ISO/TS 9320:2024
(Main)Health informatics — Standardized data set for transfer of hemodialysis patients
Health informatics — Standardized data set for transfer of hemodialysis patients
The document defines a data set for the safe and timely transfer of haemodialysis procedure for end-stage renal disease (ESRD) patients. The necessary information for dialysis is provided through required, conditionally-required and optional data fields of the data set. Complicated use cases are also described in this document. This document does not cover general quality requirements or system requirements for haemodialysis.
Informatique de santé — Ensemble de données normalisées pour le transfert des patients en hémodialyse
General Information
- Status
- Published
- Publication Date
- 08-Aug-2024
- Technical Committee
- ISO/TC 215 - Health informatics
- Drafting Committee
- ISO/TC 215 - Health informatics
- Current Stage
- 6060 - International Standard published
- Start Date
- 09-Aug-2024
- Due Date
- 18-Apr-2025
- Completion Date
- 09-Aug-2024
Overview
ISO/TS 9320:2024 - Health informatics - Standardized data set for transfer of hemodialysis patients defines a structured, clinical data set to support the safe and timely transfer of haemodialysis (hemodialysis) care for patients with end‑stage renal disease (ESRD). The Technical Specification specifies required, conditionally required, and optional data fields and describes complicated use cases to ensure continuity of dialysis therapy during referrals, hospital admissions, surgery, intensive care or international travel.
This document does not set general quality or system requirements for haemodialysis; rather, it focuses on the clinical and operational data needed to deliver safe dialysis care across settings.
Key topics and technical requirements
- Data set structure: Classification of fields by required, conditionally-required and optional to prioritize essential information for safe dialysis handover.
- Core clinical fields (examples from the specification): last dialysis date, haemodialysis interval, dry weight, dialysis duration, haemodialysis machine model, blood flow rate, access type/site/status, dialysate parameters.
- Infectious disease status: Hepatitis B/C and HIV markers are included as required fields where relevant.
- Laboratory and physiological data (conditionally required): haemoglobin, sodium, potassium, calcium, phosphate, pre‑ and post‑dialysis vitals, interdialytic weight gain, last laboratory test date.
- Prescription and procedural notes: individualized dialysis prescription and remark fields to convey clinician instructions.
- Optional clinical context: heparin concentration, remnant kidney function, radiology reports, allergies, heart failure presence and ejection fraction, access construction date.
- Use cases and examples: the document details typical and complex referral scenarios (e.g., infectious patients, heart failure) and includes Annex A (referral paper example) and Annex B (example FHIR resource) to aid implementation.
- Interoperability focus: while not prescribing system requirements, the presence of a FHIR example supports mapping the dataset to health IT standards for data exchange.
Applications and users
ISO/TS 9320:2024 is immediately useful for:
- Dialysis clinics and nephrology teams coordinating referrals or covering travelling ESRD patients
- Hospital wards and intensive care units accepting dialysis patients
- Health IT vendors and EHR integrators implementing dialysis referral workflows and interoperability (FHIR mapping)
- Clinical informaticians, care coordinators and policy-makers developing referral templates and patient‑transfer protocols
Adoption improves patient safety by standardizing critical dialysis parameters, reducing errors during handover, and supporting efficient cross‑facility and cross‑border dialysis continuity.
Related standards
- The document contains no normative references but was prepared by ISO/TC 215 (Health informatics).
- Annex B provides an example FHIR resource, facilitating alignment with HL7 FHIR-based interoperability implementations where applicable.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

NYCE
Mexican standards and certification body.
Sponsored listings
Frequently Asked Questions
ISO/TS 9320:2024 is a technical specification published by the International Organization for Standardization (ISO). Its full title is "Health informatics — Standardized data set for transfer of hemodialysis patients". This standard covers: The document defines a data set for the safe and timely transfer of haemodialysis procedure for end-stage renal disease (ESRD) patients. The necessary information for dialysis is provided through required, conditionally-required and optional data fields of the data set. Complicated use cases are also described in this document. This document does not cover general quality requirements or system requirements for haemodialysis.
The document defines a data set for the safe and timely transfer of haemodialysis procedure for end-stage renal disease (ESRD) patients. The necessary information for dialysis is provided through required, conditionally-required and optional data fields of the data set. Complicated use cases are also described in this document. This document does not cover general quality requirements or system requirements for haemodialysis.
