analysis
IFU instructions for use
INR international normalized ratio
LV left ventricle, left ventricular
MAP mean arterial pressure
MRI magnetic resonance imaging
PET positron emission tomography
PMCF post-market clinical follow-up
SV stroke volume
TEE transoesophageal echocardiography
TTE transthoracic echocardiography
5 Fundamental requirements
5.1 General
The manufacturer shall determine, at all stages of the total product life cycle, the acceptability of the
product for clinical use.
5.2 Risk management
Risk management is the essential element for design and verification of medical devices. A risk-based
methodology challenges the manufacturer to continually evaluate known and theoretical risks of the
device, to develop the most appropriate methods for mitigating the risks of the device, and to implement
the appropriate test and analysis methods to demonstrate that the risks have been mitigated. The
manufacturer shall define, implement and document risk management activities in accordance
with ISO 14971. The risk analysis shall be an iterative process over the total product life cycle of the
device based on evolving knowledge of device performance. Annex G outlines a risk management
approach relevant to heart valve repair devices, and provides examples of potential approaches to risk
management. In addition, a list of potential hazards specific to the various types of heart valve repair
devices that can serve as the basis for a risk analysis is also provided.
12 © ISO 2018 – All rights reserved
6 Device description
6.1 Intended use/Indication for use
The manufacturer shall identify the pathophysiological condition(s) to be treated, the intended patient
population, and intended claims.
6.2 Design inputs
6.2.1 General
The design attribute requirements of ISO 14630 shall apply.
6.2.2 Operational specifications
The manufacturer shall define the operational specifications for the system, including the principles of
operation, intended device delivery approach if applicable, expected device lifetime, shelf life, shipping/
storage limits, and the physiological environment in which it is intended to function. The manufacturer
shall define all relevant dimensional parameters that will be required to accurately select the size of
device to be implanted, if applicable. Table 1 and Table 2 define the expected physiological parameters
of the intended adult patient population for heart valve repair devices for both normal and pathological
patient conditions. See Annex H for guidelines regarding suggested test conditions for the paediatric
population.
Table 1 — Heart valve repair device operational environment for left side of heart — Adult
population
Parameter General Condition
Surrounding medium Human heart/Human blood
Temperature 34 °C to 42 °C
Heart rate 30 bpm to 200 bpm
Cardiac output 3 l/min to 15 l/min
Forward flow volume 25 ml to 100 ml
Peak differential pressure across
Aortic peak Aortic end
a
Pressures and result- closed valve
systolic diastolic
ant pressure loads by
pressure pressure
Aortic ΔP Mitral ΔP
A M
patient condition
mmHg mmHg
mmHg mmHg
Normotensive 90 to 140 60 to 90 80 to 115 90 to 140
Hypotensive <90 <60 <80 <90
Mild hypertensive 140 to 159 90 to 99 115 to 129 140 to 159
Moderate hypertensive 160 to 179 100 to 109 130 to 144 160 to 179
Severe hypertensive 180 to 209 110 to 119 145 to 164 180 to 209
Very severe hypertensive ≥210 ≥120 ≥165 ≥210
a
Peak differential pressure across closed aortic valve estimated using the following relationship:
— ΔP ≈ pressure associated with dicrotic notch assuming LV pressure is zero ≈ Aortic end diastolic
A
pressure + ½(Aortic peak systolic pressure – Aortic end diastolic pressure).
Peak differential pressure across closed mitral valve estimated to be equivalent to Aortic peak
systolic pressure.
Pressure values obtained from references (See references [28], [33]).
Table 2 — Heart valve repair devices operational environment for right side of heart – Adult
population
Parameter General Condition
Surrounding medium Human heart/Human blood
Temperature 34 °C to 42 °C
Heart rate 30 bpm to 200 bpm
Cardiac output 3 l/min to 15 l/min
Forward flow volume 25 ml to 100 ml
Pulmonary Peak differential pressure across
Pulmonary ar-
a
artery end closed valve
Pressures and resultant
tery peak sys-
diastolic
pressure loads by patient
tolic pressure
Pulmonary ΔP Tricuspid ΔP
P T
pressure
condition
mmHg
mmHg mmHg
mmHg
Normotensive 18 to 35 8 to 15 13 to 28 18 to 35
Hypotensive <18 <8 <13 <18
Mild hypertensive 35 to 49 15 to 19 28 to 34 35 to 49
Moderate hypertensive 50 to 59 20 to 24 35 to 42 50 to 59
Severe hypertensive 60 to 84 25 to 34 43 to 59 60 to 84
Very severe hypertensive ≥85 ≥35 ≥60 ≥85
a
Peak differe
...
