ISO 22679:2021
(Main)Cardiovascular implants — Transcatheter cardiac occluders
Cardiovascular implants — Transcatheter cardiac occluders
This document specifies important in vitro tests including functional and durability characteristics of transcatheter cardiac occluders, and their delivery systems and accessories. This document does not specify exact test methods for functional and durability testing, but it offers requirements and recommendations for performance tests of the cardiac occluder system. Surgical occluders have been omitted from the scope of this document given their significant differences in device geometry, materials, implantation methods, and test methods as compared to transcatheter cardiac occluders. This document is applicable to all intracardiac occluders intended for transcatheter implantation in humans (e.g. atrial septal occluder, ventricular septal occluder, patent foramen ovale occluder, left atrial appendage occluder, and paravalvular leak occluders). This document does not cover non-cardiac occluders, but elements of this document can be applicable to patent ductus arteriosus occluders. The following devices and components are outside the scope of this document: surgical devices, cardiac shunt devices, atrial flow regulators, active components (such as sensors), or degradable or animal tissue components. This document is applicable to both newly developed and modified cardiac occluders, their accessory devices, packaging, and labelling. This document defines operational conditions and performance requirements for cardiac occluders where either adequate scientific or clinical evidence, or both, exists for their justification. NOTE At the time of this document, it is impossible to take all future and emerging technologies into consideration. The cardiac occluder systems based on these new technologies can benefit from evaluation based on the basic requirements of this document. Testing beyond the scope of this document can also be necessary in order to verify and validate these cardiac occluder systems.
Titre manque
General Information
- Status
- Published
- Publication Date
- 28-Nov-2021
- Technical Committee
- ISO/TC 150/SC 2 - Cardiovascular implants and extracorporeal systems
- Drafting Committee
- ISO/TC 150/SC 2/WG 8 - Cardiac occluders
- Current Stage
- 6060 - International Standard published
- Start Date
- 29-Nov-2021
- Due Date
- 09-Oct-2021
- Completion Date
- 29-Nov-2021
Overview
ISO 22679:2021 - Cardiovascular implants - Transcatheter cardiac occluders defines performance requirements, testing considerations, and documentation expectations for intracardiac occluders intended for transcatheter implantation. The standard focuses on in vitro functional and durability characteristics of the occluder system, its delivery systems and accessories. It provides requirements and recommendations for performance tests without prescribing exact test methods. Surgical occluders, degradable or animal tissue components, active components (e.g., sensors), and some other device types are explicitly excluded.
Key topics and technical requirements
- Scope and applicability
- Applies to intracardiac transcatheter occluders (e.g., atrial septal, ventricular septal, patent foramen ovale, left atrial appendage, paravalvular leak occluders) and may inform testing for patent ductus arteriosus occluders.
- Covers both newly developed and modified devices, including accessories, packaging, and labelling.
- Fundamental requirements
- Emphasis on risk management, device description, design inputs and outputs, and manufacturability.
- Design verification and validation
- In vitro assessments: material property evaluation, structural performance, fatigue/durability, corrosion, visibility (imaging), dimensional verification, and simulated use testing.
- Device MRI compatibility and visual inspection requirements.
- Usability engineering and training considerations for implantation procedures.
- Preclinical and clinical evaluation
- Preclinical in vivo testing guidelines and reporting expectations.
- Clinical investigation planning: study design, endpoints, imaging protocols, sample size and ethical considerations.
- Supporting elements
- Packaging, labelling, sterilization guidance, and adverse-event classification during clinical investigations.
- Informative annexes addressing pediatric devices, fatigue assessment, delivery system evaluation, imaging protocols, and physician/staff training.
Practical applications and who uses this standard
- Medical device manufacturers developing or modifying transcatheter cardiac occluders and associated delivery systems.
- Design and QA/RA teams preparing verification/validation plans, clinical investigation protocols, and technical documentation for regulatory submissions.
- Test laboratories executing in vitro and preclinical testing to demonstrate device safety and performance.
- Clinical investigators, hospitals, and training teams implementing implantation procedures, imaging follow-up, and adverse-event reporting.
- Regulatory bodies and notified bodies assessing conformity and clinical evidence for cardiovascular implant devices.
Related standards (if applicable)
- ISO 22679 complements other ISO standards and guidance on sterilization, packaging, biocompatibility, and medical device risk management. For device-specific test methods and regulatory compliance, consult applicable national and international standards and regulatory guidance.
ISO 22679:2021 is a practical framework for evaluating safety, performance, and usability of transcatheter cardiac occluder systems, helping ensure consistent testing, documentation, and clinical evaluation across product life cycles.
ISO 22679:2021 - Cardiovascular implants -- Transcatheter cardiac occluders
ISO 22679:2021 - Cardiovascular implants — Transcatheter cardiac occluders Released:11/29/2021
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
ISO 22679:2021 is a standard published by the International Organization for Standardization (ISO). Its full title is "Cardiovascular implants — Transcatheter cardiac occluders". This standard covers: This document specifies important in vitro tests including functional and durability characteristics of transcatheter cardiac occluders, and their delivery systems and accessories. This document does not specify exact test methods for functional and durability testing, but it offers requirements and recommendations for performance tests of the cardiac occluder system. Surgical occluders have been omitted from the scope of this document given their significant differences in device geometry, materials, implantation methods, and test methods as compared to transcatheter cardiac occluders. This document is applicable to all intracardiac occluders intended for transcatheter implantation in humans (e.g. atrial septal occluder, ventricular septal occluder, patent foramen ovale occluder, left atrial appendage occluder, and paravalvular leak occluders). This document does not cover non-cardiac occluders, but elements of this document can be applicable to patent ductus arteriosus occluders. The following devices and components are outside the scope of this document: surgical devices, cardiac shunt devices, atrial flow regulators, active components (such as sensors), or degradable or animal tissue components. This document is applicable to both newly developed and modified cardiac occluders, their accessory devices, packaging, and labelling. This document defines operational conditions and performance requirements for cardiac occluders where either adequate scientific or clinical evidence, or both, exists for their justification. NOTE At the time of this document, it is impossible to take all future and emerging technologies into consideration. The cardiac occluder systems based on these new technologies can benefit from evaluation based on the basic requirements of this document. Testing beyond the scope of this document can also be necessary in order to verify and validate these cardiac occluder systems.
This document specifies important in vitro tests including functional and durability characteristics of transcatheter cardiac occluders, and their delivery systems and accessories. This document does not specify exact test methods for functional and durability testing, but it offers requirements and recommendations for performance tests of the cardiac occluder system. Surgical occluders have been omitted from the scope of this document given their significant differences in device geometry, materials, implantation methods, and test methods as compared to transcatheter cardiac occluders. This document is applicable to all intracardiac occluders intended for transcatheter implantation in humans (e.g. atrial septal occluder, ventricular septal occluder, patent foramen ovale occluder, left atrial appendage occluder, and paravalvular leak occluders). This document does not cover non-cardiac occluders, but elements of this document can be applicable to patent ductus arteriosus occluders. The following devices and components are outside the scope of this document: surgical devices, cardiac shunt devices, atrial flow regulators, active components (such as sensors), or degradable or animal tissue components. This document is applicable to both newly developed and modified cardiac occluders, their accessory devices, packaging, and labelling. This document defines operational conditions and performance requirements for cardiac occluders where either adequate scientific or clinical evidence, or both, exists for their justification. NOTE At the time of this document, it is impossible to take all future and emerging technologies into consideration. The cardiac occluder systems based on these new technologies can benefit from evaluation based on the basic requirements of this document. Testing beyond the scope of this document can also be necessary in order to verify and validate these cardiac occluder systems.