ISO/TS 9320:2024 is classified under the following ICS (International Classification for Standards) categories: 35.240.80 - IT applications in health care technology. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO/TS 9320:2024 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
Technical
Specification
ISO/TS 9320
First edition
Health informatics — Standardized
2024-08
data set for transfer of hemodialysis
patients
Informatique de santé — Ensemble de données normalisées pour
le transfert des patients en hémodialyse
Reference number
© ISO 2024
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
Contents Page
Foreword .v
Introduction .vi
1 Scope . 1
2 Normative references . 1
3 Terms, definitions and abbreviations . 1
3.1 Terms and definitions .1
3.2 Abbreviated terms .5
4 Significance of haemodialysis data set . 5
4.1 General .5
4.2 Unique elements in the haemodialysis data set .6
4.3 Purpose of a standardized data set.6
5 Use case . 7
5.1 General .7
5.2 Haemodialytic patient with no special problems .7
5.3 HIV positive haemodialytic patient .7
5.4 Haemodialytic patient with refractory heart failure .7
6 Data sets for transfer of haemodialysis . 8
6.1 General .8
6.2 Fields of required data.10
6.2.1 General .10
6.2.2 Last dialysis date . . .10
6.2.3 Haemodialysis interval .11
6.2.4 Dry weight .11
6.2.5 Haemodialysis machine model . 12
6.2.6 Haemodialysis blood flow rate . 12
6.2.7 Haemodialysis access type . 12
6.2.8 Haemodialysis access site . 13
6.2.9 Haemodialysis access status . 13
6.2.10 Hepatitis type B antigen / antibody.14
6.2.11 Hepatitis C virus infection .14
6.2.12 Human immunodeficiency virus infection . 15
6.2.13 Dialysis duration . 15
6.2.14 Dialysate .16
6.3 Fields of conditionally-required data .16
6.3.1 General .16
6.3.2 Initial dialysis date .16
6.3.3 Last laboratory test date .17
6.3.4 Blood type .17
6.3.5 Diagnosis .18
6.3.6 Blood haemoglobin concentration .18
6.3.7 Blood sodium concentration .19
6.3.8 Blood potassium concentration .19
6.3.9 Blood calcium concentration . 20
6.3.10 Blood phosphate concentration . 20
6.3.11 Venereal disease research laboratory .21
6.3.12 Pre-dialysis vital sign . 22
6.3.13 Post-dialysis vital sign . 22
6.3.14 Interdialytic weight gain . 23
6.3.15 Prescription . 23
6.3.16 Remark note .24
6.4 Fields of optional data .24
6.4.1 General .24
6.4.2 Heparin concentration .24
iii
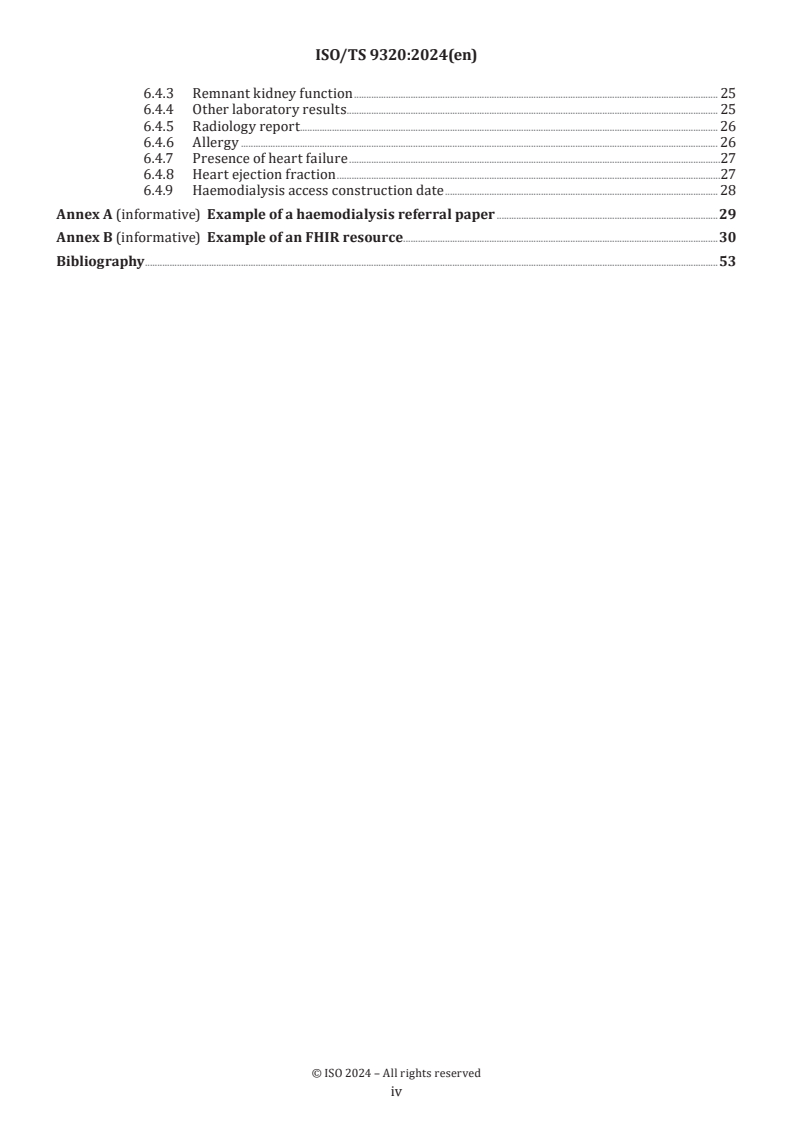
6.4.3 Remnant kidney function . 25
6.4.4 Other laboratory results . . 25
6.4.5 Radiology report. 26
6.4.6 Allergy . 26
6.4.7 Presence of heart failure .27
6.4.8 Heart ejection fraction .27
6.4.9 Haemodialysis access construction date . 28
Annex A (informative) Example of a haemodialysis referral paper .29
Annex B (informative) Example of an FHIR resource .30
Bibliography .53
iv
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out through
ISO technical committees. Each member body interested in a subject for which a technical committee
has been established has the right to be represented on that committee. International organizations,
governmental and non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely
with the International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are described
