ISO/TR 14639-1:2012
(Main)Health informatics — Capacity-based eHealth architecture roadmap — Part 1: Overview of national eHealth initiatives
Health informatics — Capacity-based eHealth architecture roadmap — Part 1: Overview of national eHealth initiatives
ISO/TR 14639-1:2012 aims to identify the business requirements of an eHealth architecture as well as providing a generic and comprehensive context description to inform architectural structuring of Health Information Systems (HIS). ISO/TR 14639-1:2012 reviews international experiences in the construction of national eHealth architectures and introduces a methodology for strategic development of HIS.
Informatique de santé — Feuille de route de l'architecture de santé électronique fondée sur la capacité — Partie 1: Aperçu des initiatives de santé électronique nationale
General Information
- Status
- Published
- Publication Date
- 07-Aug-2012
- Technical Committee
- ISO/TC 215 - Health informatics
- Drafting Committee
- ISO/TC 215/WG 1 - Architecture, Frameworks and Models
- Current Stage
- 6060 - International Standard published
- Start Date
- 08-Aug-2012
- Due Date
- 25-Jan-2013
- Completion Date
- 25-Jan-2013
Overview
ISO/TR 14639-1:2012 - "Health informatics - Capacity-based eHealth architecture roadmap - Part 1: Overview of national eHealth initiatives" provides a descriptive, practice-oriented review of how countries design and develop national eHealth architecture and health information systems (HIS). The Technical Report identifies the business requirements for a national eHealth architecture, offers a generic context description to inform architectural structuring, and introduces a methodology for strategic HIS development. It is intended particularly for nations in early to mid stages of HIS evolution and supports migration from paper-based to semi-automated and fully automated information management.
Key Topics and Requirements
- Business requirements for eHealth architecture: high-level needs that guide national HIS planning and deployment.
- Contextual architecture description: generic components, functions and inter-relationships for enterprise-wide HIS.
- Review of international initiatives: case studies and lessons from multiple countries (e.g., Australia, Brazil, Canada, India, Kenya) and initiatives such as the Health Metrics Network.
- Standards and governance: discussion of standards in use, Standards Development Organizations (SDOs) and national health informatics associations.
- Data management components: role and definition of national data warehouses, reporting infrastructures for individual and aggregate data.
- Monitoring & evaluation frameworks: alignment with international indicator frameworks and donor programs.
- Need for an eHealth Architecture Maturity Model (eHAMM): rationale and introduction to a maturity model for assessing and planning HIS development (to be elaborated in ISO/TR 14639-2).
- Migration path: principles for progressing from manual data collection to automated, interoperable systems.
Applications - Who Should Use This Standard
ISO/TR 14639-1:2012 is useful for:
- National health ministries and CIOs planning or maturing eHealth architecture and HIS strategies.
- Enterprise architects and system designers defining component models and interoperability boundaries.
- Policy-makers and program managers designing national eHealth roadmaps and capacity-building programs.
- Donors, NGOs and international agencies assessing readiness and aligning investments with national HIS needs.
- Vendors and integrators seeking to understand national-level requirements and standards alignment.
Practical applications include strategic planning, gap analysis, maturity assessment (using eHAMM), standards selection, and designing scalable data warehouses and national reporting systems.
Related Standards
- ISO/TR 14639-2 (under preparation) - Architectural components and maturity model (eHAMM).
- ISO/TS 16555 - Framework for national health information systems (complements the TR).
- Developed under ISO/TC 215 (Health informatics).
Keywords: ISO/TR 14639-1:2012, eHealth architecture, national eHealth initiatives, health information systems, HIS, eHAMM, health informatics, national data warehouse.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

NYCE
Mexican standards and certification body.
Sponsored listings
Frequently Asked Questions
ISO/TR 14639-1:2012 is a technical report published by the International Organization for Standardization (ISO). Its full title is "Health informatics — Capacity-based eHealth architecture roadmap — Part 1: Overview of national eHealth initiatives". This standard covers: ISO/TR 14639-1:2012 aims to identify the business requirements of an eHealth architecture as well as providing a generic and comprehensive context description to inform architectural structuring of Health Information Systems (HIS). ISO/TR 14639-1:2012 reviews international experiences in the construction of national eHealth architectures and introduces a methodology for strategic development of HIS.
ISO/TR 14639-1:2012 aims to identify the business requirements of an eHealth architecture as well as providing a generic and comprehensive context description to inform architectural structuring of Health Information Systems (HIS). ISO/TR 14639-1:2012 reviews international experiences in the construction of national eHealth architectures and introduces a methodology for strategic development of HIS.