ISO 22679:2021 is classified under the following ICS (International Classification for Standards) categories: 11.040.40 - Implants for surgery, prosthetics and orthotics. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO 22679:2021 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
INTERNATIONAL ISO
STANDARD 22679
First edition
2021-11
Cardiovascular implants —
Transcatheter cardiac occluders
Reference number
© ISO 2021
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
Contents Page
Foreword .v
Introduction . vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 2
4 Abbreviations . 6
5 Fundamental requirements . 7
5.1 General . 7
5.2 Risk management . 7
6 Device description .8
6.1 General . 8
6.2 Intended use . 8
6.3 Design inputs . 8
6.3.1 Operational principles and specifications . 8
6.3.2 Functional, performance and safety requirements . 8
6.3.3 Implant procedure: Device and usability requirements . 9
6.3.4 Packaging, labelling and sterilization . 10
6.4 Design outputs . 10
6.5 Design transfer (manufacturing verification or validation) . 10
7 Design verification and validation .10
7.1 General requirements . 10
7.2 In vitro assessment. 11
7.2.1 General . 11
7.2.2 Test conditions, sample selection and reporting requirements . 11
7.2.3 Material property assessment .12
7.2.4 Structural performance assessment . 13
7.2.5 Component corrosion assessment . 14
7.2.6 Visibility . 14
7.2.7 Visual inspection . 15
7.2.8 Dimensional verification . 15
7.2.9 Device MRI compatibility . 15
7.2.10 Simulated use assessment . 15
7.2.11 Usability engineering process . 15
7.2.12 Design- or procedure-specific testing . 15
7.3 Preclinical in vivo evaluation .15
7.3.1 General .15
7.3.2 Overall requirements .15
7.3.3 Methods . 17
7.3.4 Test report . 18
7.4 Clinical investigations . 19
7.4.1 General . 19
7.4.2 Study considerations .20
7.4.3 Imaging assessment . 21
7.4.4 Study design . 21
7.4.5 Explant analysis . 21
7.4.6 Pilot study considerations . 22
7.4.7 Study endpoints. 22
7.4.8 Ethical considerations . 22
7.4.9 Pivotal studies: Distribution of subjects and investigators .23
7.4.10 Site qualification and training requirements . 23
7.4.11 Study population . 23
7.4.12 Statistical considerations . 24
iii
7.4.13 Sample size . 25
7.4.14 Duration of study . 25
7.4.15 Patient selection criteria . 25
7.4.16 Clinical data requirements . 26
Annex A (informative) Rationale for the provisions of this document .31
Annex B (informative) Transcatheter cardiac occluder hazard analysis example .34
Annex C (normative) Packaging .36
Annex D (normative) Product labels and instructions for use .37
Annex E (normative) Sterilization .38
Annex F (informative) Corrosion assessment .39
Annex G (informative) In vitro test guidelines for paediatric devices .42
Annex H (informative) Fatigue and durability assessment . 44
Annex I (normative) Adverse event classification during clinical investigation .50
Annex J (informative) Imaging protocol .55
Annex K (informative) Clinical investigation endpoints for transcatheter cardiac occluders:
Suggestions for endpoints and their timing .56
Annex L (informative) Examples of design specific testing .59
Annex M (informative) Guidelines for delivery system design evaluation .61
Annex N (normative) Preclinical in vivo evaluation .63
Annex O (informative) In vitro test pressure guidelines .66
Annex P (informative) Training for physicians and support staff .68
Bibliography .69
iv
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www.iso.org/directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received (see www.iso.org/patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to
the World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT), see
www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 150, Implants for surgery, Subcommittee
SC 2, Cardiovascular implants and extracorporeal systems.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
v
Introduction
The field of transcatheter cardiac occluders has advanced and expanded significantly in recent
years. Therefore, a group of engineers, scientists, and clinicians, experts well aware of the problems
associated with transcatheter cardiac occluder devices and their development, has prepared this
document. This document deals with those areas that will help ensure adequate mitigation of device-
associated risks for patients and other users of the device, facilitate quality assurance, and help ensure
that the device will be provided in a convenient and usable form. This document emphasizes the need
to specify and report types of in vitro testing, preclinical in vivo, and clinical evaluations. It describes
the requirements for labels and packaging of the device. The in vitro, preclinical in vivo, and clinical
evaluations described in this document are intended to help establish safety and performance of a
transcatheter cardiac occluder.
This document outlines an approach for minimizing adverse events from the implantation of a
transcatheter cardiac occluder through risk management. The selection of appropriate verification
or validation tests and methods are derived from the risk assessment and design input requirements.
The tests include those to assess the physical, mechanical, chemical, and biological properties of
transcatheter cardiac occluders and of their materials and components. The tests also include those for
preclinical in vivo evaluation and clinical evaluation of the transcatheter cardiac occluders.
vi
INTERNATIONAL STANDARD ISO 22679:2021(E)
Cardiovascular implants — Transcatheter cardiac
occluders
1 Scope
This document specifies important in vitro tests including functional and durability characteristics
of transcatheter cardiac occluders, and their delivery systems and accessories. This document does
not specify exact test methods for functional and durability testing, but it offers requirements and
recommendations for performance tests of the cardiac occluder system.
Surgical occluders have been omitted from the scope of this document given their significant differences
in device geometry, materials, implantation methods, and test methods as compared to transcatheter
cardiac occluders.
This document is applicable to all intracardiac occluders intended for transcatheter implantation in
humans (e.g. atrial septal occluder, ventricular septal occluder, patent foramen ovale occluder, left
atrial appendage occluder, and paravalvular leak occluders). This document does not cover non-cardiac
occluders, but elements of this document can be applicable to patent ductus arteriosus occluders.
The following devices and components are outside the scope of this document: surgical devices, cardiac
shunt devices, atrial flow regulators, active components (such as sensors), or degradable or animal
tissue components.
This document is applicable to both newly developed and modified cardiac occluders, their accessory
devices, packaging, and labelling.
This document defines operational conditions and performance requirements for cardiac occluders
where either adequate scientific or clinical evidence, or both, exists for their justification.
NOTE At the time of this document, it is impossible to take all future and emerging technologies into
consideration. The cardiac occluder systems based on these new technologies can benefit from evaluation based
on the basic requirements of this document. Testing beyond the scope of this document can also be necessary in
order to verify and validate these cardiac occluder systems.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 10555-1, Intravascular catheters — Sterile and single-use catheters — Part 1: General requirements
ISO 10993-1, Biological evaluation of medical devices — Part 1: Evaluation and testing within a risk
management process
ISO 10993-2, Biological evaluation of medical devices — Part 2: Animal welfare requirements
ISO 11070, Sterile single-use intravascular introducers, dilators and guidewires
ISO 11135-1, Sterilization of health care products — Ethylene oxide — Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO 11137-1, Sterilization of health care products — Radiation — Part 1: Requirements for development,
validation and routine control of a sterilization process for medical devices
ISO 11137-2, Sterilization of health care products — Radiation — Part 2: Establishing the sterilization dose
ISO 11137-3, Sterilization of health care products — Radiation — Part 3: Guidance on dosimetric aspects of
development, validation and routine control
ISO 11607-1, Packaging for terminally sterilized medical devices — Part 1: Requirements for materials,
sterile barrier systems and packaging systems
ISO 11607-2, Packaging for terminally sterilized medical devices — Part 2: Validation requirements for
forming, sealing and assembly processes
ISO 13485, Medical devices — Quality management systems — Requirements for regulatory purposes
ISO 14155, Clinical investigation of medical devices for human subjects — Good clinical practice
ISO 14630, Non-active surgical implants — General requirements
ISO 14937, Sterilization of health care products — General requirements for characterization of a sterilizing
agent and the development, validation and routine control of a sterilization process for medical devices
ISO 14971, Medical devices — Application of risk management to medical devices
ISO 15223-1, Medical devices — Symbols to be used with information to be supplied by the manufacturer
— Part 1: General requirements
ISO 15223-2, Medical devices — Symbols to be used with medical device labels, labelling, and information
to be supplied — Part 2: Symbol development, selection and validation
ISO 17664-1, Processing of health care products — Information to be provided by the medical device
manufacturer for the processing of medical devices — Part 1: Critical and semi-critical medical devices
ISO 17665-1, Sterilization of health care products — Moist heat — Part 1: Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO/TS 17665-2, Sterilization of health care products — Moist heat — Part 2: Guidance on the application
of ISO 17665-1
ISO/TS 17665-3, Sterilization of health care products — Moist heat — Part 3: Guidance on the designation
of a medical device to a product family and processing category for steam sterilization
ISO 20417, Medical devices — Information to be supplied by the manufacturer
ISO 22442-1, Medical devices utilizing animal tissues and their derivatives — Part 1: Application of risk
management
IEC 62366-1, Medical devices — Part 1: Application of usability engineering to medical devices
ASTM F2052, Standard test method for measurement of magnetically induced displacement force on
medical devices in the magnetic resonance environment
ASTM F2119, Standard test method for evaluation of MR image artifacts from passive implants
ASTM F2182, Standard test method for measurement of radio frequency induced heating near passive
implants during magnetic resonance imaging
ASTM F2213, Standard test method for measurement of magnetically induced torque on medical devices in
the magnetic resonance environment
ASTM F2503, Standard practice for marking medical devices and other items for safety in the magnetic
resonance environment
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
3.1
access system
system consisting of a variety of components (e.g. sheath, haemostasis control valve, side ports for
administration of physiological fluids and medications) to provide vascular access for the cardiac
occluder (3.3) delivery system (3.8)
3.2
adverse event
AE
untoward medical occurrence, unintended disease or injury, or untoward clinical signs (including
abnormal laboratory findings), in subjects, users or other persons, whether or not related to the
investigational medical device
Note 1 to entry: This definition includes events related to the investigational medical device or the comparator.