in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the different types
of ISO document should be noted. This document was drafted in accordance with the editorial rules of the
ISO/IEC Directives, Part 2 (see www.iso.org/directives).
ISO draws attention to the possibility that the implementation of this document may involve the use of (a)
patent(s). ISO takes no position concerning the evidence, validity or applicability of any claimed patent
rights in respect thereof. As of the date of publication of this document, ISO had not received notice of (a)
patent(s) which may be required to implement this document. However, implementers are cautioned that
this may not represent the latest information, which may be obtained from the patent database available at
www.iso.org/patents. ISO shall not be held responsible for identifying any or all such patent rights.
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and expressions
related to conformity assessment, as well as information about ISO's adherence to the World Trade
Organization (WTO) principles in the Technical Barriers to Trade (TBT), see www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 215, Health informatics.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
v
Introduction
Globally, the population with end-stage renal disease (ESRD) has steadily increased. Haemodialysis, which
provides rapid clearance of solutes, is the most popular renal replacement therapy for ESRD patients.
However, haemodialysis has a high risk of serious complications for receivers of the treatment. Well-known
complications of haemodialysis include hypotension, electrolyte imbalance, infection, fluid overload,
and dialysis disequilibrium. Due to these side-effects, patients who receive haemodialysis have lower life
expectancy than the general population.
Moreover, haemodialysis requires a patient to frequently visit a hospital and to go through complex
and time-consuming dialysis procedures. This is because patients need to know how to care for the
haemodialysis access or fistula, exercise, regulate diet and monitor their blood pressure and weight. In
addition, haemodialysis patients are more likely to be depressed because they are limited in many areas of
their daily activities.
Referral of haemodialysis cases occurs often due to complications of chronic kidney disease, such as
myocardial infarction, heart failure, atrial fibrillation and cerebrovascular accidents. Recently, a notable
change in these referral cases is the increase of referrals from abroad. One of the reasons behind this increase
is that haemodialysis which is done outside of a person’s residential area is covered by many payers in the
United States. As a result, international travel for haemodialysis is growing fast in east Asian countries.
Since haemodialysis includes a complex procedure and requires attentive monitoring, it is imperative to
share important and accurate information about a patient, dialysis setup and haemodialysis access to ensure
safe and timely haemodialysis. This would also allow patients who are travelling abroad for a haemodialysis
to experience smooth referral.
