SIST-TS CEN/TS 17811:2022
(Main)Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for urine and other body fluids - Isolated cell free DNA
Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for urine and other body fluids - Isolated cell free DNA
This document specifies requirements and gives recommendations on the handling, storage, processing and documentation of body fluids specimens intended for human cfDNA examination during the pre-examination phase before a molecular examination is performed.
This document is applicable to molecular in vitro diagnostic examinations performed by medical laboratories. It is also intended to be used by health institutions including facilities collecting and handling specimen, laboratory customers, in vitro diagnostics developers and manufacturers, biobanks, institutions and commercial organizations performing biomedical research, and regulatory authorities.
Dedicated measures that need to be taken for cytohistological analysis of body fluid derived nucleated cells are not described in this technical specification. Neither are measures for preserving and handling of pathogens, and other bacterial or whole microbiome DNA in body fluids described.
Different dedicated measures need to be taken for preserving ccfDNA from other body fluids such as blood, lymph and others. These are not described in this document. ccfDNA from blood is covered in EN ISO 20186-3.
NOTE International, national or regional regulations or requirements can also apply to specific topics covered in this document.
Molekularanalytische in-vitro-diagnostische Verfahren - Spezifikationen für präanalytische Prozesse für Urin und andere Körperflüssigkeiten - Isolierte zellfreie DNA
Dieses Dokument legt Anforderungen fest an und gibt Empfehlungen für die Handhabung, Lagerung, Verarbeitung und Dokumentation von für die Untersuchung von humaner cfDNA vorgesehenen Körperflüssigkeitenproben während der präanalytischen Phase vor der Durchführung einer molekularen Analyse.
Dieses Dokument ist anwendbar auf molekulare in vitro-diagnostische Untersuchungen, die in medizinischen Laboratorien durchgeführt werden. Es ist darüber hinaus für die Verwendung durch Gesundheitseinrichtungen, einschließlich Einrichtungen, die Primärproben entnehmen und handhaben, Laborkunden, Entwickler und Hersteller von In vitro-Diagnostika, Biobanken, in der biomedizinischen Forschung tätige Einrichtungen und kommerzielle Organisationen sowie Aufsichtsbehörden, vorgesehen.
Spezielle Maßnahmen, die bei der zytohistologischen Analyse von aus Körperflüssigkeiten entnommenen kernhaltigen Zellen erforderlich sind, werden in dieser Technischen Spezifikation nicht beschrieben. Des Weiteren werden auch keine Maßnahmen zur Konservierung und Handhabung von Pathogen- und sonstiger bakterieller oder Mikrobiom-DNA in Körperflüssigkeiten beschrieben.
Für die Konservierung von ccfDNA aus anderen Körperflüssigkeiten wie Blut, Lymphe u. a. müssen abweichende spezielle Maßnahmen getroffen werden. Diese werden nicht in diesem Dokument beschrieben. ccfDNA aus Blut ist Gegenstand von EN ISO 20186-3.
ANMERKUNG Für bestimmte Aspekte, die in diesem Dokument behandelt werden, können auch internationale, nationale oder regionale Bestimmungen oder Anforderungen gelten.
Molekularne diagnostične preiskave in vitro - Specifikacije za predpreiskovalne procese pregleda urina in drugih telesnih tekočin - Izolirana brezcelična DNK
Ta dokument določa zahteve ter podaja priporočila glede obravnave, shranjevanja, obdelave in dokumentiranja vzorcev telesnih tekočin, namenjenih za preiskave cirkulirajoče brezcelične DNK (cfDNA) med predpreiskovalno fazo, preden se izvede molekularna preiskava.
Ta dokument se uporablja za molekularne diagnostične preiskave in vitro, ki jih izvajajo v medicinskih laboratorijih. Uporabljale naj bi ga tudi zdravstvene ustanove, vključno z ustanovami, ki zbirajo in obravnavajo vzorce, laboratorijske stranke, razvijalci in proizvajalci diagnostike in vitro, biobanke, institucije in komercialne organizacije, ki izvajajo biomedicinske raziskave, ter regulativni organi.
V tej tehnični specifikaciji niso opisani namenski ukrepi za citohistološko analizo celic z jedri, pridobljenih iz telesnih tekočin. Prav tako niso opisani ukrepi za ohranjanje in ravnanje s patogeni ter drugo bakterijsko ali mikrobiomsko DNK v telesnih tekočinah.
Za ohranjanje cirkulirajoče brezcelične DNK iz drugih telesnih tekočin, kot so kri, limfa in ostale tekočine, je treba uporabiti drugačne namenske ukrepe. Slednji niso opisani v tem dokumentu. Cirkulirajoča brezcelična DNK iz krvi je obravnavana v standardu EN ISO 20186 3.