ISO/TR 14639-1:2012 is classified under the following ICS (International Classification for Standards) categories: 35.240.80 - IT applications in health care technology. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO/TR 14639-1:2012 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
INTERNATIONAL ISO/TR
STANDARD 14639-1
First edition
2012-08-15
Health informatics — Capacity-based
eHealth architecture roadmap —
Part 1:
Overview of national eHealth initiatives
Informatique de santé — Feuille de route de l'architecture de santé
électronique fondée sur la capacité —
Partie 1: Aperçu des initiatives de santé électronique nationale
Reference number
©
ISO 2012
© ISO 2012
All rights reserved. Unless otherwise specified, no part of this publication may be reproduced or utilized in any form or by any means,
electronic or mechanical, including photocopying and microfilm, without permission in writing from either ISO at the address below or
ISO's member body in the country of the requester.
ISO copyright office
Case postale 56 CH-1211 Geneva 20
Tel. + 41 22 749 01 11
Fax + 41 22 749 09 47
E-mail copyright@iso.org
Web www.iso.org
Published in Switzerland
ii © ISO 2012 – All rights reserved
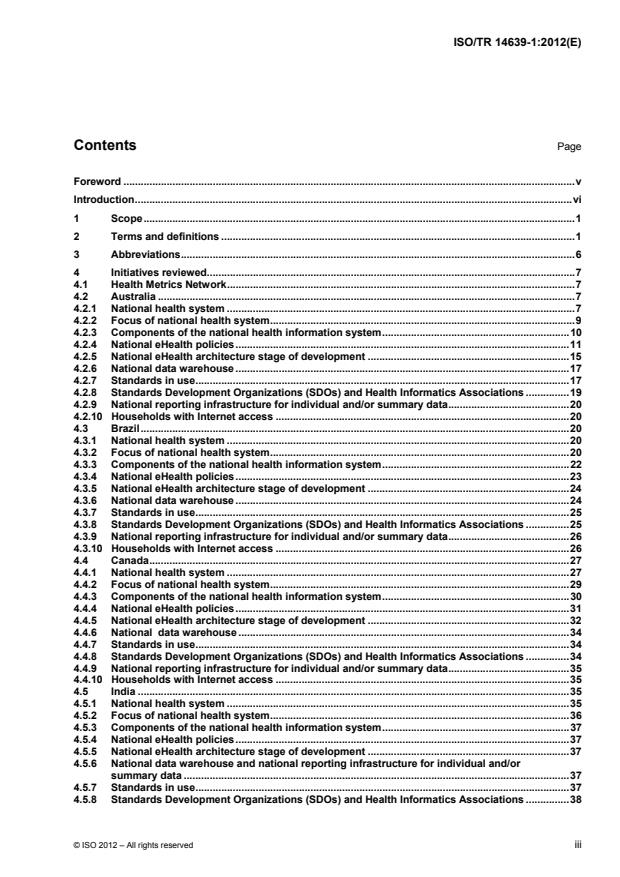
Contents Page
Foreword . v
Introduction . vi
1 Scope . 1
2 Terms and definitions . 1
3 Abbreviations . 6
4 Initiatives reviewed . 7
4.1 Health Metrics Network . 7
4.2 Australia . 7
4.2.1 National health system . 7
4.2.2 Focus of national health system . 9
4.2.3 Components of the national health information system . 10
4.2.4 National eHealth policies . 11
4.2.5 National eHealth architecture stage of development . 15
4.2.6 National data warehouse . 17
4.2.7 Standards in use . 17
4.2.8 Standards Development Organizations (SDOs) and Health Informatics Associations . 19
4.2.9 National reporting infrastructure for individual and/or summary data . 20
4.2.10 Households with Internet access . 20
4.3 Brazil . 20
4.3.1 National health system . 20
4.3.2 Focus of national health system . 20
4.3.3 Components of the national health information system . 22
4.3.4 National eHealth policies . 23
4.3.5 National eHealth architecture stage of development . 24
4.3.6 National data warehouse . 24
4.3.7 Standards in use . 25
4.3.8 Standards Development Organizations (SDOs) and Health Informatics Associations . 25
4.3.9 National reporting infrastructure for individual and/or summary data . 26
4.3.10 Households with Internet access . 26
4.4 Canada . 27
4.4.1 National health system . 27
4.4.2 Focus of national health system . 29
4.4.3 Components of the national health information system . 30
4.4.4 National eHealth policies . 31
4.4.5 National eHealth architecture stage of development . 32
4.4.6 National data warehouse . 34
4.4.7 Standards in use . 34
4.4.8 Standards Development Organizations (SDOs) and Health Informatics Associations . 34
4.4.9 National reporting infrastructure for individual and/or summary data . 35
4.4.10 Households with Internet access . 35
4.5 India . 35
4.5.1 National health system . 35
4.5.2 Focus of national health system . 36