The purpose of this document is to define the data set for referral of haemodialysis patients. This data set
will ensure continuity of haemodialysis-related care. The data set provides optimal dialysate parameters
and individualized dialysis settings. Providing this information can reduce the occurrence of dialysis-
related complications. The data set can be used for referring haemodialysis patients, for surgery or intensive
care, and it can also support safe and timely haemodialysis procedures for ESRD patients from abroad.
vi
Technical Specification ISO/TS 9320:2024(en)
Health informatics — Standardized data set for transfer of
hemodialysis patients
1 Scope
The document defines a data set for the safe and timely transfer of haemodialysis procedure for end-
stage renal disease (ESRD) patients. The necessary information for dialysis is provided through required,
conditionally-required and optional data fields of the data set. Complicated use cases are also described in
this document.
This document does not cover general quality requirements or system requirements for haemodialysis.
2 Normative references
There are no normative references in this document.
3 Terms, definitions and abbreviations
3.1 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
3.1.1
haemodialysis
dialysis
therapy where waste solutes from the blood are removed by diffusion across an artificial extracorporeal
semipermeable membrane
3.1.2
haemodialysis interval
currently prescribed interval between haemodialysis (3.1.1) sessions
Note 1 to entry: The interval determines how effectively waste products and fluids are cleared from the body.
Note 2 to entry: A longer interval can lead to accumulation of harmful body products and water, resulting in
complications such as oedema, electrolyte imbalance and increased blood pressure.
3.1.3
dry weight
optimal or target weight that a patient should achieve during or after a treatment
Note 1 to entry: Dry weight is measured without the excess fluid that builds up between dialysis treatments.
Note 2 to entry: Dry weight is an important concept because it helps clinicians determine how much excess fluid needs
to be removed during each haemodialysis (3.1.1) session.
3.1.4
haemodialysis machine model
information about haemodialysis machine manufacturer and model used in recent haemodialysis (3.1.1)
sessions
Note 1 to entry: The product name of dialysate (3.1.9) varies depending on the machine model (the manufacturer's
product).
Note 2 to entry: The information helps clinicians prescribe dialysate in the receiving unit.
3.1.5
haemodialysis blood flow rate
rate at which a patient's blood is pumped through the dialysis machine during haemodialysis (3.1.1) treatment
Note 1 to entry: Haemodialysis blood flow rate is typically measured in millilitres per minute (ml/min) or litres per
hour (l/h).
Note 2 to entry: Clinicians need to determine the appropriate blood flow rate for each individual undergoing
haemodialysis to balance the benefits and potential risks.
3.1.6
haemodialysis access type
method or route by which blood is withdrawn from the patient's body, filtered through the dialysis machine,
and then returned to the patient
Note 1 to entry: Common types of haemodialysis access are arteriovenous fistula, arteriovenous graft and central
venous catheter.
3.1.7
haemodialysis access site
anatomical location of haemodialysis (3.1.1) access
Note 1 to entry: The preferred access site for an arteriovenous fistula is usually in the forearm.
3.1.8
haemodialysis access status
condition and functionality of the access site through which haemodialysis (3.1.1) treatments are performed
Note 1 to entry: Monitoring and assessing access status is necessary to ensure that the access site remains functional,
safe and free from complications.
Note 2 to entry: Haemodialysis access status usually refers to patency, infection, maturation and functionality.
3.1.9
dialysate
fluid used in dialysis to exchange solutes with the blood
Note 1 to entry: Dialysate is used to draw fluids and toxins out of the bloodstream and supply electrolytes and other
chemicals to the bloodstream
3.1.10
initial dialysis date
date on which a patient with end-stage renal disease (ESRD) begins haemodialysis (3.1.1) treatment for the
first time.
Note 1 to entry: Initial dialysis date is a significant event for patients, as it marks the beginning of a lifelong or long-
term commitment to regular dialysis treatments.
3.1.11
blood haemoglobin concentration
concentration of haemoglobin in whole blood
Note 1 to entry: Anaemia is a common complication in patients with chronic kidney disease.
Note 2 to entry: Haemoglobin is an important determinant for iron supplementation, blood transfusion or nutritional
assessment.
3.1.12
blood sodium concentration
concentration of sodium in serum or plasma
Note 1 to entry: Sodium is key for electrolytes in the body.