OPOMBA: Za določene teme, ki so zajete v tem dokumentu, lahko veljajo tudi mednarodni, nacionalni ali regionalni predpisi ali zahteve.
General Information
- Status
- Published
- Public Enquiry End Date
- 30-Mar-2022
- Publication Date
- 21-Aug-2022
- Technical Committee
- VAZ - Healthcare
- Current Stage
- 6060 - National Implementation/Publication (Adopted Project)
- Start Date
- 04-Aug-2022
- Due Date
- 09-Oct-2022
- Completion Date
- 22-Aug-2022
Relations
- Effective Date
- 28-Jan-2026
- Referred By
SIST EN ISO 9806:2026 - Solar energy - Solar thermal collectors - Test methods (ISO 9806:2025) - Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Referred By
SIST EN ISO 24194:2022 - Solar energy - Collector fields - Check of performance (ISO 24194:2022) - Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
- Effective Date
- 01-Feb-2023
Overview
CEN/TS 17811:2022 - "Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for urine and other body fluids - Isolated cell free DNA" - is a CEN Technical Specification that defines requirements and recommendations for the pre-examination handling of body fluid specimens intended for human cell‑free DNA (cfDNA) testing. It focuses on activities before the analytical molecular test begins, covering collection, transport, storage, processing and documentation to preserve native cfDNA profiles in urine and other non‑circulating body fluids.
Key topics and requirements
This specification addresses practical pre-analytical controls to maintain cfDNA integrity. Main technical topics include:
- Specimen collection: patient/donor information, selection of appropriate body fluid collection devices, and stabilization procedures.
- Transport requirements: procedures for transporting samples with or without cfDNA stabilizers and recommendations to limit degradation and contamination.
- Specimen reception and storage: checks on receipt, short‑term and long‑term storage conditions at the laboratory.
- Sample processing prior to cfDNA isolation: centrifugation, aliquoting and steps to avoid genomic DNA release from nucleated cells.
- cfDNA isolation: guidance on using commercial extraction kits versus laboratory‑developed procedures, and expectations for validation and documentation.
- Quality and quantity assessment: recommended assessment of isolated cfDNA (yield, integrity, potential inhibitors).
- Storage of isolated cfDNA: conditions and documentation for maintaining isolated material for downstream molecular assays.
- Documentation and traceability: recording of pre‑examination variables that affect analytical test performance.
The document explicitly excludes procedures for cytohistological analysis of nucleated cells, preservation and handling of pathogens or whole microbiome DNA, and dedicated measures for circulating cfDNA from blood (blood ccfDNA is covered by EN ISO 20186‑3). National or regional regulatory requirements can also apply.
Applications and users
CEN/TS 17811:2022 is intended for organizations involved in cfDNA molecular diagnostics and research, including:
- Medical laboratories performing molecular in vitro diagnostic tests on urine and other body fluids
- Health institutions and specimen collection sites (to implement proper collection and transport)
- In vitro diagnostics (IVD) developers and manufacturers (to design compatible collection devices and kits)
- Biobanks and research organizations handling cfDNA specimens
- Regulatory authorities and quality managers assessing pre‑analytical processes
Following this specification helps reduce pre‑analytical variability, improve assay sensitivity and reliability, and support reproducible cfDNA-based diagnostics (e.g., cancer biomarkers, liquid biopsy research).
Related standards
- EN ISO 15189 - Medical laboratories - Requirements for quality and competence (referenced normative standard).
- EN ISO 20186‑3 - Specifies pre‑analytical processes for blood ccfDNA (blood ccfDNA outside scope of CEN/TS 17811:2022).
Keywords: CEN/TS 17811:2022, cell‑free DNA, cfDNA, pre‑examination, specimen handling, urine, body fluids, molecular in vitro diagnostic, DNA stabilizers, sample transport, laboratory best practice.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
SIST-TS CEN/TS 17811:2022 is a technical specification published by the Slovenian Institute for Standardization (SIST). Its full title is "Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for urine and other body fluids - Isolated cell free DNA". This standard covers: This document specifies requirements and gives recommendations on the handling, storage, processing and documentation of body fluids specimens intended for human cfDNA examination during the pre-examination phase before a molecular examination is performed. This document is applicable to molecular in vitro diagnostic examinations performed by medical laboratories. It is also intended to be used by health institutions including facilities collecting and handling specimen, laboratory customers, in vitro diagnostics developers and manufacturers, biobanks, institutions and commercial organizations performing biomedical research, and regulatory authorities. Dedicated measures that need to be taken for cytohistological analysis of body fluid derived nucleated cells are not described in this technical specification. Neither are measures for preserving and handling of pathogens, and other bacterial or whole microbiome DNA in body fluids described. Different dedicated measures need to be taken for preserving ccfDNA from other body fluids such as blood, lymph and others. These are not described in this document. ccfDNA from blood is covered in EN ISO 20186-3. NOTE International, national or regional regulations or requirements can also apply to specific topics covered in this document.