4.5.3 Components of the national health information system . 37
4.5.4 National eHealth policies . 37
4.5.5 National eHealth architecture stage of development . 37
4.5.6 National data warehouse and national reporting infrastructure for individual and/or
summary data . 37
4.5.7 Standards in use . 37
4.5.8 Standards Development Organizations (SDOs) and Health Informatics Associations . 38
4.5.9 Households with Internet access .38
4.6 Kenya .38
4.6.1 National health system; focus of national health system .38
4.6.2 Components of the national health information system .39
4.6.3 National eHealth policies .42
4.6.4 National eHealth architecture stage of development .43
4.6.5 Standards in use .43
4.6.6 Standards Development Organizations (SDO) and Health Informatics Associations .44
4.6.7 National reporting infrastructure for individual and/or summary data .44
4.6.8 Households with Internet access .44
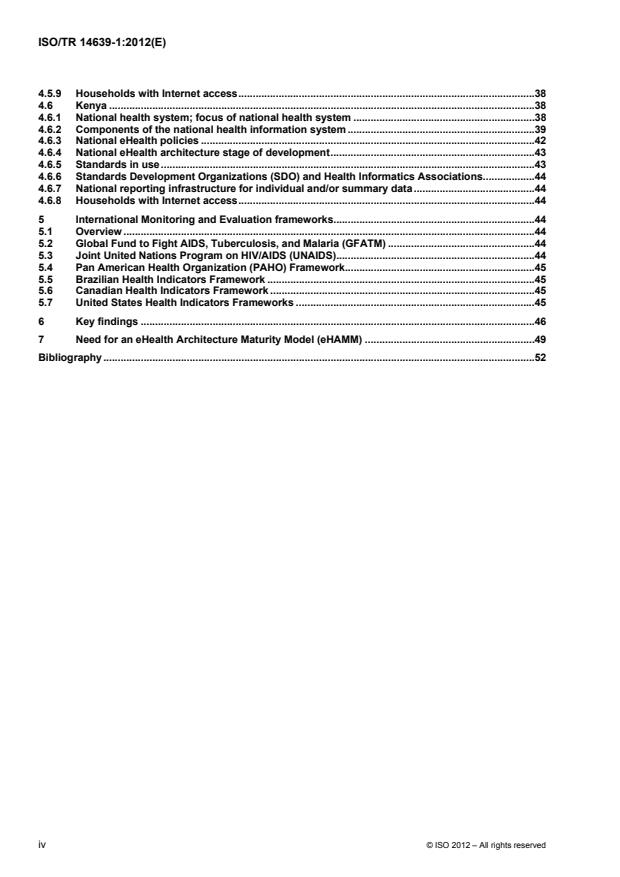
5 International Monitoring and Evaluation frameworks .44
5.1 Overview .44
5.2 Global Fund to Fight AIDS, Tuberculosis, and Malaria (GFATM) .44
5.3 Joint United Nations Program on HIV/AIDS (UNAIDS) .44
5.4 Pan American Health Organization (PAHO) Framework.45
5.5 Brazilian Health Indicators Framework .45
5.6 Canadian Health Indicators Framework .45
5.7 United States Health Indicators Frameworks .45
6 Key findings .46
7 Need for an eHealth Architecture Maturity Model (eHAMM) .49
Bibliography .52
iv © ISO 2012 – All rights reserved
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards bodies
(ISO member bodies). The work of preparing International Standards is normally carried out through ISO
technical committees. Each member body interested in a subject for which a technical committee has been
established has the right to be represented on that committee. International organizations, governmental and
non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely with the
International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
International Standards are drafted in accordance with the rules given in the ISO/IEC Directives, Part 2.
The main task of technical committees is to prepare International Standards. Draft International Standards
adopted by the technical committees are circulated to the member bodies for voting. Publication as an
International Standard requires approval by at least 75 % of the member bodies casting a vote.
In exceptional circumstances, when a technical committee has collected data of a different kind from that
which is normally published as an International Standard (“state of the art”, for example), it may decide by a
simple majority vote of its participating members to publish a Technical Report. A Technical Report is entirely
informative in nature and does not have to be reviewed until the data it provides are considered to be no
longer valid or useful.
Attention is drawn to the possibility that some of the elements of this document may be the subject of patent
rights. ISO shall not be held responsible for identifying any or all such patent rights.
ISO/TR 14639-1 was prepared by Technical Committee ISO/TC 215, Health informatics.