Note 2 to entry: This definition includes events related to the procedures involved.
Note 3 to entry: For users or other persons, this definition is restricted to events related to investigational
medical devices.
3.3
cardiac occluder
non-active (3.20) implant to occlude a specific cardiac anatomic structure (e.g. atrial septal defects,
ventricular septal defects, patent foramen ovale, left atrial appendage) or seal an abnormal site of blood
flow (e.g. heart valve substitute paravalvular leak)
3.3.1
atrial septal occluder
cardiac occluder (3.3) used to treat an atrial septal defect
3.3.2
left atrial appendage occluder
cardiac occluder (3.3) used to close the opening of the left atrial appendage
3.3.3
paravalvular leak occluder
cardiac occluder (3.3) used to close a paravalvular leak
3.3.4
patent ductus arteriosus occluder
occluder used to close a patent ductus arteriosus
3.3.5
patent foramen ovale occluder
cardiac occluder (3.3) used to close a patent foramen ovale
3.3.6
ventricular septal occluder
cardiac occluder (3.3) used to treat a ventricular septal defect
3.4
cardiac occluder system
supplied components, such as the cardiac occluder (3.3), access system (3.1), delivery system (3.8),
accessories, packaging and labelling
3.5
delivery approach
anatomical access used to deliver the cardiac occluder (3.3) to the intended implant site (3.17) (e.g.
transfemoral, transseptal)
3.6
delivery catheter
component of the delivery system (3.8), used to advance and deploy a cardiac occluder (3.3) to the
intended implantation site
3.7
delivery sheath
hollow tube that traverses the skin and subcutaneous tissue and enters the endovascular space to
facilitate entry of wires and catheters
3.8
delivery system
system [e.g. delivery catheter (3.6)] used to deliver, deploy, attach or adjust [i.e. recapture (3.22) or
retrieve] a cardiac occluder (3.3) in the intended implantation site
3.9
design validation
establishment by objective evidence that device specifications conform with user needs and intended
use(s) (3.18)
3.10
design verification
establishment by objective evidence that the design output meets the design input requirements
3.11
device embolization
post-deployment or peri-procedural dislodgement of the cardiac occluder (3.3), from the implantation
site or catheter, respectively, to an unintended and non-therapeutic location via the bloodstream
3.12
device failure
inability of a cardiac occluder (3.3) to perform its intended function sufficient to cause a hazard
3.13
device migration
detectable movement or displacement of the cardiac occluder (3.3) from its original position within
close proximity of the intended implant site (3.17), without embolization
3.14
failure mode
mechanism of device failure (3.12) [e.g. catastrophic support structure fracture (3.15)]
3.15
fracture
unintentional disruption, under the action of applied load (e.g. force, torque, or deformation), of a
structural element (3.32) of the cardiac occluder system (3.4) that were previously intact
3.16
imaging modality
imaging method used to facilitate diagnosis, delivery and/or retrieval (3.24)/recapture (3.22) of the
implant within the target implant site (3.17), as well as to assess cardiac occluder (3.3) performance
after implantation
3.17
implant site
intended anatomic site of a cardiac occluder (3.3) deployment
3.18
intended use
use of a cardiac occluder (3.3) in accordance with the specifications, instructions and information
provided by the manufacturer
3.19
membrane
flexible synthetic material covering or integrated within a portion or all of the cardiac occlude
3.20
non-active
implant which does not depend on a source of electrical energy or any source of power other than that
directly generated by the human body or gravity
3.21
protective packaging
configuration of materials designed to prevent damage to the sterile barrier system (3.31) and its
contents from the time of their assembly until the point of use
[SOURCE: ISO 11607-1:2019, 3.14]
3.22
recapture
process of returning the cardiac occluder (3.3) back into the delivery system (3.8), following partial or
full deployment, but prior to its release
3.23
repositioning
change in implant position and/or orientation of a partially or fully deployed cardiac occluder (3.3) via a
transcatheter technique, possibly requiring full or partial recapturing of the device
3.24
retrieval
removal of a partially or fully deployed cardiac occluder (3.3) via a transcatheter or surgical technique
3.25
risk
combination of the probability of occurrence of harm and the severity (3.30) of that harm
[SOURCE: ISO 14971:2019, 3.18]
3.26
risk analysis
systematic use of available information to identify hazards and to estimate the associated risk(s) (3.25)
[SOURCE: ISO 14971:2019, 3.19, modified — "associated" has been added and "(s)" has been added to
"risk".]
3.27
risk assessment
overall process comprising a risk analysis (3.26) and a risk (3.25) evaluation
[SOURCE: ISO 14971:2019, 3.20]
3.28
sample size
quantity of individual specimens of a device tested
[SOURCE: ASTM F3172 -15: 2015, 3.1.13]
3.29
safety
freedom from unacceptable risk (3.25)
[SOURCE: ISO 14971:2019, 3.26]
3.30
severity
measure of the possible consequences of a hazard
[SOURCE: ISO 14971:2019, 3.27]
3.31
sterile barrier system
minimum package that minimizes the risk (3.25) of ingress of microorganisms and allows aseptic
presentation of the sterile contents at the point of use
[SOURCE: ISO 11607-1:2019, 3.23]
3.32
structural element
stent or frame component of a cardiac occluder (3.3)
3.33
withdrawal
removal of the occluder delivery system (3.8) with or without the cardiac occluder (3.3)
4 Abbreviations
For the purposes of this document, the following abbreviations apply.
ADE adverse device effect
AE adverse event
AFib atrial fibrillation
ASD atrial septic defect
CEC Clinical Events Committee
CIP clinical investigation plan
CMR cardiac magnetic resonance
CRF case report form
CT computed tomography
DIC disseminated intravascular coagulation
DSMB Data Safety Monitoring Board
EC Ethics Committee
GCP Good Clinical Practice
HIT heparin-induced thrombocytopenia
ICE intracardiac echocardiography
IFU instructions for use
IRB Institutional Review Board
LAA left atrial appendage
MRI magnetic resonance imaging
NYHA New York Heart Association
PCI percutaneous coronary intervention
PMCF post-market clinical follow-up
PDA patent ductus arteriosus
PET position emission tomography
PFO patent foramen ovale
PVL paravalvular leak
SADE serious adverse device effect
SAE serious adverse event
TEE transesophageal echocardiography
TTE transthoracic echocardiography
VSD ventricular septal defect
5 Fundamental requirements
5.1 General
The activities described within this document shall be carried out within a formal quality system.