This document specifies requirements and gives recommendations on the handling, storage, processing and documentation of body fluids specimens intended for human cfDNA examination during the pre-examination phase before a molecular examination is performed. This document is applicable to molecular in vitro diagnostic examinations performed by medical laboratories. It is also intended to be used by health institutions including facilities collecting and handling specimen, laboratory customers, in vitro diagnostics developers and manufacturers, biobanks, institutions and commercial organizations performing biomedical research, and regulatory authorities. Dedicated measures that need to be taken for cytohistological analysis of body fluid derived nucleated cells are not described in this technical specification. Neither are measures for preserving and handling of pathogens, and other bacterial or whole microbiome DNA in body fluids described. Different dedicated measures need to be taken for preserving ccfDNA from other body fluids such as blood, lymph and others. These are not described in this document. ccfDNA from blood is covered in EN ISO 20186-3. NOTE International, national or regional regulations or requirements can also apply to specific topics covered in this document.
SIST-TS CEN/TS 17811:2022 is classified under the following ICS (International Classification for Standards) categories: 11.100.10 - In vitro diagnostic test systems. The ICS classification helps identify the subject area and facilitates finding related standards.
SIST-TS CEN/TS 17811:2022 has the following relationships with other standards: It is inter standard links to SIST EN ISO 15189:2023, SIST EN ISO 9806:2026, SIST EN 17888-1:2024, SIST-TS CEN/TS 17981-1:2024, SIST EN ISO 24194:2022, SIST EN 17887-1:2024, kSIST FprEN ISO 18704:2025. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
SIST-TS CEN/TS 17811:2022 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-september-2022
Molekularne diagnostične preiskave in vitro - Specifikacije za predpreiskovalne
procese pregleda urina in drugih telesnih tekočin - Izolirana brezcelična DNK
Molecular in vitro diagnostic examinations - Specifications for pre-examination processes
for urine and other body fluids - Isolated cell free DNA
Molekularanalytische in-vitro-diagnostische Verfahren - Spezifikationen für
präanalytische Prozesse für Urin und andere Körperflüssigkeiten - Isolierte zellfreie DNA
Ta slovenski standard je istoveten z: CEN/TS 17811:2022
ICS:
11.100.10 Diagnostični preskusni In vitro diagnostic test
sistemi in vitro systems
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
CEN/TS 17811
TECHNICAL SPECIFICATION
SPÉCIFICATION TECHNIQUE
June 2022
TECHNISCHE SPEZIFIKATION
ICS 11.100.10
English Version
Molecular in vitro diagnostic examinations - Specifications
for pre-examination processes for urine and other body
fluids - Isolated cell free DNA
Molekularanalytische in-vitro-diagnostische Verfahren
- Spezifikationen für präanalytische Prozesse für Urin
und andere Körperflüssigkeiten - Isolierte zellfreie
DNA
This Technical Specification (CEN/TS) was approved by CEN on 17 May 2022 for provisional application.
The period of validity of this CEN/TS is limited initially to three years. After two years the members of CEN will be requested to
submit their comments, particularly on the question whether the CEN/TS can be converted into a European Standard.
CEN members are required to announce the existence of this CEN/TS in the same way as for an EN and to make the CEN/TS
available promptly at national level in an appropriate form. It is permissible to keep conflicting national standards in force (in
parallel to the CEN/TS) until the final decision about the possible conversion of the CEN/TS into an EN is reached.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2022 CEN All rights of exploitation in any form and by any means reserved Ref. No. CEN/TS 17811:2022 E
worldwide for CEN national Members.