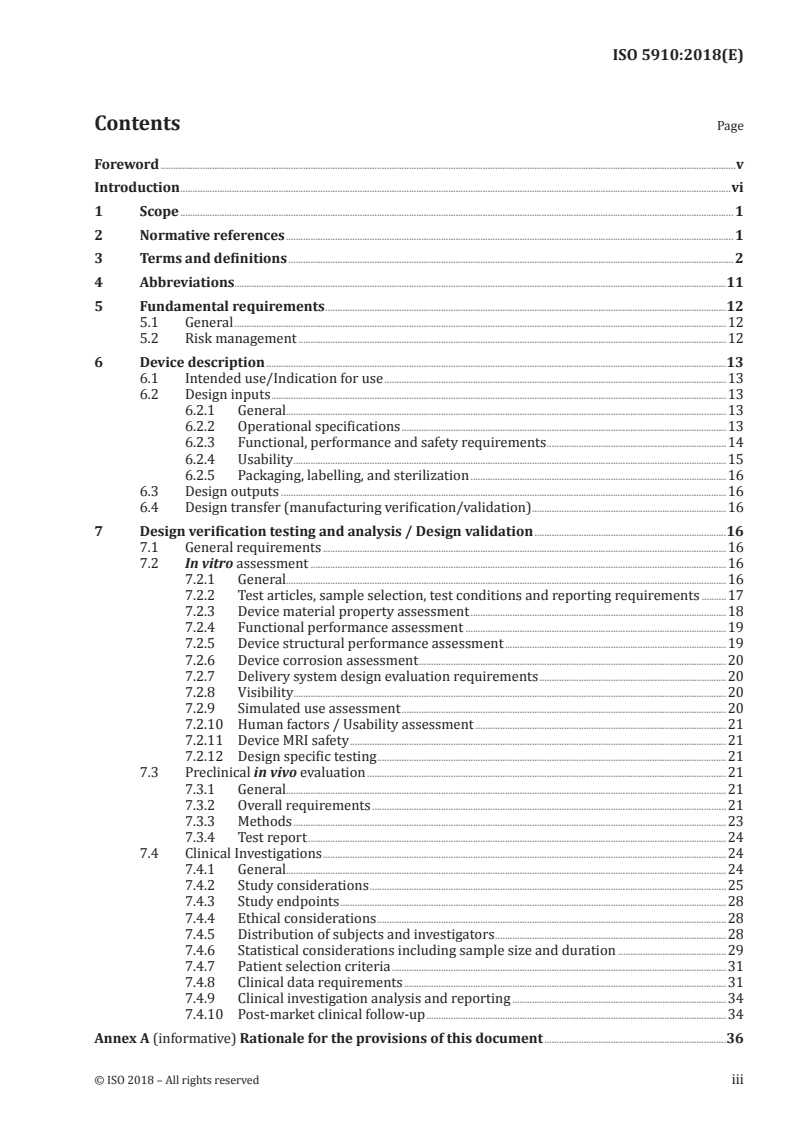
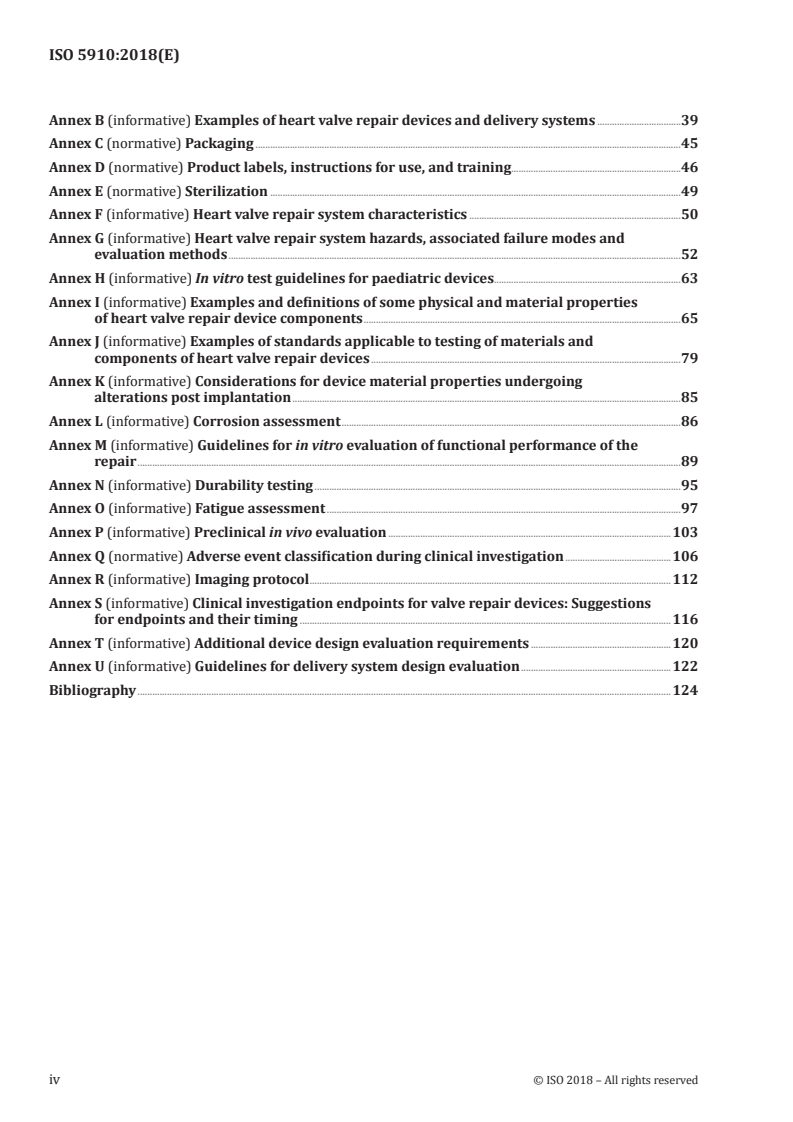
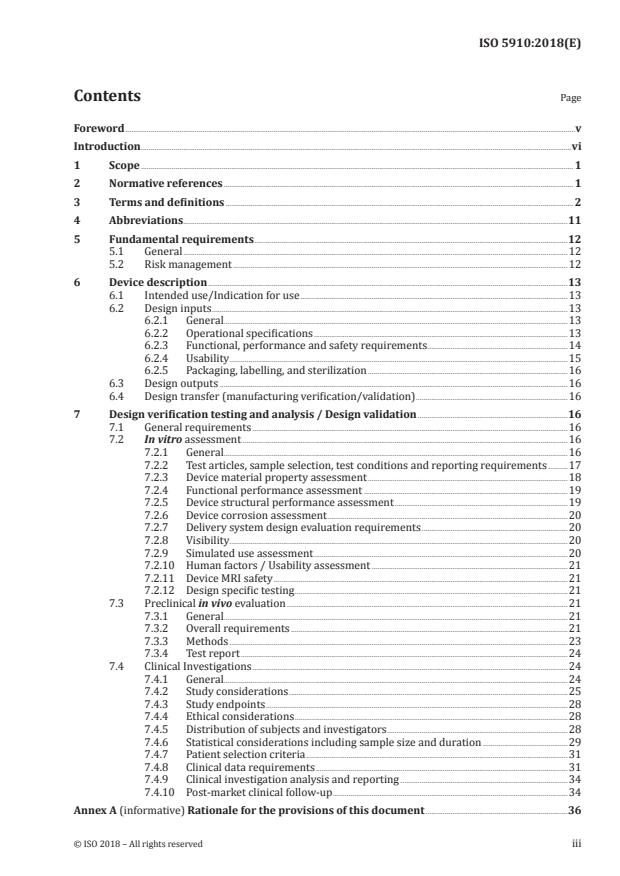