NOTE ISO 13485 contains requirements for a suitable quality system for a medical manufacturer. Additional
requirements can be specified by a country or region.
5.2 Risk management
The manufacturer shall define, implement and document risk management activities in accordance
with ISO 14971. A risk-based methodology challenges the manufacturer to continually analyse and
evaluate known and theoretical risks of the device, to develop the most appropriate methods for
mitigating the risks of the device, and to implement the appropriate test, analysis methods, or rationale
to demonstrate the residual risks are acceptable (see Annex A).
Annex B provides an example of a hazard analysis to serve as a starting point for a risk analysis specific
to some cardiac occluder devices.
Annex I provides definitions and examples of adverse events that can be useful in the risk management
process.
As part of the risk management process, the manufacturer shall establish, document, implement and
maintain a usability engineering process, linked but distinct from the device design process, as detailed
in IEC 62366-1.
6 Device description
6.1 General
The requirements of ISO 14630 shall apply.
6.2 Intended use
The manufacturer shall identify the pathological condition(s) to be treated, the intended patient
population and intended claims. The manufacturer shall also consider the intended user(s) of the
medical device and the environments in which it is used.
6.3 Design inputs
6.3.1 Operational principles and specifications
The manufacturer shall define the operational specifications for the device including the principles of
operation, intended device delivery approach or process, durability, shelf life, shipping or storage limits,
and the physiological environment in which it is intended to function. The manufacturer shall define
relevant anatomical characteristics and device dimensional parameters that will be required to select
either the device model or size, or both. Additionally, if designed for periprocedural modification, define
how the device configuration will be determined (see Annex O and Annex G).
6.3.2 Functional, performance and safety requirements
6.3.2.1 General
The manufacturer shall establish (i.e. define, document and implement) the functional, performance
and safety requirements of the cardiac occluder system for the intended use and device claims.
6.3.2.2 Implantable device
The intended performance of the cardiac occluder device shall take into consideration at least the
following:
a) the ability to occlude undesired blood flow;
b) the ability to resist migration and embolization;
c) the ability to minimize haemolysis;
d) the ability to minimize undesired thrombus formation;
e) biocompatibility;
f) the ability to resist corrosion;
g) the ability to minimize particulate shedding;
h) compatibility with adjacent anatomical structures or other implanted devices, if applicable;
i) compatibility with diagnostic imaging techniques (e.g. MRI);
j) visibility under diagnostic imaging techniques (e.g. MRI, echocardiography, fluoroscopy, CT);
k) deliverability and implantability in the target population;
l) the ability to maintain structural and functional integrity during the expected lifetime of the
device;
m) the ability to maintain structural integrity, functionality and sterility for the labelled shelf life prior
to implantation;
n) the ability to be consistently and safely prepared for implantation;
o) the ability to be consistently and safely implanted in the intended implantation site and achieve the
aforementioned performance objectives;
p) the ability to be either safely retrieved, adjusted or repositioned, or all, if applicable.
NOTE See ISO 14630.
6.3.2.3 Access and delivery system
The functional, performance and safety requirements of the access and delivery system shall be
established (see Annex M). All supplied sterile single-use intravascular catheters shall follow
ISO 10555-1. If sterile single-use intravascular introducers, dilators or guidewires are supplied by the
manufacturer, then they shall follow ISO 11070, as applicable. For cardiac occluder systems which either
require or allow the user to select a non-supplied access system, the attributes of the non-supplied
access system shall be established for it to be compatible with the cardiac occluder delivery system.
These attributes include minimum inner diameter and length.
The design attributes shall take into consideration at least the following to meet the intended
performance of the delivery and access system:
a) compatibility of the access system, delivery system, and the cardiac occluder;
b) the ability to permit consistent, accurate and safe loading, access, delivery, deployment and release
of the cardiac occluder to the intended implantation site;
c) the ability to permit consistent and safe withdrawal of the delivery system prior to and after
deployment of the cardiac occluder device;
d) the ability to minimize thrombus formation;
e) the ability to minimize blood loss;
f) the ability to either retrieve, reposition, or remove the cardiac occluder device, or all, if applicable;
g) biocompatibility;
h) the ability to resist corrosion;
i) the ability to maintain integrity of the coating, if applicable;
j) the ability to minimize particulate generation;
k) the ability to maintain its functionality and sterility for the labelled shelf life;
l) compatibility and visibility with diagnostic imaging techniques (e.g. MRI, echo, fluoroscopy, CT), if
applicable;
m) compatibility with tools and accessories required to complete the procedure.
n) the ability to avoid air thrombus during the procedure;
o) the ability to inject contrast agent through the applicable changes of the procedure, if applicable.
6.3.3 Implant procedure: Device and usability requirements
The cardiac occluder system shall provide intended users the ability to safely and effectively perform
pre-operative, intra-operative, and post-operative procedural tasks to achieve desired outcome. This
shall include procedure-specific tools and accessories that intended users will need to complete the
procedure. In addition to establishing the device physical requirements during the implant procedure,
the usability engineering process according to IEC 62366-1 shall be used to establish user interface
characteristics that can be related to safety and effectiveness during the implant procedure.
6.3.4 Packaging, labelling and sterilization
The cardiac occluder system shall meet the requirements for packaging, labelling, and sterilization
contained within Annex C, Annex D, and Annex E, respectively.
The manufacturer shall provide information and guidance (e.g. imaging modalities and sizing procedure)
in the labelling to allow for appropriate preparation of the implantation site (e.g. left atrial appendage),
selection of appropriate implant size, implantation of the cardiac occluder, and post-procedure care and
medication, if applicable. The manufacturer shall also provide MRI safety information in the labelling.
See ISO 11135, ISO 11137-1, ISO 11137-2, ISO 11137-3, ISO 14160, ISO 14937, ISO 17665-1, ISO/TS 17665-2,
and ISO/TS 17665-3 for additional information regarding sterilization.
See ISO 11607-1 and ISO 11607-2 for additional information regarding packaging.
See ISO 15223-1, ISO 15223-2, and ASTM F2503 for additional information regarding labelling,
6.4 Design outputs
Design and development outputs shall meet the requirements of ISO 13485.
The manufacturer shall establish (i.e. define, document and implement) a specification of the
cardiac occluder system. In addition to the physical components of the cardiac occluder system, the
manufacturer shall establish instructions and specifications for the implant procedure. Instructions
shall meet the requirements of Annex D.
6.5 Design transfer (manufacturing verification or validation)
Design transfer requirements shall meet the requirements of ISO 13485.
The manufacturer shall establish (i.e. define, document and implement) the manufacturing process
operations and inspection steps including components and manufacturing materials.
As part of the risk management process, the manufacturer shall establish the control measures and
process conditions necessary to ensure that the process is capable of consistently delivering quality
product. The risk management file shall identify and justify the verification or validation activities
necessary to demonstrate the acceptability of the process settings chosen.
The manufacturer shall establish the adequacy of full-scale manufacturing by validation of the
manufacturing process (the installation qualification (IQ), operational qualification (OQ) and
performance qualification (PQ)).
7 Design verification and validation
7.1 General requirements
The manufacturer shall perform design verification to demonstrate that the design output of a cardiac
occluder system meets the design input. The manufacturer shall establish a design verification strategy
relating to hazards identified from the risk analysis. The protocols shall identify the test purpose, setup,
equipment (e.g. specifications, calibration), test conditions (with a justification of appropriateness to
anticipated in vivo operating conditions for the device, if applicable), acceptance criteria, and sample
quantities to be tested. Design verification includes testing, analyses, and other activities.