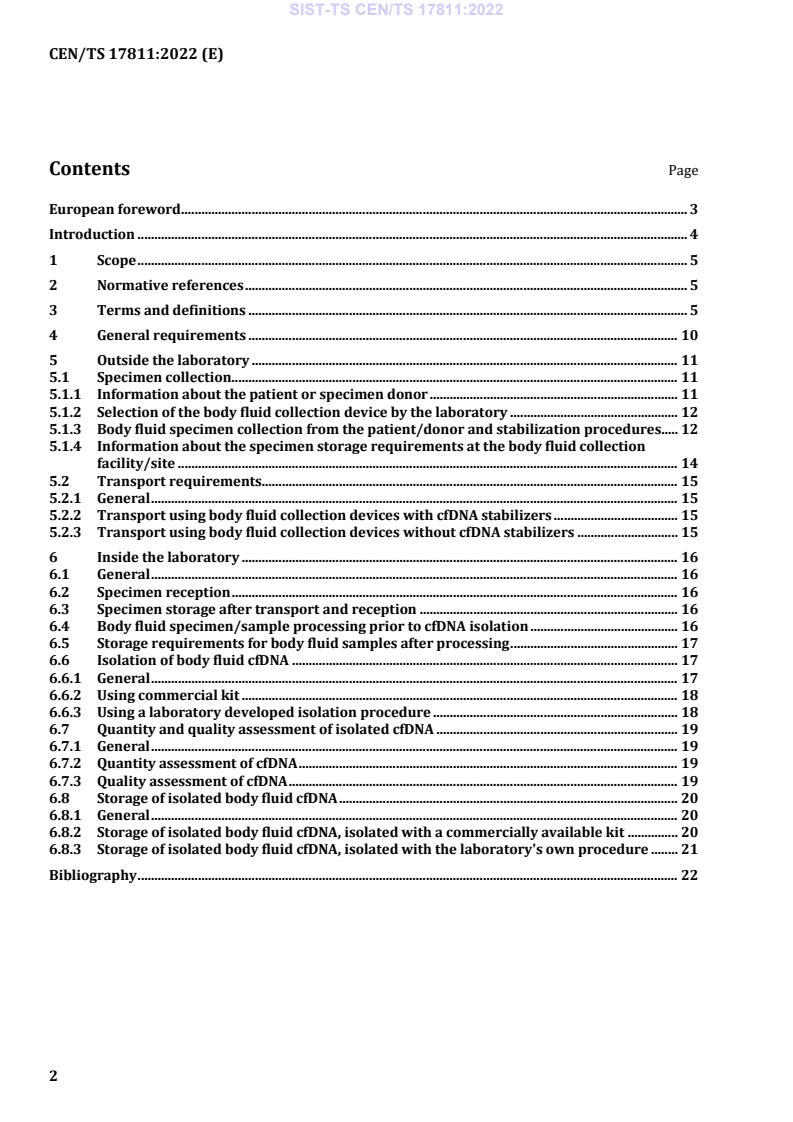
Contents Page
European foreword . 3
Introduction . 4
1 Scope . 5
2 Normative references . 5
3 Terms and definitions . 5
4 General requirements . 10
5 Outside the laboratory . 11
5.1 Specimen collection . 11
5.1.1 Information about the patient or specimen donor . 11
5.1.2 Selection of the body fluid collection device by the laboratory . 12
5.1.3 Body fluid specimen collection from the patient/donor and stabilization procedures. 12
5.1.4 Information about the specimen storage requirements at the body fluid collection
facility/site . 14
5.2 Transport requirements. 15
5.2.1 General . 15
5.2.2 Transport using body fluid collection devices with cfDNA stabilizers . 15
5.2.3 Transport using body fluid collection devices without cfDNA stabilizers . 15
6 Inside the laboratory . 16
6.1 General . 16
6.2 Specimen reception . 16
6.3 Specimen storage after transport and reception . 16
6.4 Body fluid specimen/sample processing prior to cfDNA isolation . 16
6.5 Storage requirements for body fluid samples after processing . 17
6.6 Isolation of body fluid cfDNA . 17
6.6.1 General . 17
6.6.2 Using commercial kit . 18
6.6.3 Using a laboratory developed isolation procedure . 18
6.7 Quantity and quality assessment of isolated cfDNA . 19
6.7.1 General . 19
6.7.2 Quantity assessment of cfDNA . 19
6.7.3 Quality assessment of cfDNA . 19
6.8 Storage of isolated body fluid cfDNA . 20
6.8.1 General . 20
6.8.2 Storage of isolated body fluid cfDNA, isolated with a commercially available kit . 20
6.8.3 Storage of isolated body fluid cfDNA, isolated with the laboratory's own procedure . 21
Bibliography . 22
European foreword
This document (CEN/TS 17811:2022) has been prepared by Technical Committee CEN/TC 140 “In vitro
diagnostic medical devices”, the secretariat of which is held by DIN.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN-CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to implement this European Standard: Austria, Belgium, Bulgaria, Croatia,
Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland,
Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of North
Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and the United
Kingdom.
Introduction
Molecular in vitro diagnostics has enabled a significant progress in medicine. Further progress is expected
by new technologies analysing profiles of nucleic acids, proteins, and metabolites in human tissues and
body fluids. However, the profiles of these molecules can change drastically during specimen collection,
transport, storage and processing thus making the outcome from diagnostics or research unreliable or
even impossible because the subsequent analytical assay will not determine the situation in the patient
but an artificial profile generated during the pre-examination process.