ISO/TR 14639 consists of the following parts, under the general title Health informatics — Capacity-based
eHealth architecture roadmap:
Part 1: Overview of national eHealth initiatives
The following parts are under preparation:
Part 2: Architectural components and maturity model
This part of ISO/TR 14639 complements and supports the general requirements for the use of information in
health services which are to be set out in the proposed technical specification, ISO/TS 16555, Health
informatics — Framework for national health information systems. ISO/TS 16555 will provide specifications
defining data sources and business processes supporting the more general use of information within the
delivery, operation, management and planning of health services within a country.
Introduction
This part of ISO/TR 14639 arises from the recognition that currently there is considerable diversity
internationally in the approach and scope of development and implementation of national health information
systems (HIS). Growing interest in health system strengthening in low-income countries (LIC) in the
[3]
international community has led to increasing interest in and support of this activity .
In preparing this part of ISO/TR 14639, the original aim was to provide guidance for developing and emerging
countries and for the many international groups that conduct health programs in the developing and emerging
world. As the work proceeded, it became clear that the work is more widely applicable to all health services,
for whom there are potential lessons to be learned as they examine the way in which information is used,
produced and managed in various aspects of their work. The identification of relevant health informatics
standards and the role of international standardization in support of eHealth were also important drivers.
This part of ISO/TR 14639 builds on lessons from many countries, including those whose activities are
summarized in this part of ISO/TR 14639, and was largely inspired by the Health Metrics Network (HMN)
[1][2]
activities sponsored by the World Health Organization (WHO) .
This work has been motivated in part by a recognition that countries vary in terms of readiness and resources
for health system strengthening, with the expectation that it will help to provide the tools needed for policy-
making, strategic planning and eHealth architecture development for robust and appropriate country HIS.
The particular focus of this part of ISO/TR 14639 is the potential for Information and Communications
Technology (ICT) to assist in the collection, communication, storage, processing and use of information to
support the delivery, planning and coordination of health services. However, it also recognizes the importance
of initial measures that involve paper-based collection and the need for a migration path from manual to semi-
automated to fully automated information management systems.
This part of ISO/TR 14639 presents a description of contemporary national enterprise-wide HIS. The resulting
landscape identifies key high-level categories for different aspects of such systems which should be
considered in any national architecture design endeavour. While not an exhaustive inventory of systems or
necessarily a description of best practices, it is roughly representative of all income levels and strives to
illustrate the diversity of HIS in different information technology environments with varying levels of capacity.
Supported by the findings from this review, this part of ISO/TR 14639 also proposes development of an
eHealth architecture maturity model (eHAMM) for expressing the extent of development of HIS and eHealth
architecture. The model can be used to direct planning and assess progress of national HIS towards maturity.
The maturity model will be elaborated upon in ISO/TR 14639-2 and includes a methodology for classifying HIS
according to descriptions of architectural components.
vi © ISO 2012 – All rights reserved
TECHNICAL REPORT ISO/TR 14639-1:2012(E)
Health informatics — Capacity-based eHealth architecture
roadmap —
Part 1:
Overview of national eHealth initiatives
1 Scope
This part of ISO/TR 14639 aims to identify the business requirements of an eHealth architecture as well as
providing a generic and comprehensive context description to inform architectural structuring of Health
Information Systems (HIS).
This part of ISO/TR 14639 reviews international experiences in the construction of national eHealth
[4]
architectures and introduces a methodology for strategic development of HIS , which will be elaborated upon
in ISO/TR 14639-2.
This part of ISO/TR 14639 is intended to assist nations which are in the early or mid stages of developing
such systems.
2 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
2.1
architecture system
structure of components, their functions and their inter-relationships, and the principles and guidelines
governing their design and evolution over time, or a description of the structure and behaviour of a system, a
system’s components, its functions and inter-relationships
[14]
NOTE 1 Adapted from Open Group Architecture Framework (TOGAF), 2009 and Blobel, B., Application of the
[86]
Component Paradigm for Analysis and Design of Advanced Health System Architectures, 2000 .
NOTE 2 This term also includes architecture and system architecture.
2.2
biosurveillance
process of active data-gathering with appropriate analysis and interpretation of biosphere data that might
relate to disease activity and threats to human or animal health (whether infectious, toxic, metabolic, or
otherwise, and regardless or intentional or natural origin) in order to achieve early warning of health threats,
early detection of health events and overall situational awareness of disease activity
[88]
[CDC Concept Plan for the Implementation of the National Biosurveillance Strategy for Human Health ]
2.3
clinical information
information about a person, relevant to his or her health or healthcare
[ISO 13606-1:2008, definition 3.13]
2.4
chronic disease
health condition of 3 months' duration or longer
[US National Center for Health Statistics]
2.5
data warehouse
grouping of data accessible by a single data management system, possibly of diverse sources, pertaining to a
system or sub-system and enabling secondary data analysis for questions relevant to understanding the
functioning of that system, and hence supporting proper maintenance and improvement of that system
NOTE 1 A data warehouse tends not to be used in real time; however, depending on the rapidity of transfer of data to
the data warehouse, and data integrity, near real time applications are not excluded.