Note 2 to entry: Haemodialysis (3.1.1) patients are at risk of fluid and electrolyte imbalance due to impaired kidney
function and haemodialysis process.
3.1.13
blood potassium concentration
concentration of potassium in serum or plasma
Note 1 to entry: Potassium is key for electrolytes in the body.
3.1.14
blood calcium concentration
concentration of calcium in serum or plasma
Note 1 to entry: Calcium is key for electrolytes in the body.
3.1.15
blood phosphate concentration
concentration of phosphate in serum or plasma
Note 1 to entry: Phosphate is key for electrolytes in the body.
3.1.16
venereal disease research laboratory
nontreponemal test result for screening of syphilis
3.1.17
pre-dialysis vital sign
vital sign measured before haemodialysis (3.1.1) session
Note 1 to entry: Vital signs can be subcategorized in “blood pressure”, “heart rate”, “body temperature” and
“respiration rate.”
Note 2 to entry: Pre-dialysis vital signs help ensure patient’s safety and provide information about their readiness for
haemodialysis.
3.1.18
post-dialysis vital sign
vital signs measured after haemodialysis (3.1.1) session
Note 1 to entry: Vital sign can be subcategorized in “blood pressure”, “heart rate”, “body temperature” and
“respiration rate.”
Note 2 to entry: Post-dialysis vital signs are needed to assess haemodialysis response and to ensure patient’s safety.
3.1.19
interdialytic weight gain
amount of weight gain between two haemodialysis (3.1.1) sessions
Note 1 to entry: Interdialytic weight gain is the result of salt and water intake.
Note 2 to entry: Interdialytic weight gain helps clinicians assess how effectively the patient is managing fluid intake
and output between dialysis sessions.
Note 3 to entry: Interdialytic weight gain is used to determine the target fluid removal for each dialysis session.
3.1.20
remark note
note containing information or precautions regarding haemodialysis (3.1.1), disease management and
general patient-care
Note 1 to entry: A remark note is usually provided in plain text.
3.1.21
heparin concentration
concentration of an anticoagulant in haemodialysis (3.1.1) fluid required to prevent thrombosis in catheter,
filter and circuit
Note 1 to entry: Heparin concentration usually refers to heparin bolus dose as initial and maintenance dose.
3.1.22
remnant kidney function
renal working capacity remaining after haemodialysis (3.1.1)
Note 1 to entry: Remnant kidney function is usually measured as daily urine output or glomerular filtration rate
(3.1.29).
3.1.23
other laboratory results
laboratory examination of a blood sample other than those mentioned among required and conditionally-
required data set
3.1.24
radiology report
text that represents the interpretation of a radiological study
3.1.25
allergy
altered bodily reactivity (such as hypersensitivity) to an antigen in response to a first exposure
3.1.26
presence of heart failure
presence of a condition in which the heart cannot pump enough blood to meet the body's needs
Note 1 to entry: Haemodialysis (3.1.1) patients are at an elevated risk of cardiovascular complications.
Note 2 to entry: Managing heart failure is important for fluid management, blood pressure control and dialysis
procedure.
3.1.27
heart ejection fraction
measure of cardiac function reflecting the average fraction of emptying of the left ventricle with each
contraction
Note 1 to entry: Heart ejection fraction is a crucial indicator of heart function and is commonly assessed using
echocardiography.
3.1.28
haemodialysis access construction date
procedure date of current haemodialysis (3.1.1) access
Note 1 to entry: Haemodialysis access construction date helps clinicians check the duration of access use and
complications that can arise over time.
3.1.29
glomerular filtration rate
calculated measure of renal function which is expressed by the total volume of fluid filtered through all
renal glomeruli in a minute
Note 1 to entry: The glomerular filtration rate is usually corrected for estimated body surface area, and reported in
ml/min/1,73 m .
3.2 Abbreviated terms
ESRD end-stage renal disease
HD haemodialysis
HBsAg surface antigen of the hepatitis B virus
HBV hepatitis B virus
HCV hepatitis C virus
HIV human immunodeficiency virus
LOINC Logical Observation Identifiers Names and Codes
FHIR Fast Healthcare Interoperability Resources
VDRL venereal disease research laboratory
GFR glomerular filtration rate
NYHA New York Heart Association
4 Significance of haemodialysis data set
4.1 General
Haemodialysis is one method of renal replacement therapy for ESRD patients. Since ESRD patients do not
have functioning kidneys, patients experience symptoms such as water retention and accumulation of waste
metabolites. Typically, ESRD patients require extracorporeal blood circulation that connects to the patient’s
vascular structures (vascular access), which are artificially constructed in the body.