Most of the DNA in the body is located within cells, but a small amount of nucleic acids can also be found
outside of cells, so called cell-free DNA (cfDNA). In case of circulating body fluids such as blood, this DNA
is called circulating cell-free DNA (ccfDNA) and in case of non-circulating body fluids such as urine, saliva,
cerebrospinal fluid, pleural effusion, ascites, and synovial fluid, the DNA is called cell-free DNA (cfDNA).
cfDNA is of specific interest, as for example cfDNA in urine originates from cells from the genitourinary
tract or from ccfDNA in circulation passing through glomerular filtration [1]. cfDNA from cancerous or
malignant cells in urine have been associated with cancer specific sequences, epigenetic and structural
changes [2], [3].
Standardization of the entire workflow from specimen collection to the cfDNA examination is needed to
minimize release of DNA from cells into the fluid, and degradation of cfDNA in the specimen, which can
change the original native cfDNA profile in the body fluid after specimen collection. Post collection
microbial growth in the specimen can further enhance the degradation of the cfDNA, e.g. in urine and
saliva. Studies have been undertaken to determine the important influencing factors as they can impact
the sensitivity and reliability of cfDNA examination from urine and other body fluids.
This document draws upon such work to codify and standardize the steps for cfDNA examination from
body fluids in what is referred to as the pre-examination phase.
In this document, the following verbal forms are used:
— “shall” indicates a requirement;
— “should” indicates a recommendation;
— “may” indicates a permission;
— “can” indicates a possibility or a capability.
1 Scope
This document specifies requirements and gives recommendations on the handling, storage, processing
and documentation of body fluids specimens intended for human cfDNA examination during the pre-
examination phase before a molecular examination is performed.
This document is applicable to molecular in vitro diagnostic examinations performed by medical
laboratories. It is also intended to be used by health institutions including facilities collecting and
handling specimen, laboratory customers, in vitro diagnostics developers and manufacturers, biobanks,
institutions and commercial organizations performing biomedical research, and regulatory authorities.
Dedicated measures that need to be taken for cytohistological analysis of body fluid derived nucleated
cells are not described in this technical specification. Neither are measures for preserving and handling
of pathogens, and other bacterial or whole microbiome DNA in body fluids described.
Different dedicated measures need to be taken for preserving ccfDNA from other body fluids such as
blood, lymph and others. These are not described in this document. ccfDNA from blood is covered in
EN ISO 20186-3.
NOTE International, national or regional regulations or requirements can also apply to specific topics covered
in this document.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
EN ISO 15189, Medical laboratories - Requirements for quality and competence (ISO 15189)
3 Terms and definitions
For the purposes of this document, the terms and definitions given in EN ISO 15189 and the following
terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https://www.iso.org/obp
— IEC Electropedia: available at http://www.electropedia.org/
3.1
aliquot
portion of a larger amount of homogenous material, assumed to be taken with negligible sampling error
Note 1 to entry: The term is usually applied to fluids. Tissues are heterogeneous and therefore cannot be
aliquoted.
Note 2 to entry: The definition is derived from [4], [5] and [6].
3.2
ambient temperature
unregulated temperature of the surrounding air
3.3
analyte
component represented in the name of a measurable quantity
[SOURCE: EN ISO 17511:2021, 3.1 — Deleted example.]
3.4
analytical test performance
analytical performance
examination performance
accuracy, precision, and sensitivity of a test to measure the analyte of interest
Note 1 to entry: Other test performance characteristics such as robustness, repeatability can apply as well.
[SOURCE: EN ISO 20184-1:2018, 3.4]
3.5
ascites
abnormal build-up of fluid in the abdomen that can cause swelling
Note 1 to entry: In late-stage cancer, tumour cells can be found in the fluid in the abdomen.
Note 2 to entry: Ascites also occurs in patients with liver disease.
Note 3 to entry: This definition was derived from [7].
3.6
body fluid collection device
tube or other container in which the body fluid (e.g. urine) specimen is collected
3.7
ccfDNA
circulating cell free DNA
extracellular human DNA present in blood and plasma
Note 1 to entry: ccfDNA can include DNA present in vesicles such as exosomes.
[SOURCE: EN ISO 20186-3:2019, 3.5]
3.8
cfDNA
cell free DNA
extracellular human DNA present in body liquids such as urine
Note 1 to entry: cfDNA can include DNA present in vesicles such as exosomes [8].