NOTE 2 Adapted from ISO/TR 22221:2006.
2.6
eHealth
the combined use of electronic communication and information technology in the health sector to enable
better health and healthcare
[World Health Organization]
2.7
eHealth architecture
structure of a system of eHealth components and services
2.8
electronic health record
EHR
information relevant to the wellness, health and healthcare of an individual, in computer-processable form and
represented according to a standardized information model, or the longitudinal electronic record of an
individual that contains or virtually interlines to data in multiple EMRs and EPRs, which is to be shared and/or
interoperable across healthcare settings and is patient-centric
NOTE Adapted from ISO 18308:2011 and the European 2011 eHealth Strategies Final Report, January 2011.
2.9
electronic medical record
EMR
electronic record of an individual in a physician’s office or clinic, which is typically in one setting and is
provider-centric
[European 2011 eHealth Strategies Final Report, January 2011]
2.10
electronic patient record
EPR
electronic record of an individual in a hospital or health care facility, which is typically in one organisation and
is facility-centric
[European 2011 eHealth Strategies Final Report, January 2011]
2.11
health
state of complete physical, mental and social well-being and not merely the absence of disease or infirmity
[World Health Organization 1948]
2 © ISO 2012 – All rights reserved
2.12
health condition
aspect of a person or group’s health that requires some form of intervention
NOTE These interventions could be anticipatory or prospective, such as enhancing wellness, wellness promotion or
illness prevention (e.g. immunization).
[Canada Health Infoway EHRS Blueprint v1.0: 2003]
2.13
health information
information about a person relevant to his or her health
[ISO 18308:2011, definition 3.28]
2.14
health information system
HIS
system that combines vital and health statistical data from multiple sources to derive information and make
decisions about the health needs, health resources, costs, uses, and outcomes of healthcare
NOTE Adapted from Canada Health Infoway, Canadian Electronic Drug Messaging (CeRx) Standards 1-2010/03/29.
2.15
health worker
person engaged in actions that are primarily intended to enhance health
NOTE 1 This term also includes healthcare worker.
NOTE 2 Adapted from World Health Report, January 01, 2006.
2.16
healthcare
activities, services or supplies related to the health of an individual
[EN 13940-1:2007]
2.17
healthcare activity
activity performed for a subject of care with the intention of directly or indirectly improving or maintaining the
health of that subject of care
[EN 13940-1:2007]
2.18
healthcare professional
person authorized to be involved in the direct provision of certain healthcare provider activities in a jurisdiction
according to a mechanism recognized in that jurisdiction
NOTE Adapted from EN 13940-1:2007.
2.19
healthcare provider
healthcare organization or healthcare professional involved in the direct provision of healthcare
[EN 13940-1:2007]
2.20
interoperability
see semantic interoperability (2.34) and syntactic interoperability (2.36)
2.21
low income country
LIC
country where income is USD 1 005 gross national income (GNI) per capita or less, calculated using the
World Bank Atlas method
NOTE 1 An LIC is part of the classification system of all World Bank member countries (187), and all other economies
with populations of more than 30,000 (213 total). Economies are divided according to 2009 GNI per capita, calculated
using the World Bank Atlas method. The groups are: low income, $995 or less; lower middle income, $996 - $3,945; upper
middle income, $3,946 - $12,195; and high income, $12,196 or more.
NOTE 2 Adapted from World Bank Country Classifications.
2.22
monitoring and evaluation
M & E
routine tracking of the key elements of programme/project performance, usually inputs and outputs, through
record-keeping, regular reporting and surveillance systems, as well as health facility observation and client
surveys, and the episodic assessment of the change in targeted results that can be attributed to the
programme or project/project intervention
NOTE Evaluation attempts to link a particular output or outcome directly to an intervention after a period of time has
passed.
[Global Fund]
2.23
notifiable diseases
list of diseases determined by the International Health Regulations used as a decision instrument for the
assessment and notification of events that may constitute a public health emergency of international concern
[World Health Organization, International Health Regulations]
2.24
organization
unique framework of authority within which a person or persons act, or are designated to act, towards some
purpose
NOTE Adapted from ISO/IEC 6523-1:1998, definition 3.1.
2.25
patient
individual who is a subject of care
NOTE Adapted from ISO/TR 20514:2005, definition 2.30.
2.26
personal health information
any information that concerns a person's health, health history, health treatment or genetic characteristics in a
form that enables the person to be identified
NOTE Adapted from ISO/TR 18307:2001, definition 3.112.