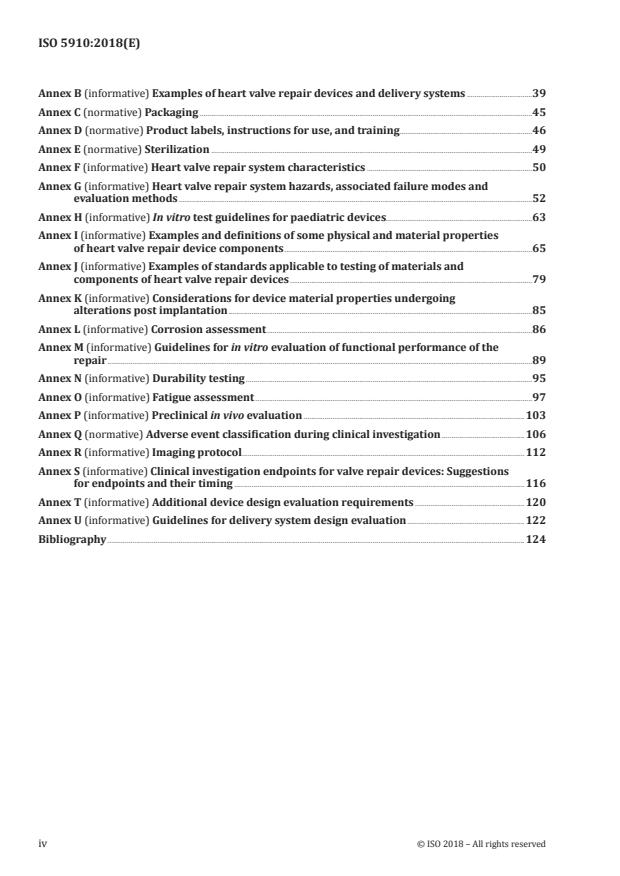
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...