ISO/TS 21547:2010
(Main)Health informatics — Security requirements for archiving of electronic health records — Principles
Health informatics — Security requirements for archiving of electronic health records — Principles
The purpose of ISO/TS 21547:2010 is to define the basic principles needed to securely preserve health records in any format for the long term. It concentrates on previously documented healthcare specific archiving problems. It also gives a brief introduction to the general archiving principles. Unlike the traditional approach to standardization work, where the perspective is that of modelling, code sets and messages, this Technical Specification looks at archiving from the angle of document management and related privacy protection. In ISO/TS 21547:2010 archiving is understood to be a wider process than just the permanent preservation of selected records. ISO/TS 21547:2010 defines architecture and technology-independent security requirements for long-term preservation of EHRs having fixed content. ISO/TS 21547:2010 and a complementary Technical Report, ISO 21548, concentrate on the security requirements (integrity, confidentiality, availability and accountability) necessary for ensuring adequate protection of health information in long-term digital preservation. This Technical Specification will also address privacy protection requirements for both the EHR and eArchiving systems used in the healthcare environment. ISO/TS 21547:2010 defines functional security requirements for long term archiving of EHRs, but the practical archiving models and technology required are outside the concept of this Technical Specification.
Informatique de santé — Exigences de sécurité pour l'archivage des dossiers de santé électroniques — Principes
General Information
- Status
- Published
- Publication Date
- 01-Feb-2010
- Technical Committee
- ISO/TC 215 - Health informatics
- Drafting Committee
- ISO/TC 215/WG 4 - Security, Safety and Privacy
- Current Stage
- 9599 - Withdrawal of International Standard
- Start Date
- 18-Dec-2025
- Completion Date
- 12-Feb-2026
Overview
ISO/TS 21547:2010 - Health informatics - Security requirements for archiving of electronic health records - Principles - defines the fundamental principles for securely preserving electronic health records (EHRs) over the long term. The Technical Specification focuses on healthcare‑specific archiving challenges and presents architecture‑ and technology‑independent security requirements for EHR‑archives (eArchiving). It treats archiving as a holistic process - not only permanent preservation but records maintenance, retention, disclosure and eventual destruction - and emphasizes document management and privacy protection in the healthcare context.
Key topics and technical requirements
ISO/TS 21547:2010 concentrates on high‑level, functional security requirements rather than specific technologies. Core topics include:
- Security objectives: integrity, confidentiality, availability and accountability (non‑repudiation) for long‑term EHR preservation.
- Privacy protection: requirements for protecting patient privacy in both EHR content and eArchiving systems, including access/disclosure controls and auditability.
- EHR‑archive concepts: definitions of EHR, EHR‑archive, backup versus archive, elements and types of archives (centralized, federated, online storage).
- eArchiving process: roles, responsibilities, policies, and lifecycle activities (submission to archive, maintenance, access, migration and disposal).
- Legal and regulatory alignment: requirements derived from legislation and national frameworks are considered; the specification highlights the need to meet jurisdictional obligations.
- Architecture independence: security requirements are specified independent of implementation models and technologies (no prescriptive formats or systems).
Practical applications
ISO/TS 21547:2010 is used to:
- Define security and privacy requirements for long‑term EHR archiving projects.
- Guide design of eArchiving policies, responsibilities and audit frameworks.
- Inform procurement specifications for EHR‑archive solutions and third‑party archival services.
- Support compliance assessments and risk analyses for health information preservation.
Typical use cases include national/regional EHR archives, hospital record retention programs, clinical document repositories and cross‑organizational exchange where long‑term trust and legal evidentiary value are required.
Who should use this standard
- Healthcare IT architects and system designers
- Records managers and clinical archivists
- Security, privacy and compliance officers in health organizations
- EHR vendors and cloud archival service providers
- Policymakers and implementers of national eHealth programs
Related standards
- ISO 14721 (OAIS reference model) - digital preservation concepts
- ISO 15489 (records management) - recordkeeping practices
- ISO 19005‑1 (PDF/A) - preservation file format
- ISO/TR 21548 - complementary technical report to ISO/TS 21547
- National frameworks (annexes cover examples from Finland, UK, Japan, USA/HIPAA)
Keywords: ISO/TS 21547:2010, electronic health records, EHR‑archive, eArchiving, long‑term preservation, security requirements, integrity, confidentiality, availability, accountability, privacy protection.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

NYCE
Mexican standards and certification body.