2.27
policy
set of rules such as legal, political or organizational which can be expressed as obligations, permissions or
prohibitions
NOTE Adapted from ISO/TS 22600-1:2006, definition 2.13.
4 © ISO 2012 – All rights reserved
2.28
primary care
first level of care (access to first contact), characterized mainly by longitudinality, comprehensive care and
coordination of care within the health system itself
NOTE It may have additional features such as family counselling and community and cultural competence.
[Starfield, B., Primary care: concept, evaluation and policy. New York, Oxford University Press, 1992]
2.29
privacy
freedom from intrusion into the private life or affairs of an individual when that intrusion results from undue or
illegal gathering and use of data about that individual
[ISO/IEC 2382-8:1998, definition 08.01.23]
2.30
register
formal or official recording of items, names or actions
[ISO/IEC 10036:1996, definition 3.3]
2.31
registry
server capable of holding data for the systematic and continuous follow-up of information objects maintained
in accordance with specific rules
[ISO/TR 21089:2004, definition 3.79]
2.32
roadmap
detailed plan to guide progress towards a goal
[Merriam-Webster Dictionary]
2.33
secure messaging
set of means for cryptographic protection of [parts of] command-response pairs
[ISO/IEC 7816-4:2005, definition 3.39]
2.34
semantic interoperability
ability for data shared by systems to be understood at the level of fully defined domain concepts
[ISO/TS 18308:2011, definition 3.45]
2.35
subject of care
person seeking to receive, receiving, or having received healthcare
[EN 13940-1:2007]
2.36
syntactic interoperability
capability of two or more systems to communicate and exchange data through specified data formats and
communication protocols
[ISO 18308:2011, definition 3.48]
2.37
teleconsultation
provision of healthcare via a telehealth service, generally for the purpose of diagnosis or treatment of a
subject of care at a site remote from the patient or their primary care provider
NOTE Adapted from the Medical Conditions Dictionary.
2.38
telehealth
the use of telecommunication techniques for the purpose of providing telemedicine, medical education and
health education over distance
[ISO/TS 16058:2004, definition 3.13]
2.39
vocabulary
terminological dictionary which contains designations and definitions from one or more specific subject fields
NOTE Adapted from ISO 1087-1:2000, definition 3.7.2.
3 Abbreviations
AIDS Acquired Immunodeficiency Syndrome
CDA Clinical Document Architecture
eHAMM eHealth architecture maturity model
EHR Electronic Health Record
EMR Electronic Medical Record
HIC Health Information Custodian
HIS Health Information System
HIV Human Immunodeficiency Virus
HL7 Health Level Seven
ICD International Statistical Classification of Diseases and Related Health Problems
ICT Information and Communications Technology
IHE Integrating the Healthcare Enterprise
IHTSDO International Health Terminology Standards Development Organization
ISO International Organization for Standardization
ISO/TC 215 ISO Technical Committee 215 (Health Informatics)
IT Information Technology
LIC Low Income Country
M & E Monitoring & Evaluation
6 © ISO 2012 – All rights reserved
MoH Ministry of Health
NGO Non-governmental organization
PHR Personal Health Record
SNOMED CT Systematized Nomenclature of Medicine Clinical Terms
TB Tuberculosis
4 Initiatives reviewed
4.1 Health Metrics Network
[1][2]
The Health Metrics Network (HMN), under the auspices of the World Health Organization (WHO) , is the
first global health partnership that focuses on two core requirements necessary to strengthen the health
system that delivers care and services in countries. It focuses on the need to enhance entire health
information and statistical systems, rather than focusing only upon specific diseases. It also concentrates
country efforts on strengthening country leadership for health information production and use. This Framework
has been devised to coordinate and align partners to focus investments and technical assistance on
standardizing health information system development.
The HMN Framework is expected to permit access to and better use of improved health information at country
and global levels. The 2007 60th World Health Assembly and its nearly 200 member states passed Resolution
60.27 in which it urged stakeholders ranging from international bodies, the public and private sectors and
health information and statistical communities to use the standardized norms and guiding principles of the
HMN Framework in the strengthening of health information systems. All of these constituencies are expected
to directly benefit from the use of the Framework by countries. To date, over 80 countries in all six continents
have commenced using the Framework.