3.9
cfDNA profile
cell free DNA profile
amount of different cfDNA molecules, that are present in a body liquid, that can be measured in the
absence of any losses, inhibition and interference
3.10
closed system
non-modifiable system provided by the vendor including all necessary components for the analysis (i.e.,
hardware, software, procedures and reagents)
3.11
CSF
cerebrospinal fluid
fluid that flows in and around the hollow spaces of the brain and spinal cord, and between two of the
meninges (the thin layers of tissue that cover and protect the brain and spinal cord)
Note 1 to entry: Cerebrospinal fluid is made by tissue called the choroid plexus in the ventricles (hollow spaces)
in the brain.
Note 2 to entry: This definition was derived from [7].
3.12
DNA
deoxyribonucleic acid
polymer of deoxyribonucleotides occurring in a double-stranded (dsDNA) or single-stranded (ssDNA)
form
[SOURCE: EN ISO 22174:2005, 3.1.2]
3.13
DNA stabilizers
compounds, solutions or mixtures that are designed to minimize degradation and fragmentation of cfDNA
as well as release of genomic DNA from nucleated cells
3.14
examination
analytical test
set of operations having the object of determining the value or characteristics of a property
Note 1 to entry: Processes that start with the isolated measurand and include all kinds of parameter testing or
chemical manipulation for quantitative or qualitative examination.
[SOURCE: EN ISO 15189:2012, 3.7, modified — Term and definition are used here without the original
notes; an additional term was added.]
3.15
examination manufacturer
analytical test manufacturer
entity that manufactures and/or produces a specific analytical test
[SOURCE: CEN/TS 17747:2021, 3.9 — Deleted Note.]
3.16
examination performance
analytical test performance
analytical performance
accuracy, precision, and sensitivity of a test to measure the analyte of interest
Note 1 to entry: Other test performance characteristics such as robustness, repeatability can apply as well.
[SOURCE: EN ISO 20184-1:2018, 3.4]
3.17
genomic DNA
gDNA
genomic DNA present in nucleated cells
3.18
homogenous
uniform in structure and composition
3.19
interfering substances
endogenous or exogenous substances (e.g. stabilization solution) that can be present in specimens and
that can alter an examination result
3.20
microorganisms
entity of microscopic size, encompassing bacteria, fungi, protozoa and viruses
[SOURCE: ISO 18362:2016, 3.18]
3.21
pleural effusion
abnormal collection of fluid between the thin layers of tissue (pleura) lining the lung and the wall of the
chest cavity
Note 1 to entry: This definition was derived from [7].
3.22
pre-examination processes
pre-analytical phase
pre-analytical workflow
pre-examination phase
processes that start, in chronological order, from the clinician’s request and include the examination
request, preparation and identification of the patient, collection of the primary sample(s), transportation
to and within the analytical laboratory, storage, isolation of analytes, and end when the analytical
examination begins
Note 1 to entry: The pre-examination phase includes preparative processes that influence the outcome of the
intended examination.
[SOURCE: EN ISO 15189:2012, 3.15, modified — An additional term was added and more detail was
included.]
3.23
primary sample
specimen
discrete portion of a body fluid, breath, hair or tissue taken for examination, study or analysis of one or
more quantities or properties assumed to apply for the whole
[SOURCE: EN ISO 15189:2012, 3.16, modified — The term and definition are used here without the
original notes.]
3.24
proficiency test
evaluation of participant performance against pre-established criteria by means of inter-laboratory
comparisons
[SOURCE: EN ISO/IEC 17043:2010, 3.7, modified — Term and definition are used here without the
original notes.]
3.25
room temperature
temperature in the range of 18 °C to 25 °C
Note 1 to entry: Local or national regulations can have different definitions.
[SOURCE: EN ISO 20166-1:2018, 3.22]
3.26
sample
one or more parts taken from a primary sample
[SOURCE: EN ISO 15189:2012, 3.24, modified — Example has been removed.]
3.27
stability
ability of a sample material, when stored under specified conditions, to maintain a stated property value
within specified limits for a specified period of time
Note 1 to entry: The measurand constituent for the purpose of this document is isolated DNA.
[SOURCE: ISO Guide 30:2015, 2.1.15, modified — The words “reference material” were replaced by
“sample material”.]
3.28
storage
prolonged interruption of the pre-analytical workflow of a sample or analyte respectively, or of their
derivatives, under appropriate conditions in order to preserve their properties
Note 1 to entry: Long-term storage typically occurs in laboratory archives or in biobanks.
[SOURCE: EN ISO 20184-1:2018, 3.21, modified — Example has been removed.]
3.29
synovial fluid
transparent, sticky liquid produced in joints (i.e. places where two bones are connected) that allows the
bones and tendons to move smoothly
Note 1 to entry: In pathological situations the collected synovial fluid can have a different colour.
Note 2 to entry: This definition was derived from [9].