The basic principle of haemodialysis is to remove unnecessary body water and toxic wastes, such as urea
and creatinine, by extracorporeal filtration of patients’ blood. Haemodialysis is conventionally performed
and managed by highly trained staff. Furthermore, many clinics have specialized haemodialysis facilities
such as high-quality water purification system and electricity system. The facility should apply additional
measures to prevent microbial contamination.
Although the number of haemodialysis medical institutions and haemodialysis machines is steadily
increasing, it is difficult to manage the quality of haemodialysis treatment for various reasons. Patients' lack
of awareness of their dialysis data and their non-compliance to medical staff’s instructions are obstacles to
the improvement of patient’s life quality and the reduction of mortality in ESRD patients. Additionally, ESRD
patients usually suffer from severe anaemia, malnutrition, hyperparathyroidism, hyperphosphatemia,
hypocalcaemia, metabolic acidaemia, hypertension and congestive heart failure at the start of dialysis.
Hypoalbuminemia, anaemia and left ventricular hypertrophy are common side effects of dialysis treatment.
Sometimes dialysis results in premature death. Details of these cases should be communicated through
standardized data set so that this ultimately leads to improvement in dialysis treatment and better prognosis
[8],[9]
for ESRD patients.
4.2 Unique elements in the haemodialysis data set
There are unique data elements that exist only for haemodialysis and these elements are sometimes
misleading. Procedural data is often misunderstood as observational data. Caution is required as the
meaning of a specific data element can be conveyed inaccurately. Some data sets do not use standard medical
terminology. Table 1 provides unique data elements which exist only in the haemodialysis domain and often
lack standard terminology.
Table 1 — Unique data elements in haemodialysis
Elements Element description and its significance
Dry weight — Target weight of haemodialysis without fluid overload or hypovolemia.
— It should not be misinterpreted as common body weight.
Haemodialysis blood flow rate — Blood flow in haemodialysis machine.
— It should not be misinterpreted as the blood flow in the patient's body.
— It represents setting value in the haemodialysis machine.
Haemodialysis access — Body site to reach the blood for haemodialysis.
Dialysate — Kind of chemical bath used in dialysis to draw fluids and toxins out of the blood
stream.
— It is not considered as medication data.
Interdialytic weight gain — Amount of weight gain as a result of salt and water intake between two
haemodialysis sessions.
— It is used as value to calculate target weight during haemodialysis.
— It should not be misinterpreted as common weight gain.
Haemodialysis machine model — Information of haemodialysis machine manufacturer and model.
— Importance of model is often neglected.
— Standard terminology not given.
4.3 Purpose of a standardized data set
Safe and timely haemodialysis requires a complex set of data and it is practically unfeasible for a patient to
remember each element. Therefore, it has been a common practice to carry paper-based data when they are
transferred (see Annex A). A standard haemodialysis data set benefits both patients and medical staff by
electronically transferring relevant and accurate dialysis data.
Moreover, a standard haemodialysis data set can provide safe dialysis to patients by reducing the possibility
of haemodialysis-related complications. Haemodialysis is a care-intensive process that requires the utmost
attention to prevent various complications. For example, if haemodialysis parameters are set inappropriately,
too much water can be removed from patients which can lead to hypovolemia, hypotension and fatigue.
Therefore, it is critical to have data from previous dialysis about end-dialysis weight and dialysis speed.
Such information can be accurately and electronically transferred from one medical institution to another
using the standardized data set proposed in this document.
Timely haemodialysis is important, because delays in haemodialysis schedule can lead to worsening uraemia,
increased infection susceptibility and other preventable complications. Sometimes, medical staff need to
additionally contact the medical institution that issued the referral because patients did not know all the
necessary information for their haemodialysis. Since the standardized data set proposed in this document
provides basic parameters to start and monitor haemodialysis procedure, it can reduce the time for medical
staff to prepare a haemodialysis session.