Sponsored listings
Frequently Asked Questions
ISO/TS 21547:2010 is a technical specification published by the International Organization for Standardization (ISO). Its full title is "Health informatics — Security requirements for archiving of electronic health records — Principles". This standard covers: The purpose of ISO/TS 21547:2010 is to define the basic principles needed to securely preserve health records in any format for the long term. It concentrates on previously documented healthcare specific archiving problems. It also gives a brief introduction to the general archiving principles. Unlike the traditional approach to standardization work, where the perspective is that of modelling, code sets and messages, this Technical Specification looks at archiving from the angle of document management and related privacy protection. In ISO/TS 21547:2010 archiving is understood to be a wider process than just the permanent preservation of selected records. ISO/TS 21547:2010 defines architecture and technology-independent security requirements for long-term preservation of EHRs having fixed content. ISO/TS 21547:2010 and a complementary Technical Report, ISO 21548, concentrate on the security requirements (integrity, confidentiality, availability and accountability) necessary for ensuring adequate protection of health information in long-term digital preservation. This Technical Specification will also address privacy protection requirements for both the EHR and eArchiving systems used in the healthcare environment. ISO/TS 21547:2010 defines functional security requirements for long term archiving of EHRs, but the practical archiving models and technology required are outside the concept of this Technical Specification.
The purpose of ISO/TS 21547:2010 is to define the basic principles needed to securely preserve health records in any format for the long term. It concentrates on previously documented healthcare specific archiving problems. It also gives a brief introduction to the general archiving principles. Unlike the traditional approach to standardization work, where the perspective is that of modelling, code sets and messages, this Technical Specification looks at archiving from the angle of document management and related privacy protection. In ISO/TS 21547:2010 archiving is understood to be a wider process than just the permanent preservation of selected records. ISO/TS 21547:2010 defines architecture and technology-independent security requirements for long-term preservation of EHRs having fixed content. ISO/TS 21547:2010 and a complementary Technical Report, ISO 21548, concentrate on the security requirements (integrity, confidentiality, availability and accountability) necessary for ensuring adequate protection of health information in long-term digital preservation. This Technical Specification will also address privacy protection requirements for both the EHR and eArchiving systems used in the healthcare environment. ISO/TS 21547:2010 defines functional security requirements for long term archiving of EHRs, but the practical archiving models and technology required are outside the concept of this Technical Specification.
ISO/TS 21547:2010 is classified under the following ICS (International Classification for Standards) categories: 35.240.80 - IT applications in health care technology. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO/TS 21547:2010 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
TECHNICAL ISO/TS
SPECIFICATION 21547
First edition
2010-02-15
Health informatics — Security
requirements for archiving of electronic
health records — Principles
Informatique de santé — Exigences de sécurité pour l'archivage des
dossiers de santé électroniques — Principes
Reference number
©
ISO 2010
PDF disclaimer
This PDF file may contain embedded typefaces. In accordance with Adobe's licensing policy, this file may be printed or viewed but
shall not be edited unless the typefaces which are embedded are licensed to and installed on the computer performing the editing. In
downloading this file, parties accept therein the responsibility of not infringing Adobe's licensing policy. The ISO Central Secretariat
accepts no liability in this area.
Adobe is a trademark of Adobe Systems Incorporated.
Details of the software products used to create this PDF file can be found in the General Info relative to the file; the PDF-creation
parameters were optimized for printing. Every care has been taken to ensure that the file is suitable for use by ISO member bodies. In
the unlikely event that a problem relating to it is found, please inform the Central Secretariat at the address given below.
© ISO 2010
All rights reserved. Unless otherwise specified, no part of this publication may be reproduced or utilized in any form or by any means,
electronic or mechanical, including photocopying and microfilm, without permission in writing from either ISO at the address below or
ISO's member body in the country of the requester.
ISO copyright office
Case postale 56 • CH-1211 Geneva 20
Tel. + 41 22 749 01 11
Fax + 41 22 749 09 47
E-mail copyright@iso.org
Web www.iso.org
Published in Switzerland
ii © ISO 2010 – All rights reserved
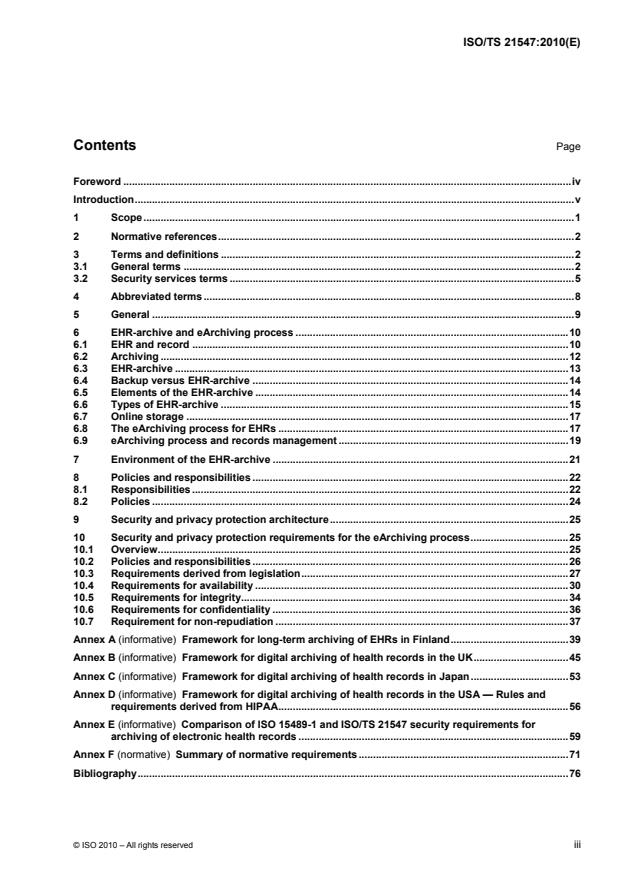
Contents Page
Foreword .iv
Introduction.v
1 Scope.1
2 Normative references.2
3 Terms and definitions .2