3.30
urine
liquid product of the human excretory system produced by the kidneys and expelled through the urethra
via urination (i.e. micturition)
[SOURCE: ISO 30500:2018, 3.1.2.3]
3.31
validation
confirmation, throughout the provision of objective evidence, that the requirements for a specific
intended use or application have been fulfilled
Note 1 to entry: The term “validated” is used to designate the corresponding status.
[SOURCE: EN ISO 9000:2015, 3.8.13, modified — Note 1 and 3 have been omitted.]
3.32
verification
confirmation, through provision of objective evidence, that specified requirements have been fulfilled
Note 1 to entry: The term “verified” is used to designate the corresponding status.
Note 2 to entry: Confirmation can comprise activities such as:
— performing alternative calculations;
— comparing a new design specification with a similar proven design specification;
— undertaking tests and demonstrations; and
— reviewing documents prior to issue
[SOURCE: EN ISO 9000:2015, 3.8.12, modified — Note 1 and Note 2 have been omitted.]
3.33
workflow
series of activities necessary to complete a task
[SOURCE: EN ISO 20166-1:2018, 3.30]
4 General requirements
For general statements on medical laboratory quality management systems and in particular on
specimen collection, reception and handling (including avoidance of cross contaminations) see
EN ISO 15189 and EN ISO/IEC 17020 or EN ISO/IEC 17025. ISO/TS 20658 and EN ISO 20387 (for
biobanking) can also apply. The requirements on laboratory equipment, reagents, and consumables
according to EN ISO 15189 shall be followed; EN ISO 15189 shall be followed; EN ISO/IEC 17020 and
EN ISO/IEC 17025 can also apply.
All steps of the pre-examination, examination and post-examination processes (i.e. the entire workflow)
can influence the diagnosis or research study results.
Thus, this entire workflow shall be specified, verified and validated during the development of the
examination, including the development of in vitro diagnostic (IVD) medical devices. This includes
specifically all pre-examination process steps such as the examination request, preparation and
identification of the patient, collection of the primary sample(s), transport to and within the medical
laboratory, storage and isolation of analytes.
The stability of the cfDNA profile should be investigated throughout the complete pre-examination
process development. The verification and validation shall take into account the variability of the body
fluid specimen's quality. cfDNA profiles can change significantly after body fluid collection. The post-
collection release of genomic DNA from cells in the body fluid can change the cfDNA profile (see [10]). In
some body fluids, such as urine, post-collection growth of bacteria can cause additional changes to the
cfDNA profile such as contaminating the human cfDNA with bacterial DNA and causing degradation of
target cfDNA. Other post-collection effects can also result in cfDNA degradation. Post-collection changes
can vary individually in specimens from different donors or patients, and they can also depend on
pathophysiological conditions. This can impact the validity and reliability of the examination results.
During the design and development of a cfDNA based examination, a risk assessment shall be performed
(see also EN ISO 14971). Mitigation measures for eliminating or reducing identified risks shall be
established where required for ensuring the performance of the examination. It shall especially be
investigated and ensured that the cfDNA profile(s) intended to be analysed is/are not compromised
during the pre-examination process in a manner impacting the examination performance. This includes
investigations on whether and/or how the profile intended to be examined changes during all pre-
analytical process steps (e.g. degradation of target cfDNA, and the post-collection release of genomic DNA
from present cells). This can be done, e.g. by applying the intended examination to specimens/samples
which underwent time course studies reflecting the individual pre-examination process steps such as
transport and storage and by implementing measures to prevent or reduce impacts by the identified pre-
analytical variables, e.g. by using body fluid collection devices with cfDNA stabilizers.
During the whole pre-examination process, precautions shall be taken to avoid cross contamination
between different samples/specimens (e.g. by using single-use material whenever feasible or
appropriate cleaning procedures between processing of different specimens/samples) and to avoid
mixing up of specimens/samples.
Safety instructions for the whole pre-examination process shall be in place and followed. Safety
regulations on specimen/sample transport and handling shall be considered (see EN ISO 15189,
ISO 15190 and ISO/TS 20658). If transport is required over public areas, corresponding regulations or
laws for packaging and transport apply (e.g. International Air Transport Association (IATA) for air
transport).
The manufacturer's material safety data sheet should be considered before first use of any potentially
hazardous material (e.g. chemicals in stabilizers).
For all pre-examination steps, the examination manufacturer's instructions shall be followed, if provided.
Where, for justified reasons (e.g. unmet patient needs), a commercial product is not used in accordance
with the manufacturer's instructions, responsibility for its verification, validation, use and performance
lies with the laboratory.