Formal vetting and publishing by ISO would help make this framework a keystone in strengthening these
country health information systems. In the fall of 2010, the HMN brought a new work item (NWI) to ISO/TC
215 which passed balloting and is moving forward to become an ISO standard: ISO TS 16555 Health
informatics - Framework for national health information systems. The aspects of standardization to be covered
in the NWI include the preservation of the framework as a whole and delineation of the specifications of the
framework into standardized formats. A timely follow-on work item to produce these formats could serve as a
powerful catalyst to maintain the global momentum of enterprise architects and designers and users around
this work, and crystallize global consensus. As the NWI specifications will be technology-neutral, present and
future forms of technology will remain equally relevant. The urgency of the NWI is further exemplified by the
growing global movement around the use of mobile technology (m-health) as a driver of country health
information systems. It is necessary for this work to include the mHealth activities given their expected impact.
The framework will also be updated to include other emerging topics such as human resources (HR), for
example that may not be represented in the current landscaping.
4.2 Australia
4.2.1 National health system
Australia has a federal system of government with the Australian Government operating at the national level
alongside six state governments and two territory governments. The Australian Government collects most of
the tax revenue and distributes a proportion of it back to the states and territories, which have constitutional
responsibility for delivering a range of health and welfare services within their jurisdictions - including acute-
care public hospitals, mental health, public health and some community-based social care and preventative
programs.
Most primary care and many specialist medical and allied health services are delivered by independent private
practitioners on a fee-for-service basis. A significant proportion of the cost to consumers of medical and some
allied health services is covered by a universal health insurance program operated by the Australian
Government (Medicare).
There are also networks of Aboriginal Medical Services and Aboriginal-Controlled Community Health Services
serving indigenous (Aboriginal and Torres Strait Islander) communities. These are mainly funded by the
Australian Government but managed through the states and territories.
Although there is no single national authority with responsibility for delivery of healthcare services across the
country, the Australian Government uses its powers over health insurance, reimbursement of private
practitioners (Medical Benefits Scheme), payment for prescription medications (Pharmaceutical Benefits
Scheme), aged care, indigenous health, veterans care, special-purpose programs and particularly the funding
it contributes to the states and territories under the Medicare Agreement, to maintain a reasonably uniform
healthcare regime across the country.
Under this regime, all Australians (including non-citizen residents) are entitled to free care in public hospitals
and public contributions toward the cost of care received from private practitioners and the amount they pay
for prescription drugs - with an additional safety net that limits the cost for those on low incomes and those
facing higher healthcare costs.
In March 2010, the Australian Government released a report entitled "A national health and hospitals network
[5]
for Australia’s future" (NHHN) which, among other things, proposed more direct involvement of the
Australian Government in the funding of healthcare and hospitals and a reduced role for the states and
territories in management of these services. While most Australians favour some level of reform to get more
efficient and better integrated management of healthcare delivery, the proposed NHHN reforms faced
significant constitutional, political and financial barriers.
Under the Australian federal system, the leaders of the Australian, State and Territory Governments regularly
meet at the Council of Australian Government (COAG) to debate and, where possible, agree on common
policy positions. Within the health sector, collaborative programs are also progressed through the Australian
Health Ministers Council (AHMC) which is advised by AHMAC (the Australian Health Ministers Advisory
Committee, made up of relevant heads of agencies responsible for health in each of the Australian, state and
territory jurisdictions).
At the COAG meeting in May 2010 most, but not all, states/territories accepted the proposed NHHN reforms in
principle but full agreement on the details could not be finalised before a series of elections changed the
political landscape.
At a further COAG meeting in February 2011, some elements of the reform package were dropped in favour
of a further heads of agreement [6] that provides the framework for a revised National Health Reform
Agreement for execution in 2011. The heads of agreement reaffirms the state/territory role as managers of
public hospital and public health systems within their jurisdictions but with increased funding and oversight
from the Australian Government and better coordination of primary care service delivery.
Central to the reforms being proposed under the new National Health Reform Agreement are: a new national
hospital funding authority, which will allocate funds directly to local hospital networks from a single
consolidated pool of federal and state/territory funds, an Independent Hospital Pricing Authority (IHPA), a
Health Performance Authority (HPA) and a permanent, increased role for the Australian Commission on
Safety and Quality in Healthcare, which develops, monitors and implements national standards for improving
clinical safety and quality to improve patient outcomes.
Australia also has a well-developed private hospital and aged care sector, which is an integral part of the
national healthcare regime. There are tax incentives to encourage Australians to take out private health
insurance which provides cover for private hospital and ambulance costs and, optionally, dental, optical and
some other allied health services. Private practitioners are free to set their own fees and privately insured
patients may choose to be treated by an approved private practitioner in a public hospital (in which case the
public hospital also charges an accommodation fee set by each state/territory).
While Australians may insure against hospital costs, they must meet any additional amounts (gaps) charged
by private practitioners above the public rebate out of their own pockets and are not allowed to insure for
8 © ISO 2012 – All rights reserved
these gaps. This measure is aimed at ensuring that there is some price competition moderating the fees
charged for clinical services.