3.1 General terms .2
3.2 Security services terms .5
4 Abbreviated terms .8
5 General .9
6 EHR-archive and eArchiving process .10
6.1 EHR and record .10
6.2 Archiving .12
6.3 EHR-archive .13
6.4 Backup versus EHR-archive .14
6.5 Elements of the EHR-archive .14
6.6 Types of EHR-archive .15
6.7 Online storage .17
6.8 The eArchiving process for EHRs .17
6.9 eArchiving process and records management .19
7 Environment of the EHR-archive .21
8 Policies and responsibilities .22
8.1 Responsibilities .22
8.2 Policies .24
9 Security and privacy protection architecture.25
10 Security and privacy protection requirements for the eArchiving process.25
10.1 Overview.25
10.2 Policies and responsibilities .26
10.3 Requirements derived from legislation.27
10.4 Requirements for availability .30
10.5 Requirements for integrity.34
10.6 Requirements for confidentiality .36
10.7 Requirement for non-repudiation .37
Annex A (informative) Framework for long-term archiving of EHRs in Finland.39
Annex B (informative) Framework for digital archiving of health records in the UK.45
Annex C (informative) Framework for digital archiving of health records in Japan.53
Annex D (informative) Framework for digital archiving of health records in the USA — Rules and
requirements derived from HIPAA.56
Annex E (informative) Comparison of ISO 15489-1 and ISO/TS 21547 security requirements for
archiving of electronic health records .59
Annex F (normative) Summary of normative requirements .71
Bibliography.76
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards bodies
(ISO member bodies). The work of preparing International Standards is normally carried out through ISO
technical committees. Each member body interested in a subject for which a technical committee has been
established has the right to be represented on that committee. International organizations, governmental and
non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely with the
International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
International Standards are drafted in accordance with the rules given in the ISO/IEC Directives, Part 2.
The main task of technical committees is to prepare International Standards. Draft International Standards
adopted by the technical committees are circulated to the member bodies for voting. Publication as an
International Standard requires approval by at least 75 % of the member bodies casting a vote.
In other circumstances, particularly when there is an urgent market requirement for such documents, a
technical committee may decide to publish other types of document:
⎯ an ISO Publicly Available Specification (ISO/PAS) represents an agreement between technical experts in
an ISO working group and is accepted for publication if it is approved by more than 50 % of the members
of the parent committee casting a vote;
⎯ an ISO Technical Specification (ISO/TS) represents an agreement between the members of a technical
committee and is accepted for publication if it is approved by 2/3 of the members of the committee casting
a vote.
An ISO/PAS or ISO/TS is reviewed after three years in order to decide whether it will be confirmed for a
further three years, revised to become an International Standard, or withdrawn. If the ISO/PAS or ISO/TS is
confirmed, it is reviewed again after a further three years, at which time it must either be transformed into an
International Standard or be withdrawn.
Attention is drawn to the possibility that some of the elements of this document may be the subject of patent
rights. ISO shall not be held responsible for identifying any or all such patent rights.
ISO/TS 21547 was prepared by Technical Committee ISO/TC 215, Health informatics.
iv © ISO 2010 – All rights reserved
Introduction
The healthcare industry is faced with the challenge of reducing costs by moving from paper-based processes
to automated electronic processes. New models of healthcare delivery emphasise the need for patient
information to be shared among a growing number of specialist healthcare providers and across traditional
organizational boundaries.
Paper-based patient records have traditionally been stored in archives which were once located near work
sites; however, it is now common that these documents are located in the organization's centralized archive.
Due to lack of space or to ensure safekeeping, paper data from archives have been transferred to microfilm.
When patient data are transferred to an electronic format, data are either maintained in a simple database or
on paper printouts in an archive. During the past few years, electronic archives independent of basic systems
have been created, such as DICOM – a standard archival system for medical images. An electronic archive
can become a shared information storage system, an archive containing different software and even different
organizations. Centralized administration provides opportunities for managing good data security and
utilization of archival information in accordance with the patient's requests.
Electronic data storage is threatened by the same basic hazards as paper storage. Data can disappear or the
ability to read and understand it can be lost. Electronic media such as magnetic tapes, diskettes and hard
disks can break, be destroyed or get lost. We only have a few decades of experience as to their durability.