The manufacturer shall also validate the design of the cardiac occluder system to ensure that the device
meets user needs and intended use; refer to applicable sections of ISO 13485. The design verification
and validation shall address all risks identified in the risk assessment at the appropriate level.
[50]
NOTE See ISO/IEC 17025 regarding considerations for test method validation.
7.2 In vitro assessment
7.2.1 General
In vitro assessment shall be used, where appropriate, to demonstrate mitigation of risks identified in
the risk analysis through either design verification or validation, or both.
7.2.2 Test conditions, sample selection and reporting requirements
7.2.2.1 Test conditions
The test conditions for each in vitro assessment shall be defined and justified (see Annex G and Annex O
for examples of differential pressures).
7.2.2.2 Test sample selection
Test samples for either design verification or validation, or both, shall represent the cardiac occluder
system product intended for clinical use. Representative products include initial production units,
batches or their equivalents. Test samples shall be appropriately preconditioned prior to testing,
including exposure to the maximum number of allowed sterilization cycles, process chemicals, aging
effects, shipping/handling, in accordance with all manufacturing procedures and instructions for use,
where appropriate. Any deviations of the test samples from the finished product shall be justified.
The full range of available device configurations (e.g. sizes, deployment shapes, use ranges, delivery
system and accessories, and implant sites) shall be considered during selection of test samples; however,
depending on the particular test, testing does not necessarily have to be completed for each device
configuration.
For all tests, the number of samples shall be justified based on the specific intent of the test, with a
scientific justification. Additional information regarding sampling and sample conditioning, includi
...
INTERNATIONAL ISO
STANDARD 22679
First edition
2021-11
Cardiovascular implants —
Transcatheter cardiac occluders
Reference number
© ISO 2021
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
Contents Page
Foreword .v
Introduction . vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 2
4 Abbreviations . 6
5 Fundamental requirements . 7
5.1 General . 7
5.2 Risk management . 7
6 Device description .8
6.1 General . 8
6.2 Intended use . 8
6.3 Design inputs . 8
6.3.1 Operational principles and specifications . 8
6.3.2 Functional, performance and safety requirements . 8
6.3.3 Implant procedure: Device and usability requirements . 9
6.3.4 Packaging, labelling and sterilization . 10
6.4 Design outputs . 10
6.5 Design transfer (manufacturing verification or validation) . 10
7 Design verification and validation .10
7.1 General requirements . 10
7.2 In vitro assessment. 11
7.2.1 General . 11
7.2.2 Test conditions, sample selection and reporting requirements . 11
7.2.3 Material property assessment .12
7.2.4 Structural performance assessment . 13
7.2.5 Component corrosion assessment . 14
7.2.6 Visibility . 14
7.2.7 Visual inspection . 15
7.2.8 Dimensional verification . 15
7.2.9 Device MRI compatibility . 15
7.2.10 Simulated use assessment . 15
7.2.11 Usability engineering process . 15
7.2.12 Design- or procedure-specific testing . 15
7.3 Preclinical in vivo evaluation .15
7.3.1 General .15
7.3.2 Overall requirements .15
7.3.3 Methods . 17
7.3.4 Test report . 18
7.4 Clinical investigations . 19
7.4.1 General . 19
7.4.2 Study considerations .20
7.4.3 Imaging assessment . 21
7.4.4 Study design . 21
7.4.5 Explant analysis . 21
7.4.6 Pilot study considerations . 22
7.4.7 Study endpoints. 22
7.4.8 Ethical considerations . 22
7.4.9 Pivotal studies: Distribution of subjects and investigators .23
7.4.10 Site qualification and training requirements . 23
7.4.11 Study population . 23
7.4.12 Statistical considerations . 24
iii
7.4.13 Sample size . 25
7.4.14 Duration of study . 25
7.4.15 Patient selection criteria . 25
7.4.16 Clinical data requirements . 26
Annex A (informative) Rationale for the provisions of this document .31
Annex B (informative) Transcatheter cardiac occluder hazard analysis example .34
Annex C (normative) Packaging .36
Annex D (normative) Product labels and instructions for use .37
Annex E (normative) Sterilization .38
Annex F (informative) Corrosion assessment .39
Annex G (informative) In vitro test guidelines for paediatric devices .42
Annex H (informative) Fatigue and durability assessment . 44
Annex I (normative) Adverse event classification during clinical investigation .50
Annex J (informative) Imaging protocol .55
Annex K (informative) Clinical investigation endpoints for transcatheter cardiac occluders:
Suggestions for endpoints and their timing .56
Annex L (informative) Examples of design specific testing .59
Annex M (informative) Guidelines for delivery system design evaluation .61
Annex N (normative) Preclinical in vivo evaluation .63
Annex O (informative) In vitro test pressure guidelines .66
Annex P (informative) Training for physicians and support staff .68
Bibliography .69
iv
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www.iso.org/directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received (see www.iso.org/patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to
the World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT), see
www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 150, Implants for surgery, Subcommittee
SC 2, Cardiovascular implants and extracorporeal systems.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
v
Introduction
The field of transcatheter cardiac occluders has advanced and expanded significantly in recent
years. Therefore, a group of engineers, scientists, and clinicians, experts well aware of the problems
associated with transcatheter cardiac occluder devices and their development, has prepared this
document. This document deals with those areas that will help ensure adequate mitigation of device-
associated risks for patients and other users of the device, facilitate quality assurance, and help ensure
that the device will be provided in a convenient and usable form. This document emphasizes the need
to specify and report types of in vitro testing, preclinical in vivo, and clinical evaluations. It describes
the requirements for labels and packaging of the device. The in vitro, preclinical in vivo, and clinical
evaluations described in this document are intended to help establish safety and performance of a
transcatheter cardiac occluder.
This document outlines an approach for minimizing adverse events from the implantation of a
transcatheter cardiac occluder through risk management. The selection of appropriate verification
or validation tests and methods are derived from the risk assessment and design input requirements.
The tests include those to assess the physical, mechanical, chemical, and biological properties of
transcatheter cardiac occluders and of their materials and components. The tests also include those for
preclinical in vivo evaluation and clinical evaluation of the transcatheter cardiac occluders.
vi
INTERNATIONAL STANDARD ISO 22679:2021(E)
Cardiovascular implants — Transcatheter cardiac
occluders
1 Scope
This document specifies important in vitro tests including functional and durability characteristics
of transcatheter cardiac occluders, and their delivery systems and accessories. This document does
not specify exact test methods for functional and durability testing, but it offers requirements and
recommendations for performance tests of the cardiac occluder system.
Surgical occluders have been omitted from the scope of this document given their significant differences
in device geometry, materials, implantation methods, and test methods as compared to transcatheter
cardiac occluders.
This document is applicable to all intracardiac occluders intended for transcatheter implantation in
humans (e.g. atrial septal occluder, ventricular septal occluder, patent foramen ovale occluder, left
atrial appendage occluder, and paravalvular leak occluders). This document does not cover non-cardiac
occluders, but elements of this document can be applicable to patent ductus arteriosus occluders.
The following devices and components are outside the scope of this document: surgical devices, cardiac
shunt devices, atrial flow regulators, active components (such as sensors), or degradable or animal
tissue components.
This document is applicable to both newly developed and modified cardiac occluders, their accessory
devices, packaging, and labelling.
This document defines operational conditions and performance requirements for cardiac occluders
where either adequate scientific or clinical evidence, or both, exists for their justification.