In summary, Australia has a national health funding regime (with healthcare costs shared between the
Australian Government, state/territory governments, private insurance and the health consumer) but not a
unified national healthcare delivery program. Health has recently become a major political issue with
significant changes in responsibilities and greater central control having been proposed but it is too early to
predict the outcomes.
4.2.2 Focus of national health system
The national healthcare funding regime is generally broad in coverage; however, there is less public funding
available for dentistry and some allied health areas, but this is under discussion.
In terms of healthcare service delivery, Australia has high levels of public health, disease control and life
expectancy with world-class clinical care facilities distributed across the country and readily available to much
of the population; however, the ageing of both the population and the clinical workforce and the associated
rising costs of health as a proportion of GDP (9,0 % in 2008-09) are putting traditional modes of care delivery
under pressure. In particular:
1. Chronic Disease. A significant and rapidly growing proportion of healthcare costs in Australia are driven by
chronic disease, particularly later in a person's life. The Australian, state and territory governments all
have programs aimed at improving the treatment and management of chronic disease, reducing its
burden on patients and its cost to society, with a particular focus on:
arthritis and musculoskeletal conditions
asthma, chronic obstructive pulmonary disorder (COPD) and other respiratory diseases
cancer control – through research, early detection and prevention and continual improvement and
targeting of treatment regimes
cardiovascular health – through research, monitoring, reducing risk factors and improved treatment.
Cardiovascular disease is the leading cause of death accounting for over one-sixth of all deaths in
both males and females[7].
diabetes mellitus – and the many co-morbidities that flow from it
injury prevention and control
mental health, and
reducing common risk factors – smoking, alcohol, substance abuse, obesity, diet, inactivity,
hypertension
2. Indigenous health. Indigenous Australians have significantly lower life expectancy and health outcomes
compared with the rest of the Australian population. This is a matter of long-standing national concern
across all jurisdictions. Some years ago, the Australian Government took a strong lead in seeking to
address the problem but there are many issues and interacting social factors that need to be managed
before it is likely to be solved.
3. Rural and regional healthcare. Australia is a very big country with most of its population concentrated
along a narrow strip along the southern and eastern seaboards and a couple of other major centres. As in
many countries, there has been a drift away from rural areas to the big cities. Clinical practices and health
services in many small rural towns are no longer economically viable or able to provide or access the
range of services now expected for modern care delivery. It is also difficult to attract and hold clinical staff
in these areas. Programs aimed at addressing these problems include greater use of Information and
Communications Technologies (ICT) to support both practitioners and patients in remote areas by
leveraging policies aimed at getting effective broadband services to 98% of the Australian population.
4. Clinical workforce. The clinical workforce is ageing with the population and is under ever increasing
workload. For many years, much of the shortfall has been made up by use of overseas-trained clinical
personnel in both a temporary and permanent capacity; however, this is an issue that Australia is
addressing in several ways including:
Greatly increasing the number of clinical training positions – not only in medicine, but also in
clinical nursing and allied health professions
Moving to shorter, postgraduate clinical training programs more strongly focused on clinical
practice
Developing new models of team-based care, in which clinical nurse specialists, physician
assistants, pharmacists and other clinical support personnel take on a wider range of
responsibilities and there is greater collaboration between medical specialties in care delivery. To
be effective these new models of care anticipate improved sharing of clinical information.
The NHHN health reforms put forward by the Australian Government in 2010 seek to address the above
needs by a targeted program of activities in the following areas (see [8] for more details):
Governance and funding of healthcare National standards and performance
Hospitals Workforce
GP and primary healthcare Prevention
Aged care eHealth
Mental health Stakeholder engagement
In 2010/11, for the first time, the Australian Government budget separately recognised eHealth as an enabler
of health reform and allocated significant project funding to eHealth as part of its commitment to the overall
NHHN reform package.
4.2.3 Components of the national health information system
There are nationally agreed and widely adopted specifications for classification of clinical information and
statistical reporting of healthcare status and activities. These are applied at the level of individual healthcare
facilities, state/territory and on an Australia-wide basis and are used to support statistical reporting,
performance evaluation, health service planning and activity based funding - predominantly for institutional
care. Under the proposed National Health Reform Agreement, most public hospital reimbursement is planned
to be based on activity.
National health and welfare statistics are compiled in accordance with agreed national standards through the
Australian Institute of Health and Welfare (AIHW) based on information sourced from the state and territory
health authorities. These statistics include activities carried out in both public and private sectors. [For more
information, see: http://www.aihw.gov.au/].
While the national health and welfare statistics contain comprehensive information on hospital activity, long-
term care and some community care, there is much less information available on the h
...
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...