Merely retaining the media does not guarantee that the data will be available. As computer hardware and
software are quickly upgraded, older, yet still-functioning media cannot be used with current readers or
software because they are no longer able to read the stored data. With the development of technology, we
must be prepared to transfer old data to new media whenever necessary. Data structures must also be
converted or else unstructured data must be used.
Issues of stability and integrity threaten the storage of electronic data more than paper-based data. The
unlawful usurping or copying of data must also be effectively prevented.
Electronic patient records must be available throughout their whole lifecycle. The need to access patient
records regardless of place and time has increased data transfer between service provider organizations and
healthcare professionals within the last few years. Particularly, data transfer involving different software has
greatly increased over the past few years. The objective to reinforce patient rights to self-determination and
participation in healthcare at its different stages invites the opportunity for the patient to gain more information
concerning his or her care.
An EHR-archive (web-based, regionally centralized or organization-specifically distributed) can manage the
aforementioned data usage and transfer needs in a cost-effective and information-secure way. The use of
health services across national borders is continuously increasing due to mobility of inhabitants,
internationalization of companies and virtualization of health services. In cases where the EHR-archive
discloses records over borderlines, it is necessary that the archive be trusted.
The healthcare environment is unique. Any information system planned for use in this domain should
understand healthcare-specific features such as:
⎯ specific ethical and legal environments;
⎯ in cases where personal health information is accessed, used or disclosed, privacy protection should be
taken into account;
⎯ strong regulations for who can access or disclose healthcare records, when and for what purpose;
⎯ in many countries, citizens/patients have the right to control the use or disclosure of their records using
opt-out and/or consent methods;
⎯ citizens/patients can have the right to know who has used their electronic health records (EHRs) and for
what purpose;
⎯ health service providers or service provider organizations have the responsibility for managing the
records;
⎯ EHRs have a very long preservation time;
⎯ EHR content is sensitive and has specific context and purpose;
⎯ EHR content can grow (e.g. be dynamic) during the preservation time;
⎯ specific responsibilities for EHR management or use;
⎯ the information content of the EHR has context, purpose and sensitivity based access and disclosure
rules;
⎯ the nature of the EHR or its parts can change during the preservation time;
⎯ EHR content should be understandable during the whole preservation time;
⎯ for confidentiality and legal purposes, it might be necessary to prove the non-repudiation of events
occurring during the preservation time of the EHR.
Not all of the above-mentioned features are unique for healthcare. Features described are common for most
countries in the world, but there are also variations depending on national regulatory and normative
environments. In any case, it is clear that healthcare forms a unique environment for records management
and archiving.
Digital archiving is not a healthcare-specific question. Digital libraries and many other organizations are
developing both the necessary technology and the requirements for digital archiving. However, based on the
unique nature of healthcare information, the following healthcare-specific questions remain to be solved:
a) health information has a very long preservation time (up to 100+ years);
b) the content (e.g. data objects/documents) of the EHR can be dynamic during its lifetime (e.g. the service
provider can add new fixed parts to the record before it is sent to the eArchive);
c) data content is sensitive;
d) a high degree of security, confidentiality and privacy protection is required;
e) there is a strong legal framework regulating who can access, what and when;
f) data objects have context, purpose and sensitivity based access/disclosure rules;
g) the nature of data can be legal for a given period;
h) non-repudiation of data and evidence should be secured during the whole preservation time.
Standards already exist for long-term preservation of digital documents. For example ISO 14721 defines a
reference model for open archival information systems (OAIS). The ISO 15489 series, clearly shows how any
organization can systematically and effectively improve their record-keeping. ISO 19005-1 defines a standard
file format for preservation.
vi © ISO 2010 – All rights reserved
Many countries have already developed frameworks or “codes of practice” for preservation of health records
(Annexes B to F). It is possible, based on already existing standards and national frameworks, to develop an
international standard and guidelines, setting requirements for the secure archiving of electronic health
records.
TECHNICAL SPECIFICATION ISO/TS 21547:2010(E)
Health informatics — Security requirements for archiving of
electronic health records — Principles
IMPORTANT — The electronic file of this document contains colours which are considered to be
useful for the correct understanding of the document. Users should therefore consider printing this
document using a colour printer.
1 Scope
The purpose of this Technical Specification is to define the basic principles needed to securely preserve
health records in any format for the long term. It concentrates on previously documented healthcare-specific
archiving problems. It also gives a brief introduction to general archiving principles. Unlike the traditional
approach to standardization work, where the perspective is that of modelling, code sets and messages, this
Technical Specification looks at archiving from the angle of document management and related privacy
protection. The document management angle has traditionally been used in connection with patient records in
paper form and it can also be applied to digitally stored documents. There are different architectural and
technical ways to develop and implement long-term preservation of electronic health records. Archiving can be
a function of the online record-keeping system, and we can have a separate independent archive or a
federated one. Electronic health records are, in many cases, archived in the form of documents, but other
technical solutions also exist.