NOTE At the time of this document, it is impossible to take all future and emerging technologies into
consideration. The cardiac occluder systems based on these new technologies can benefit from evaluation based
on the basic requirements of this document. Testing beyond the scope of this document can also be necessary in
order to verify and validate these cardiac occluder systems.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 10555-1, Intravascular catheters — Sterile and single-use catheters — Part 1: General requirements
ISO 10993-1, Biological evaluation of medical devices — Part 1: Evaluation and testing within a risk
management process
ISO 10993-2, Biological evaluation of medical devices — Part 2: Animal welfare requirements
ISO 11070, Sterile single-use intravascular introducers, dilators and guidewires
ISO 11135-1, Sterilization of health care products — Ethylene oxide — Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO 11137-1, Sterilization of health care products — Radiation — Part 1: Requirements for development,
validation and routine control of a sterilization process for medical devices
ISO 11137-2, Sterilization of health care products — Radiation — Part 2: Establishing the sterilization dose
ISO 11137-3, Sterilization of health care products — Radiation — Part 3: Guidance on dosimetric aspects of
development, validation and routine control
ISO 11607-1, Packaging for terminally sterilized medical devices — Part 1: Requirements for materials,
sterile barrier systems and packaging systems
ISO 11607-2, Packaging for terminally sterilized medical devices — Part 2: Validation requirements for
forming, sealing and assembly processes
ISO 13485, Medical devices — Quality management systems — Requirements for regulatory purposes
ISO 14155, Clinical investigation of medical devices for human subjects — Good clinical practice
ISO 14630, Non-active surgical implants — General requirements
ISO 14937, Sterilization of health care products — General requirements for characterization of a sterilizing
agent and the development, validation and routine control of a sterilization process for medical devices
ISO 14971, Medical devices — Application of risk management to medical devices
ISO 15223-1, Medical devices — Symbols to be used with information to be supplied by the manufacturer
— Part 1: General requirements
ISO 15223-2, Medical devices — Symbols to be used with medical device labels, labelling, and information
to be supplied — Part 2: Symbol development, selection and validation
ISO 17664-1, Processing of health care products — Information to be provided by the medical device
manufacturer for the processing of medical devices — Part 1: Critical and semi-critical medical devices
ISO 17665-1, Sterilization of health care products — Moist heat — Part 1: Requirements for the development,
validation and routine control of a sterilization process for medical devices
ISO/TS 17665-2, Sterilization of health care products — Moist heat — Part 2: Guidance on the application
of ISO 17665-1
ISO/TS 17665-3, Sterilization of health care products — Moist heat — Part 3: Guidance on the designation
of a medical device to a product family and processing category for steam sterilization
ISO 20417, Medical devices — Information to be supplied by the manufacturer
ISO 22442-1, Medical devices utilizing animal tissues and their derivatives — Part 1: Application of risk
management
IEC 62366-1, Medical devices — Part 1: Application of usability engineering to medical devices
ASTM F2052, Standard test method for measurement of magnetically induced displacement force on
medical devices in the magnetic resonance environment
ASTM F2119, Standard test method for evaluation of MR image artifacts from passive implants
ASTM F2182, Standard test method for measurement of radio frequency induced heating near passive
implants during magnetic resonance imaging
ASTM F2213, Standard test method for measurement of magnetically induced torque on medical devices in
the magnetic resonance environment
ASTM F2503, Standard practice for marking medical devices and other items for safety in the magnetic
resonance environment
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
3.1
access system
system consisting of a variety of components (e.g. sheath, haemostasis control valve, side ports for
administration of physiological fluids and medications) to provide vascular access for the cardiac
occluder (3.3) delivery system (3.8)
3.2
adverse event
AE
untoward medical occurrence, unintended disease or injury, or untoward clinical signs (including
abnormal laboratory findings), in subjects, users or other persons, whether or not related to the
investigational medical device
Note 1 to entry: This definition includes events related to the investigational medical device or the comparator.
Note 2 to entry: This definition includes events related to the procedures involved.
Note 3 to entry: For users or other persons, this definition is restricted to events related to investigational
medical devices.
3.3
cardiac occluder
non-active (3.20) implant to occlude a specific cardiac anatomic structure (e.g. atrial septal defects,
ventricular septal defects, patent foramen ovale, left atrial appendage) or seal an abnormal site of blood
flow (e.g. heart valve substitute paravalvular leak)
3.3.1
atrial septal occluder
cardiac occluder (3.3) used to treat an atrial septal defect
3.3.2
left atrial appendage occluder
cardiac occluder (3.3) used to close the opening of the left atrial appendage
3.3.3
paravalvular leak occluder
cardiac occluder (3.3) used to close a paravalvular leak
3.3.4
patent ductus arteriosus occluder
occluder used to close a patent ductus arteriosus
3.3.5
patent foramen ovale occluder
cardiac occluder (3.3) used to close a patent foramen ovale
3.3.6
ventricular septal occluder
cardiac occluder (3.3) used to treat a ventricular septal defect
3.4
cardiac occluder system
supplied components, such as the cardiac occluder (3.3), access system (3.1), delivery system (3.8),
accessories, packaging and labelling
3.5
delivery approach
anatomical access used to deliver the cardiac occluder (3.3) to the intended implant site (3.17) (e.g.
transfemoral, transseptal)
3.6
delivery catheter
component of the delivery system (3.8), used to advance and deploy a cardiac occluder (3.3) to the
intended implantation site
3.7
delivery sheath
hollow tube that traverses the skin and subcutaneous tissue and enters the endovascular space to
facilitate entry of wires and catheters
3.8
delivery system
system [e.g. delivery catheter (3.6)] used to deliver, deploy, attach or adjust [i.e. recapture (3.22) or
retrieve] a cardiac occluder (3.3) in the intended implantation site
3.9
design validation
establishment by objective evidence that device specifications conform with user needs and intended
use(s) (3.18)
3.10
design verification
establishment by objective evidence that the design output meets the design input requirements
3.11
device embolization
post-deployment or peri-procedural dislodgement of the cardiac occluder (3.3), from the implantation
site or catheter, respectively, to an unintended and non-therapeutic location via the bloodstream
3.12
device failure
inability of a cardiac occluder (3.3) to perform its intended function sufficient to cause a hazard
3.13
device migration
detectable movement or displacement of the cardiac occluder (3.3) from its original position within
close proximity of the intended implant site (3.17), without embolization
3.14
failure mode
mechanism of device failure (3.12) [e.g. catastrophic support structure fracture (3.15)]
3.15
fracture
unintentional disruption, under the action of applied load (e.g. force, torque, or deformation), of a
structural element (3.32) of the cardiac occluder system (3.4) that were previously intact
3.16
imaging modality
imaging method used to facilitate diagnosis, delivery and/or retrieval (3.24)/recapture (3.22) of the
implant within the target implant site (3.17), as well as to assess cardiac occluder (3.3) performance
after implantation
3.17
implant site
intended anatomic site of a cardiac occluder (3.3) deployment
3.18
intended use
use of a cardiac occluder (3.3) in accordance with the specifications, instructions and information
provided by the manufacturer
3.19
membrane
flexible synthetic material covering or integrated within a portion or all of the cardiac occlude
3.20
non-active
implant which does not depend on a source of electrical energy or any source of power other than that
directly generated by the human body or gravity
3.21
protective packaging
configuration of materials designed to prevent damage to the sterile barrier system (3.31) and its
contents from the time of their assembly until the point of use
[SOURCE: ISO 11607-1:2019, 3.14]
3.22
recapture
process of returning the cardiac occluder (3.3) back into the delivery system (3.8), following partial or
full deployment, but prior to its release
3.23
repositioning
change in implant position and/or orientation of a partially or fully deployed cardiac occluder (3.3) via a
transcatheter technique, possibly requiring full or partial recapturing of the device
3.24
retrieval
removal of a partially or fully deployed cardiac occluder (3.3) via a transcatheter or surgical technique
3.25
risk
combination of the probability of occurrence of harm and the severity (3.30) of that harm
[SOURCE: ISO 14971:2019, 3.18]
3.26
risk analysis
systematic use of available information to identify hazards and to estimate the associated risk(s) (3.25)
[SOURCE: ISO 14971:2019, 3.19, modified — "associated" has been added and "(s)" has been added to
"risk".]