5 Use case
5.1 General
Haemodialysis transfer is a multidisciplinary process because it involves wide range of agenda, including
educating a patient on diet and exercise and explaining inadvertent complications of haemodialysis to the
patient’s family members.
A transfer can be done for various reasons, for example if the patient needs a procedure unrelated to kidney
issues or if they move to another state. It can also occur if the patient’s family planned a family trip to a near-
by country.
Reviewing the data elements in the proposed data set provides helpful information to medical staff,
especially in the case of a haemodialysis patient who is planned to be transferred. For instance, the time
between receiving the data and the patient's visit would help medical staff to evaluate risk factors for the
upcoming transfer and to decide on appropriate transfer time. Sending the proposed data set to a recipient
hospital is more than a simple data transfer because it helps a recipient hospital prepare for unexpected
events that can occur at any step of the transfer process. Detailed information on the transfer process should
be shared with the patient, and discussions can be necessary with patient’s custodians.
Patients can have very different complication risks depending on their age, race and comorbidities. Some
patients can develop repetitive complications by haemodialysis and can develop similar complications in the
recipient hospital. Repetitive adverse events can be notified and can be prevented. Sometimes it is necessary
to contact the recipient hospital to query whether all necessary medical equipment is ready for expected
emergency.
5.2, 5.3 and 5.4 are intended to provide several use cases with different risks of complication.
5.2 Haemodialytic patient with no special problems
In this use case, the haemodialysis patient has had stable haemodialysis repeatedly. The patient is young.
Vital signs are stable. No adverse event has been notable in repeated haemodialysis session. The patient can
be transferred with only the required data set. Other fields are either conditionally-required or optional.
The required, conditionally-required and optional field are further explained in Clause 6.
5.3 HIV positive haemodialytic patient
When a haemodialytic patient is HIV positive, additional measures should take place to minimize the risk of
spreading HIV to other patients and clinic staff. HIV test result shall be included in the data set. Clinic staff
are also required to share the information because careless contacts with the patient must be avoided. Also,
a recipient haemodialysis clinic must provide a haemodialysis machine which is dedicated to HIV patients.
Before referral, a physician can contact the recipient hospital for the availability of HIV haemodialysis. Since
an HIV dedicated machine is equipped in limited numbers, it is imperative to check that schedules are not
overlapping and that those machines are ready for the next scheduled haemodialysis.
5.4 Haemodialytic patient with refractory heart failure
Heart failure and renal dysfunction can coexist. The number of comorbidities increases over time. A critical
issue with this combination is that each disease can exacerbate another. ESRD can lead to retention of water
which can cause cardiac dysfunction. ESRD can also exacerbate heart failure progressively and finally make
it refractory to treatment. A possible treatment approach can be to address the treatable cause of valvular
heart disease. Physicians should deal with the volume of excess fluid. Patients are requested to reduce the
dietary intake of salt during the transfer process. The data set which is related to heart failure shall be
transmitted before transfer process. The recipient clinic shall make a decision on whether they accept the
transfer. Medication should be also monitored and approximated because renal dysfunction commonly
limits the use of medication on cardiac problems.
6 Data sets for transfer of haemodialysis
6.1 General
In this document, data set types are categorized as required, conditionally-required and optional. Data sets
are also categorized according to when they are needed, so they are defined as needed before, during or
after the haemodialysis procedure. Data sets are also categorized according to the importance of the
dialysis procedure, as the focus is on the dialysis procedure rather than general health. Therefore, they may
differ from general healthcare data sets. Table 2 shows the overall data tabulated and accompanied by the
necessary metadata, including a glossary of terms and brief examples with code and value property. Also,
more detailed exemplary data are provided in Annex B.