In this Technical Specification archiving is understood to be a wider process than just the permanent
preservation of selected records. Archiving of EHRs is a holistic process covering records maintenance,
retention, disclosure and destruction when the record is not in active use. Archiving also includes tasks the
EHR system should perform before the record is sent to the EHR-archive.
This Technical Specification defines architecture and technology-independent security requirements for the
long-term preservation of EHRs having fixed content.
This Technical Specification and a complementary Technical Report, ISO/TR 21548, concentrate on the
security requirements (integrity, confidentiality, availability and accountability) necessary for ensuring
adequate protection of health information in long-term digital preservation. This Technical Specification will
also address privacy protection requirements for both the EHR and eArchiving systems used in the healthcare
environment.
This Technical Specification defines functional security requirements for long-term archiving of EHRs, but the
practical archiving models and technology required are outside the concept of this Technical Specification.
It is also outside of the Scope of this Technical Specification to comment on the following.
⎯ The creation, management and storage of active health records (records which can be modified, updated
and accessed any time at the level of a single object or item) inside the EHR-system. However this
Technical Specification defines responsibilities and tasks the EHR-system should undertake before it
transfers an EHR to the electronic archive.
⎯ The content of information submission packets sent to the EHR-archive. However this Technical
Specification defines security requirements for those packets.
⎯ Any storage structures used (such as DICOM, HL7 or XML) or metafile descriptions used (such as Dublin
core or HL7 CDA header) in the eArchiving process.
⎯ Implementation of security services such as PKI, electronic signatures, etc.
⎯ Any of the storage times of EHRs or media applicable for their storage; rather, these will continue to be
provided in accordance with national legislation.
2 Normative references
The following referenced documents are indispensable for the application of this document. For dated
references, only the edition cited applies. For undated references, the latest edition of the referenced
document (including any amendments) applies.
ISO/IEC 13888 (all parts), Information technology — Security techniques — Non-repudiation
ISO 14721, Space data and information transfer systems — Open archival information system — Reference
model
ISO 15489-1, Information and documentation — Records management — Part 1: General
ISO/TR 15489-2, Information and documentation — Records management — Part 2: Guidelines
ISO/IEC 17799, Information technology — Security techniques — Code of practice for information security
management
ISO/TS 18308, Health informatics — Requirements for an electronic health record architecture
ISO/TR 18492, Long-term preservation of electronic document-based information
ISO/TR 21548, Health informatics — Security requirements for archiving of electronic health records —
Guidelines
ISO/TS 22600-1, Health informatics — Privilege management and access control — Part 1: Overview and
policy management
ISO/TS 22600-2, Health informatics — Privilege management and access control — Part 2: Formal models
ISO 23081-1, Information and documentation — Records management processes — Metadata for records —
Part 1: Principles
ISO 27799, Health informatics — information security management in health using ISO/IEC 27002
EN 13606 (all parts), Health informatics — Electronic health record communication
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
3.1 General terms
3.1.1
application
any software process used in healthcare information systems, including those without any direct role in
treatment or diagnosis
NOTE In some jurisdictions, software processes can be regulated medical devices.
3.1.2
archive
organization that intends to preserve information for access and use for any designed users or process
NOTE Adapted from OAIS Red Book, June 12, 2001. Electronic archive (EHR-archive) preserves information in
digital format. It is an information system that manages and provides access to records through their whole lifecycle.
EHR-archive is an archive preserving digitalized health records.
2 © ISO 2010 – All rights reserved
3.1.3
archiving process
holistic long-term preservation process covering the whole lifecycle of the health record
3.1.4
administration
archival entity that contains the services and functions needed to control the operation of functional entities on
a day-to-day basis
3.1.5
content information
set of information that is the original target for preserving
3.1.6
data
re-interpretable representation of information in a formalized manner suitable for communication,
interpretation or processing
3.1.7
digital preservation
storage, maintenance, and access to a digital object over a long time, usually as a consequence of applying
one or more preservation strategies
1)
NOTE 1 Adapted from ELAG 2001.
NOTE 2 Preservation consists of processes and operations involved in ensuring the technical and intellectual survival
of authentic records through time (see ISO 15489-1).
3.1.8
directory
organizational unit or container, used to organize folders and files into a hierarchical structure
3.1.9
eArchiving process
holistic long-term preservation process covering the whole lifecycle of the electronic health record (EHR)
3.1.10
EHR
comprehensive, structured set of clinical, demographic, environmental, social and financial data and
information in electronic form, documenting the healthcare given to a single individual
NOTE Adapted from ASTM E1769.
3.1.11
EHR-archive
EHR-archive that preserves fixed EHRs for a long time
3.1.12
EHR-system
set of components that forms the mechanism from which patients, records are created, used, stored and
retrieved.
NOTE 1 It includes people, data, rules and procedures, processing and storage of data, and communication facilities.