3.27
risk assessment
overall process comprising a risk analysis (3.26) and a risk (3.25) evaluation
[SOURCE: ISO 14971:2019, 3.20]
3.28
sample size
quantity of individual specimens of a device tested
[SOURCE: ASTM F3172 -15: 2015, 3.1.13]
3.29
safety
freedom from unacceptable risk (3.25)
[SOURCE: ISO 14971:2019, 3.26]
3.30
severity
measure of the possible consequences of a hazard
[SOURCE: ISO 14971:2019, 3.27]
3.31
sterile barrier system
minimum package that minimizes the risk (3.25) of ingress of microorganisms and allows aseptic
presentation of the sterile contents at the point of use
[SOURCE: ISO 11607-1:2019, 3.23]
3.32
structural element
stent or frame component of a cardiac occluder (3.3)
3.33
withdrawal
removal of the occluder delivery system (3.8) with or without the cardiac occluder (3.3)
4 Abbreviations
For the purposes of this document, the following abbreviations apply.
ADE adverse device effect
AE adverse event
AFib atrial fibrillation
ASD atrial septic defect
CEC Clinical Events Committee
CIP clinical investigation plan
CMR cardiac magnetic resonance
CRF case report form
CT computed tomography
DIC disseminated intravascular coagulation
DSMB Data Safety Monitoring Board
EC Ethics Committee
GCP Good Clinical Practice
HIT heparin-induced thrombocytopenia
ICE intracardiac echocardiography
IFU instructions for use
IRB Institutional Review Board
LAA left atrial appendage
MRI magnetic resonance imaging
NYHA New York Heart Association
PCI percutaneous coronary intervention
PMCF post-market clinical follow-up
PDA patent ductus arteriosus
PET position emission tomography
PFO patent foramen ovale
PVL paravalvular leak
SADE serious adverse device effect
SAE serious adverse event
TEE transesophageal echocardiography
TTE transthoracic echocardiography
VSD ventricular septal defect
5 Fundamental requirements
5.1 General
The activities described within this document shall be carried out within a formal quality system.
NOTE ISO 13485 contains requirements for a suitable quality system for a medical manufacturer. Additional
requirements can be specified by a country or region.
5.2 Risk management
The manufacturer shall define, implement and document risk management activities in accordance
with ISO 14971. A risk-based methodology challenges the manufacturer to continually analyse and
evaluate known and theoretical risks of the device, to develop the most appropriate methods for
mitigating the risks of the device, and to implement the appropriate test, analysis methods, or rationale
to demonstrate the residual risks are acceptable (see Annex A).
Annex B provides an example of a hazard analysis to serve as a starting point for a risk analysis specific
to some cardiac occluder devices.
Annex I provides definitions and examples of adverse events that can be useful in the risk management
process.
As part of the risk management process, the manufacturer shall establish, document, implement and
maintain a usability engineering process, linked but distinct from the device design process, as detailed
in IEC 62366-1.
6 Device description
6.1 General
The requirements of ISO 14630 shall apply.
6.2 Intended use
The manufacturer shall identify the pathological condition(s) to be treated, the intended patient
population and intended claims. The manufacturer shall also consider the intended user(s) of the
medical device and the environments in which it is used.
6.3 Design inputs
6.3.1 Operational principles and specifications
The manufacturer shall define the operational specifications for the device including the principles of
operation, intended device delivery approach or process, durability, shelf life, shipping or storage limits,
and the physiological environment in which it is intended to function. The manufacturer shall define
relevant anatomical characteristics and device dimensional parameters that will be required to select
either the device model or size, or both. Additionally, if designed for periprocedural modification, define
how the device configuration will be determined (see Annex O and Annex G).
6.3.2 Functional, performance and safety requirements
6.3.2.1 General
The manufacturer shall establish (i.e. define, document and implement) the functional, performance
and safety requirements of the cardiac occluder system for the intended use and device claims.
6.3.2.2 Implantable device
The intended performance of the cardiac occluder device shall take into consideration at least the
following:
a) the ability to occlude undesired blood flow;
b) the ability to resist migration and embolization;
c) the ability to minimize haemolysis;
d) the ability to minimize undesired thrombus formation;
e) biocompatibility;
f) the ability to resist corrosion;
g) the ability to minimize particulate shedding;
h) compatibility with adjacent anatomical structures or other implanted devices, if applicable;
i) compatibility with diagnostic imaging techniques (e.g. MRI);
j) visibility under diagnostic imaging techniques (e.g. MRI, echocardiography, fluoroscopy, CT);
k) deliverability and implantability in the target population;
l) the ability to maintain structural and functional integrity during the expected lifetime of the
device;
m) the ability to maintain structural integrity, functionality and sterility for the labelled shelf life prior
to implantation;
n) the ability to be consistently and safely prepared for implantation;
o) the ability to be consistently and safely implanted in the intended implantation site and achieve the
aforementioned performance objectives;
p) the ability to be either safely retrieved, adjusted or repositioned, or all, if applicable.
NOTE See ISO 14630.
6.3.2.3 Access and delivery system
The functional, performance and safety requirements of the access and delivery system shall be
established (see Annex M). All supplied sterile single-use intravascular catheters shall follow
ISO 10555-1. If sterile single-use intravascular introducers, dilators or guidewires are supplied by the
manufacturer, then they shall follow ISO 11070, as applicable. For cardiac occluder systems which either
require or allow the user to select a non-supplied access system, the attributes of the non-supplied
access system shall be established for it to be compatible with the cardiac occluder delivery system.
These attributes include minimum inner diameter and length.
The design attributes shall take into consideration at least the following to meet the intended
performance of the delivery and access system:
a) compatibility of the access system, delivery system, and the cardiac occluder;
b) the ability to permit consistent, accurate and safe loading, access, delivery, deployment and release
of the cardiac occluder to the intended implantation site;
c) the ability to permit consistent and safe withdrawal of the delivery system prior to and after
deployment of the cardiac occluder device;
d) the ability to minimize thrombus formation;
e) the ability to minimize blood loss;
f) the ability to either retrieve, reposition, or remove the cardiac occluder device, or all, if applicable;
g) biocompatibility;
h) the ability to resist corrosion;
i) the ability to maintain integrity of the coating, if applicable;
j) the ability to minimize particulate generation;
k) the ability to maintain its functionality and sterility for the labelled shelf life;
l) compatibility and visibility with diagnostic imaging techniques (e.g. MRI, echo, fluoroscopy, CT), if
applicable;
m) compatibility with tools and accessories required to complete the procedure.
n) the ability to avoid air thrombus during the procedure;
o) the ability to inject contrast agent through the applicable changes of the procedure, if applicable.
6.3.3 Implant procedure: Device and usability requirements
The cardiac occluder system shall provide intended users the ability to safely and effectively perform
pre-operative, intra-operative, and post-operative procedural tasks to achieve desired outcome. This
shall include procedure-specific tools and accessories that intended users will need to complete the
procedure. In addition to establishing the device physical requirements during the implant procedure,
the usability engineering process according to IEC 62366-1 shall be used to establish user interface
characteristics that can be related to safety and effectiveness during the implant procedure.
6.3.4 Packaging, labelling and sterilization
The cardiac occluder system shall meet the requirements for packaging, labelling, and sterilization
contained within Annex C, Annex D, and Annex E, respectively.
The manufacturer shall provide information and guidance (e.g. imaging modalities and sizing procedure)
in the labelling to allow for appropriate preparation of the implantation site (e.g. left atrial appendage),
selection of appropriate implant size, implantation of the cardiac occluder, and post-procedure care and
medication, if applicable. The manufacturer shall also provide MRI safety information in the labelling.
See ISO 11135, ISO 11137-1, ISO 11137-2, ISO 11137-3, ISO 14160, ISO 14937, ISO 17665-1, ISO/TS 17665-2,
and ISO/TS 17665-3 for additional information regarding sterilization.
See ISO 11607-1 and ISO 11607-2 for additional information regarding packaging.