5 Outside the laboratory
5.1 Specimen collection
5.1.1 Information about the patient or specimen donor
The documentation shall include the identity of the patient or specimen donor, which can be in the form
of a code.
The documentation should include, but is not limited to:
a) the relevant health status of the patient or specimen donor (e.g. healthy, disease type, concomitant
disease, demographics [e.g. age and gender]);
b) the information about medical treatment and special treatment prior to body fluid collection (e.g.
anaesthetics, medications, fasting status, surgical or diagnostic procedures);
c) the type and the purpose of the examination requested;
d) the appropriate consent from the patient or specimen donor.
See also EN ISO 15189.
5.1.2 Selection of the body fluid collection device by the laboratory
The cfDNA profile of body fluids can be influenced by inadequate collection procedures, inappropriate
storage/transport conditions, separation of contaminating cells as well as by cfDNA isolation procedures.
Specifically, the post-collection degradation can change the cfDNA profile in body fluids, e.g. in urine
significantly [11], [12]. This can impact the validity of the examination results.
In order to prevent cfDNA degradation, bacterial growth and, where required, genomic DNA release from
cells, body fluid collection devices with cfDNA profile stabilizers, or devices without stabilizers with
immediate post-collection addition of stabilizers should be used. These stabilizers should also allow the
separation of nucleated cells from cfDNA in the body fluid, e.g. by centrifugation. Body fluid collection
without cfDNA profile stabilizers should only be used, if the ordered examination specifications allow the
non-use of stabilizers.
The examination manufacturer's instructions for use for the collection of the specimen shall be followed.
Where the cfDNA examination manufacturer requires usage of a dedicated body fluid collection device or
body fluid cfDNA stabilizer, these shall be used. This can include a transfer into a secondary container
with a stabilizer. The device's and stabilizers' catalogue and lot numbers should be documented.
For specimens intended for extended storage in a biobank it is usually not known which individual human
cfDNA examinations will be performed after the extended storage. Therefore, body fluid collection
devices with cfDNA profile stabilizers should be used to enable the use of a wider range of examinations.
5.1.3 Body fluid specimen collection from the patient/donor and stabilization procedures
5.1.3.1 General
The body fluid collection device manufacturer shall provide specified and verified instructions on the
body fluid collection procedure. These shall be followed as long as not specified differently by the
examination manufacturer. The laboratory shall have written instructions for body fluid collection in
place following the body fluid collection device manufacturer's and/or the examination manufacturer's
requirements.
Where self-collection is possible (e.g. saliva, urine), written and/or visual instructions, for example from
the manufacturer, the laboratory or physician, following the body fluid collection device manufacturer's
and/or the examination manufacturer's requirements shall be supplied to the patient/donor.
The instructions for body fluid specimen collection shall include:
1) all the requirements necessary for the identification, collection, storage and transport to the
laboratory. For collection this shall include requirements:
a) to collect the specified specimen volume;
b) to mix the specimen with the stabilizers immediately after body fluid specimen collection e.g. by
shaking or inverting;
2) requirements and recommendations to follow before the collection, in particular related to e.g.
drinking and/or fasting before collection, or collection time, e.g. first midstream urine of the morning.
For self-collection, the patient/donor shall be provided with an appropriate body fluid collection device
(e.g. container, tube), identity tag(s) (e.g. label, RFID), and in general anything needed for the specimen
collection, preservation, storage and transport procedure for returning the specimen to laboratory.
The patient/donor shall also be provided with an option to confirm compliance with the supplied
instructions for the body fluid specimen collection, e.g. electronic, paper based.
The patient/donor or person collecting the specimen in the patient's/donor's stead shall confirm
compliance with the supplied instructions for the body fluid specimen collection.
The identity of the person collecting the specimen shall be documented. This can e.g. be done in form of
the name or a code. The date and time of body fluid collection shall be documented.
For the labelling (sample/specimen identification) of the body fluid collection device, a routine procedure
(EN ISO 15189 for medical laboratories or EN ISO 20387 for biobanks) or a procedure with additional
information (e.g. 2D-barcode) shall be used.
Any tampering with and/or additions to the specimen shall be documented.
Where, for justified reasons (e.g. unmet patient needs), a commercial product is not used in accordance
with the manufacturer's instructions, responsibility for its verification, validation, use and performance
lies with the laboratory.
5.1.3.2 Body fluid collection with cfDNA stabilizers
The examination manufacturer's instructions for use of the body fluid collection device and/or cfDNA
stabilizers shall be followed for specimen collection and stabilization.
The examination manufacturer's instructions for use of the body fluid collection device and/or cfDNA
stabilizers may refer to the instructions of the body fluid collection device manufacturer and/or stabilizer
ma
...



Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...