NOTE 2 A narrow definition says that the EHR-system is a system for recording, retrieving, and manipulating
information in electronic healthcare records. See EN 13606.
1) European Library Automation Group.
3.1.13
fixity
permanent character or condition
NOTE Fixity information is that which documents mechanisms to ensure that the Content Information object has not
been altered in an undocumented manner. See ISO 14721.
3.1.14
healthcare organization
officially registered organization that has a main activity related to healthcare services or health promotion
NOTE 1 Examples include hospitals, internet healthcare website providers and healthcare research institutions.
NOTE 2 The organization should be recognised as legally liable for its activities but need not be registered for its
specific role in health. An internal part of an organization is called here an organizational unit as in X.501.
3.1.15
health professional
person who is authorized by a nationally recognised body, to be qualified to perform certain health services
NOTE 1 The types of registering or accrediting bodies differ by country and profession. Nationally recognised bodies
include local or regional governmental agencies, independent professional associations and other formally and nationally
recognised organizations. They can be exclusive or non-exclusive in their territory.
NOTE 2 A nationally recognised body in this definition does not imply one nationally controlled system of professional
registration but in order to facilitate international communication it would be preferable that one nationwide directory of
recognised health professional registration bodies exists.
EXAMPLE Physicians, registered nurses and pharmacists.
3.1.16
information
any type of knowledge that can be exchanged
3.1.17
long-term preservation
act of maintaining information in a correct and independently understandable form over a long time
3.1.18
metadata
data describing context, content and structure of records and their management through time
ISO 15489-1:2001, definition 3.12.
3.1.19
patient/consumer
person who is the receiver of health-related services and an actor in a health information system
3.1.20
privacy
freedom from intrusion into the private life or affairs of an individual when that intrusion results from undue or
illegal gathering and use of data about that individual
ISO/IEC 2382-8:1998, definition 08.01.23.
3.1.21
privacy protection
implementation of appropriate safeguards to ensure the security and confidentiality of data records, as well as
to protect the records against threats or hazards that could result in substantial embarrassment, harm,
inconvenience or unfairness to any person
4 © ISO 2010 – All rights reserved
3.1.22
privacy policy
privacy protection policy
document that states, in writing, principles of data protection used by an organization
NOTE It can be national as is the NHS Care Record Guarantee or local, made by an organization.
3.1.23
records management
field of management responsible for the efficient and systematic control of the creation, receipt, maintenance,
use and disposition of records
NOTE Adapted from the NHS Code of Practice.
3.1.24
record-keeping system
information system that captures, manages and provides access to records through time
NOTE 1 Adapted from the NHS Code of Practice.
NOTE 2 The EHR-system is a typical record-keeping system.
3.1.25
reference information
information that provides identifiers that allow an outside system to refer unambiguously to the particular
information
3.1.26
replication
digital duplication where there is no change to the information
3.1.27
structure information
information that imports knowledge about how other information is organized
3.2 Security services terms
3.2.1
access control
means of ensuring that the resources of a data processing system can be accessed only by authorized
entities in authorized ways
ISO/IEC 2382-8:1998, definition 08.04.01.
3.2.2
accountability
property that ensures that the actions of an entity may be traced uniquely to the entity
ISO 7498-2:1989, definition 3.3.3.
3.2.3
asymmetric cryptographic algorithm
algorithm for performing encipherment or the corresponding decipherment in which the keys used for
encipherment and decipherment differ
ISO/IEC 10181-1:1996, definition 3.3.1.
3.2.4
authenticity
quality of being authentic or of established authority for truth and correctness
NOTE An authentic record is one that can be proven to be what it purports to be, to have been created or sent by
persons purporting to have created or sent it and to have been created or sent at the time purported [Records
Management, NHS Code of Practice].
3.2.5
authentication
process of reliably identifying security subjects by securely associating an identifier and its authenticator
NOTE See also data origin authentication (3.2.11).
3.2.6
authorization
granting of rights, which includes the granting of access based on access rights
ISO 7498-2:1989, definition 3.3.10.
3.2.7
availability
property of being accessible and usable upon demand by an authorized entity
ISO 7498-2:1989, definition 3.3.11.
3.2.8
confidentiality
property that information is not made available or disclosed to unauthorized individuals, entities, or processes
ISO 7498-2:1989, definition 3.3.16.
3.2.9
cryptography
discipline which embodies principles, means and methods for the transformation of data in order to hide its
information content, prevent its undetected modification and/or prevent its unauthorized use
ISO 7498-2:1989, definition 3.3.20.
3.2.10
data integrity
property that data have not been altered or destroyed in an unauthorized manner
ISO 7498-2:1989, definition 3.3.21.
3.2.11
data origin authentication
corroboration that the source of data received is as claimed
ISO 7498-2:1989, definition 3.3.22.
3.2.12
decryption
process of obtaining, from a cipher text, the original corresponding data
ISO/IEC 2382-8:1998, definition 08-03-04.