See ISO 15223-1, ISO 15223-2, and ASTM F2503 for additional information regarding labelling,
6.4 Design outputs
Design and development outputs shall meet the requirements of ISO 13485.
The manufacturer shall establish (i.e. define, document and implement) a specification of the
cardiac occluder system. In addition to the physical components of the cardiac occluder system, the
manufacturer shall establish instructions and specifications for the implant procedure. Instructions
shall meet the requirements of Annex D.
6.5 Design transfer (manufacturing verification or validation)
Design transfer requirements shall meet the requirements of ISO 13485.
The manufacturer shall establish (i.e. define, document and implement) the manufacturing process
operations and inspection steps including components and manufacturing materials.
As part of the risk management process, the manufacturer shall establish the control measures and
process conditions necessary to ensure that the process is capable of consistently delivering quality
product. The risk management file shall identify and justify the verification or validation activities
necessary to demonstrate the acceptability of the process settings chosen.
The manufacturer shall establish the adequacy of full-scale manufacturing by validation of the
manufacturing process (the installation qualification (IQ), operational qualification (OQ) and
performance qualification (PQ)).
7 Design verification and validation
7.1 General requirements
The manufacturer shall perform design verification to demonstrate that the design output of a cardiac
occluder system meets the design input. The manufacturer shall establish a design verification strategy
relating to hazards identified from the risk analysis. The protocols shall identify the test purpose, setup,
equipment (e.g. specifications, calibration), test conditions (with a justification of appropriateness to
anticipated in vivo operating conditions for the device, if applicable), acceptance criteria, and sample
quantities to be tested. Design verification includes testing, analyses, and other activities.
The manufacturer shall also validate the design of the cardiac occluder system to ensure that the device
meets user needs and intended use; refer to applicable sections of ISO 13485. The design verification
and validation shall address all risks identified in the risk assessment at the appropriate level.
[50]
NOTE See ISO/IEC 17025 regarding considerations for test method validation.
7.2 In vitro assessment
7.2.1 General
In vitro assessment shall be used, where appropriate, to demonstrate mitigation of risks identified in
the risk analysis through either design verification or validation, or both.
7.2.2 Test conditions, sample selection and reporting requirements
7.2.2.1 Test conditions
The test conditions for each in vitro assessment shall be defined and justified (see Annex G and Annex O
for examples of differential pressures).
7.2.2.2 Test sample selection
Test samples for either design verification or validation, or both, shall represent the cardiac occluder
system product intended for clinical use. Representative products include initial production units,
batches or their equivalents. Test samples shall be appropriately preconditioned prior to testing,
including exposure to the maximum number of allowed sterilization cycles, process chemicals, aging
effects, shipping/handling, in accordance with all manufacturing procedures and instructions for use,
where appropriate. Any deviations of the test samples from the finished product shall be justified.
The full range of available device configurations (e.g. sizes, deployment shapes, use ranges, delivery
system and accessories, and implant sites) shall be considered during selection of test samples; however,
depending on the particular test, testing does not necessarily have to be completed for each device
configuration.
For all tests, the number of samples shall be justified based on the specific intent of the test, with a
scientific justification. Additional information regarding sampling and sample conditioning, includi
...



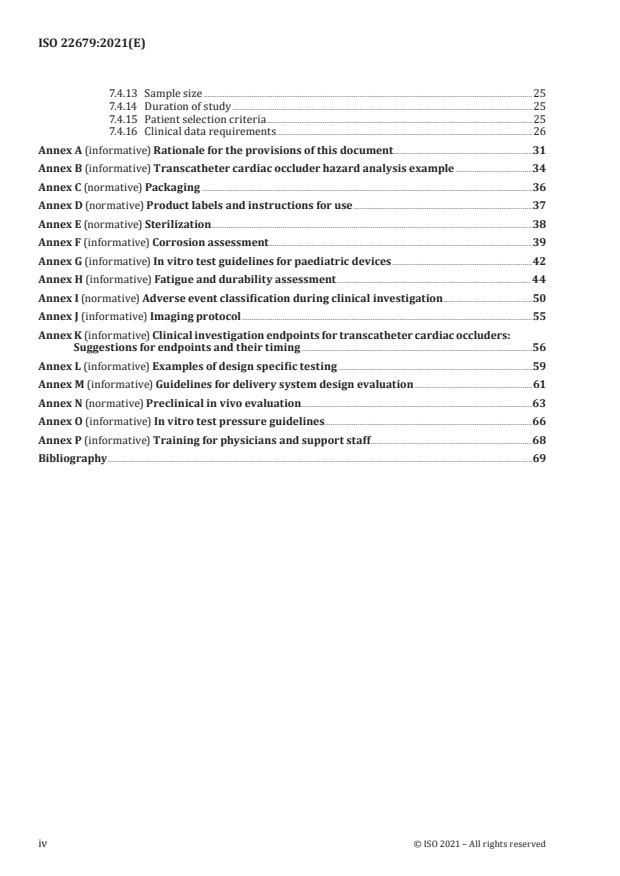
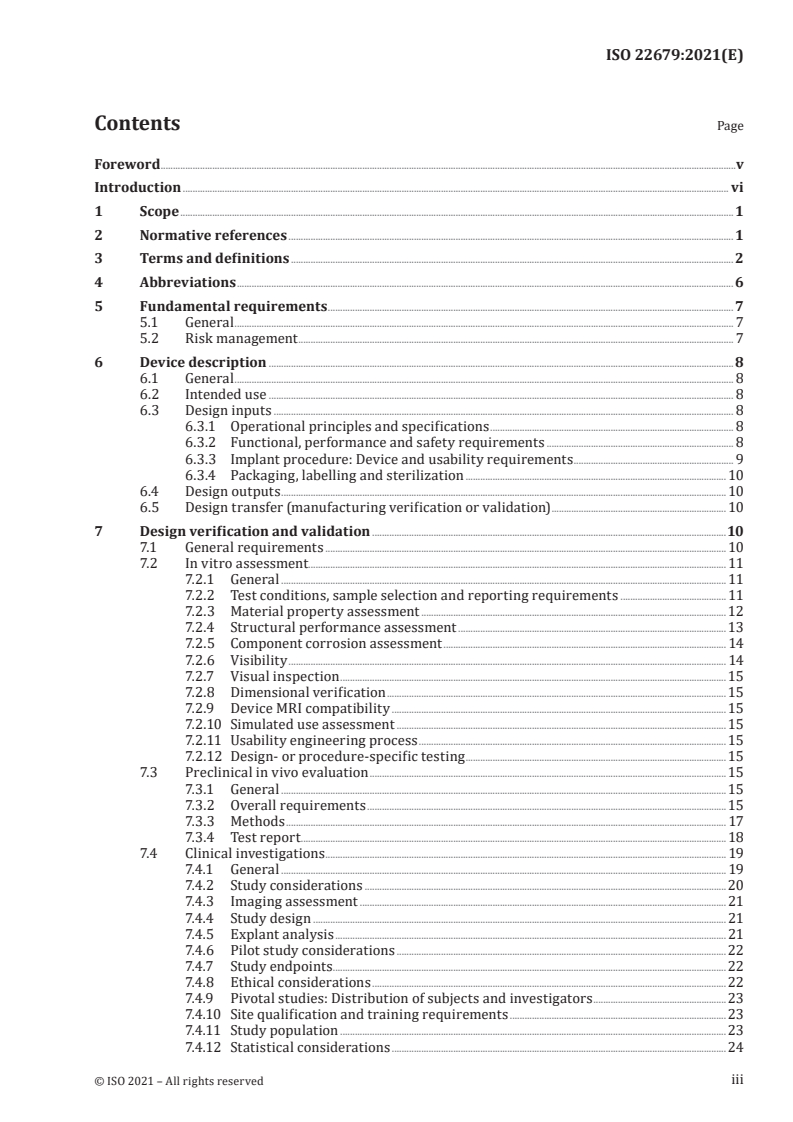
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...