6 © ISO 2010 – All rights reserved
3.2.13
digital signature
data appended to, or a cryptographic transformation [see cryptography (3.2.9)] of a data unit that allows a
recipient of the data unit to prove the source and integrity of the data unit and protect against forgery, e.g. by
the recipient
ISO 7498-2:1989, definition 3.3.26.
3.2.14
identity authentication
identity validation
performance of tests to enable a data processing system to recognise entities
ISO/IEC 2382-8:1998, definition 08.04.12.
3.2.15
identifier
piece of information used to claim an identity, before a potential corroboration by a corresponding
authenticator
ENV 13608-1:2000.
3.2.16
integrity
proof that the message content has not altered, deliberately or accidentally in any way, during transmission
3.2.17
key
sequence of symbols that controls the operations of encipherment and decipherment
ISO 7498-2:1989, definition 3.3.32.
3.2.18
key management
generation, storage, distribution, deletion, archiving and application of keys in accordance with a security
policy (3.2.22)
ISO 7498-2:1989, definition 3.3.33.
3.2.19
non-repudiation
service that provides proof of the integrity and origin of data (both in an unforgivable relationship) which can
be verified by any party
NOTE In a wider meaning, non-repudiation means there is unforgivable evidence that a specific action has occurred.
3.2.20
role
set of behaviours that is associated with a task
3.2.21
security
combination of availability, confidentiality, integrity and accountability
ENV 13608-1:2000.
3.2.22
security policy
plan or course of action adopted for providing computer security
ISO/IEC 2382-8:1998, definition 08.01.06.
EXAMPLE A set of laws, rules and practices that regulate how sensitive information is managed and distributed
within a specific system.
3.2.23
security service
service, provided by a layer of communicating open systems, which ensures adequate security of the systems
or of data transfers
ISO 7498-2:1989, definition 3.3.51.
3.2.24
information security
protection of information from (accidental or intentional) unauthorized access, use, disclosure, disruption,
modification or destruction
3.2.25
information security policy
document that states, in writing, how an organization plans to protect its physical and information technology
assets
3.2.26
security classification
category to which personal information and material is assigned to denote the degree of damage that
unauthorized disclosure would cause a person or his/her relations and to denote the degree of protection
required
4 Abbreviated terms
⎯ CDA Clinical documentation architecture
⎯ EHR Electronic health record
⎯ HL7 Health level 7
⎯ ISMS Information security management system
⎯ PKI Public key infrastructure
⎯ LAN Local area network
⎯ NHS National Health Service
⎯ PACS Picture archiving and communication system
⎯ TTP Trusted third party
⎯ XML Extensible mark-up language
⎯ VPN Virtual private network
8 © ISO 2010 – All rights reserved
5 General
Healthcare service providers are realizing many benefits when they are using digital technology for archiving
health records. The most commonly mentioned benefits are:
⎯ cost savings;
⎯ new possibilities for information sharing;
⎯ new ways to support clinical workflows;
⎯ data are available online on a 24 h/7 d basis.
From an archiving viewpoint, we have to understand that archiving personal health information in digital
format produces not only benefits, it also gives rise to new security and confidentiality problems:
⎯ digital material requires constant maintenance in order to stay alive;
⎯ digital information can be easily corrupted, disseminated and copied without recognition;
⎯ digitally stored information is easily accessed over traditional organizational borderlines;
⎯ digital documents have a shorter lifecycle than paper documents;
⎯ digital documents are usually closely linked to media, and any media we currently know may soon
become inaccessible;
⎯ information retrieval is dependent on software versions used;
⎯ risks due to malicious code and viruses.
For digital archiving, the difference between paper and digital is extreme. However, digital archiving is not a
healthcare-specific question. Digital libraries and many other organizations are developing both the
necessary technology and requirements for digital archiving. Based on the unique nature of healthcare
information, many healthcare-specific questions remain to be solved:
⎯ health information has very long preservation time (up to 100+ years);
⎯ healthcare data objects/documents are dynamic during the whole lifetime;
⎯ healthcare data are context sensitive;
⎯ the data content is sensitive;
⎯ a high degree of security, confidentiality and privacy protection is required;
⎯ there is a strong legal framework regulating who can access what and when;
⎯ data objects have context, purpose and sensitivity based access/disclose rules;
⎯ the nature of data can be legal for a given period;
⎯ non-repudiation of data and evidence should be secured during the whole preservation time.
6 EHR-archive and eArchiving process
6.1 EHR and record
6.1.1 Overview
In this Technical Specification we are defining security requirements for the long-term preservation of EHRs.
ISO 15489-1 is another International Standard already used in healthcare. Therefore it is necessary to
understand special features of the EHR.
There are a great variety of definitions for a record. A record is:
⎯ anything (e.g. document) providing permanent evidence of or information about past events;
⎯ a permanent form;
⎯ a document that can serve as legal evidence of a transaction;
⎯ recorded information;
⎯ a collection of related data;
⎯ what you retrieve when you search in a database;
⎯ a written document;
⎯ an individual component of a database;
⎯ a collection of related fields;
⎯ a database record consisting of one set of tuples for a given relational table; in a relational database,
records correspond to rows in each table;
⎯ a composite variable that can store data values of different types.
ISO 15489-1 has defined the record in the following way:
A record is information created, received, and maintained as evidence and information by an organization or
person, in pursuance of legal obligations or in the transaction of business.
The definition of health record varies in different countries. A number of definitions for the term “EHR" also
exist worldwide. There is no internationally accepted definition for the EHR (see ISO/TS 18308). Differences
reflect different shades of meaning between different countries and organizations. It is possible that the
information content of the EHR is restricted compared to the content of the Health Record. Generally we can
say that the Health Record may not equal EHR.
Two widely used definitions for the EHR are:
a) a comprehensive, structured set of clinical, demographic, environmental, social, and financial data and
information in electronic form documenting the healthcare given to a single individual (ASTM E1769);
b) a longitudinal collection (e.g. produced by encounters in one or more care settings) of personal health
information for a single individual, entered or accepted by a healthcare provider, and stored electronically
(HINA 2000).
It is also possible to speak about Regulated or Legal Health Records and Primary Records. AHIMA (American
Health Information Management Association) defines the legal health record as “generated at or for a
healthcare organization as its business records and is the record that would be released upon request”.
10 © ISO 2010 – All rights reserved
To highlight how the EHR has been defined in different countries, we can take two examples, the UK and
Finland. In the UK, the NHS the Code of Practice speaks about NHS records. Typical NHS records are:
⎯ patient records (e.g. GP medical record and speciality records);
⎯ records of private patients;
⎯ some registers (e.g. accident and operating theatre registers);
⎯ administrative records (e.g. financial and accounting records and notes).
In Finland the EHR is a legal record of a single patient created by the service provider organization producing
the care or treatment. This EHR is cumulative and lifelong at the level of a service provider. In Finland the Act
on Patients' Rights defines service provider organizations (e.g. secondary care hospital, primary healthcare
centre, occupational care service provider and a single private physician). This means that in Finland a citizen
can have many separate EHRs (which are cumulative at service provider organization level).
We can also speak about logical EHRs. A typical logical EHR is:
⎯ an institutional EHR;
⎯ a longitudinal EHR;
⎯ a lifelong EHR.
The institutional EHR can be:
⎯ a single physical record including all information on one inpatient or outpatient visit or treatment;
⎯ a combination of records created by a service provider organization (e.g. lab or X-ray records and records
created by specialities) during a patient's visit or an episode of care; in this case separate records are
typically linked together to form a logical EHR;
⎯ a cumulative personal record including information on all visits to one service provider organization; the
record can be a single physical cumulative record or it can include many linked cumulative sub-records
(or folders);
⎯ a collection of selected cross-organizational patient records.
Independent of the way the EHR is archived (e.g. as a single record or in the form of connected separate
records), it is necessary to prove not only the integrity of one record but also the integrity of all connected
records forming the logical EHR during the whole preservation time.
Typical solutions to manage an EHR including more that one fixed part are registration service, master index
table and metadata technology.
A variety of computer-based technologies to store and manage EHRs exist. Typical technologies used are:
⎯ relational databases;
⎯ document management systems;
⎯ image management systems;
⎯ picture management systems;
⎯ specialized systems storing biosignals.
Documents can also come in many formats, for example HL7 CDA, PDF or Word. Images can come in a
variety of formats such as JPG and TIFF.
One dimension of the EHR is the location where it is technically stored and managed. Typically it is stored in
the computer system of one service provider.
6.1.2 Distributed EHR architecture
Some countries use the distributed record architecture model. In this architecture the EHR can be defined as
a composite of physically distributed records (e.g. a summary of linked cross-organizational EHRs). In a
distributed model, it is possible that the management of the EHR is not in the hands of a single service
provider. Therefore, the management of integrity of distributed EHRs requires specific actions.
Technically, EHRs can be linked together either horizontally or vertically. In the case of a vertically linked,
distributed EHR, the link point is typically a master index file. It is also possible to duplicate some content of
distributed parts in the master repository (the SPINE in the UK is just this kind of master index repository).
6.1.3 Healthcare-specific features of the EHR
There are many healthcare-specific features in the EHR. One of them is that during its lifetime the content of
the EHR includes both dynamic and fixed parts. The content is dynamic during the direct care or treatment
process. Many health professionals and other persons who participate in the care process can manage the
content of the EHR based on their roles and privileges. It is also typical that some entities (e.g. automatic
analyser) can automatically add new information to the EHR.
2)
In most countries the content of the health record or some parts of it must be signed, after the care episode
or treatment, by the responsible physician in such a way that it is not possible to make modifications to the
record. After signature the content of the record shall not be changed i.e. the record can be called a fixed
record. Depending on the EHR-ar
...
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...