Table 2 — data elements for haemodialysis
a
Attribute name/Data Coding Code value Data value type Qualifier
element name system
Last dialysis date Applicable DateTime R
terminology
Haemodialysis interval LOINC LOINC 50951-9 DateTime R
Interdialytic time (ESRD)
Dry weight LOINC LOINC 8341-0 kg, lb R
Dry body weight measured
Haemodialysis machine Text R
model
Haemodialysis blood flow LOINC LOINC 99711-4 ml/min R
rate
Blood flow rate Renal
replacement therapy circuit
Haemodialysis access type LOINC LOINC 72050-8 LOINC Answer List R
LL2169-2 ESRD-dialysis
Dialysis access
access type
Haemodialysis access site LOINC LOINC 99715-5 SNOMED Body Structure R
Dialysis access site
Haemodialysis access LOINC LOINC 99716-3 LOINC Answer List R
status LL2150-8 Access site
Dialysis access site appearance
apperance
Hepatitis type B antigen / LOINC LOINC 5195-3 LOINC Answer List R
antibody LL3865-4 True|-
Hepatitis B virus surface Ag
False|Unknown
(presence) in serum
Hepatitis C virus infection LOINC LOINC 11259-9 LOINC Answer List R
LL3865-4 True|-
Hepatitis C virus RNA
False|Unknown
(presence) in serum or plasma
Human immunodeficiency LOINC LOINC 7917-8 LOINC Answer List R
virus infection LL3865-4 True|-
HIV 1 Ab (Presence) in serum
False|Unknown
Dialysis duration LOINC LOINC 68489-4 Hours R
Dialysis hours per session
Dialysate LOINC LOINC 99732-0 Text R
Dialysate fluid renal
replacement therapy circuit
Initial dialysis date Applicable DateTime C (6.3.2.2)
terminology
Last laboratory test date Applicable DateTime C (6.3.3.2)
terminology
a
R = required; C = conditionally required; O = optional.
TTaabbllee 22 ((ccoonnttiinnueuedd))
a
Attribute name/Data Coding Code value Data value type Qualifier
element name system
Blood type LOINC LOINC 882 LOINC Answer List C (6.3.4.2)
LL2972-9 ABORh
ABO and Rh group (type) in
blood
Diagnosis ICD 10/11, ICD10 M47 Code, List of Codes C (6.3.5.2)
SNOMED Spondylosis arthrosis or
osteoarthritis of spine
Applicable
Terminology
Blood haemoglobin LOINC LOINC 42810-2 Haemoglobin g/dl C (6.3.6.2)
concentration (mass/volume)
in blood
Blood sodium concentration LOINC LOINC 2951-2 mmol/l C (6.3.7.2)
Sodium (moles/volume) in
serum or plasma
Blood potassium LOINC LOINC 2823 mmol/l C (6.3.8.2)
concentration
Potassium (moles/volume) in
serum or plasma
Blood calcium LOINC LOINC 2000-8 mmol/l C (6.3.9.2)
concentration
Calcium (moles/volume) in
serum or plasma
Blood phosphate LOINC LOINC 2777-1 mg/dl C (6.3.10.2)
concentration
Phosphate (mass/volume) in
serum or plasma
Venereal disease LOINC LOINC 5292-8 LOINC Answer List C (6.3.11.2)
LL3865-4 True|-
search laboratory Reagin Ab in serum
False|Unknown
Pre/post- Systolic LOINC LOINC 8480-6 mmHg
dialysis
Blood Systolic blood pressure
vital sign
pressure
Diastolic LOINC LOINC 8462-4 mmHg
blood
Diastolic blood pressure
pressure
C (6.3.12.2,
Heart rate LOINC LOINC 8867-4 /min
6.3.13.2)
Heart rate
Respiration LOINC LOINC 9279-1 /min
rate
Respiratory rate
Body LOINC LOINC 8310-5 Degrees Celsius,
temperature Fahrenheit
Body temperature
°C, °F
Interdialytic weight gain LOINC LOINC-74006-8 Numeric (kg, lb) C (6.3.14.2)
Weight difference: pre-dialysis
vs. post-dialysis
Prescription RxNorm, RxCUI 385629 Code/ List of Codes C (6.3.15.2)
SNOMED
Acetaminophen 5 mg/ml
Remark note Applicable Not determined Text C (6.3.16.2)
terminology
Heparin concentration Applicable Not determined Heparin unit/dose O
terminology
Remnant kidney function LOINC LOINC 9188-4 ml/h O
urine output 1 hour
a
R = required; C = conditionally required; O = optional.
TTaabbllee 22 ((ccoonnttiinnueuedd))
a
Attribute name/Data Coding Code value Data value type Qualifier
element name system
Other laboratory result LOINC / LOINC 789-8 Numeric /nominal O
SNOMED
erythrocytes in blood by /ordinal depending on
applicable
automated count element
terminology
Radiology report LOINC LOINC 18782-3 Text O
Radiology study observation
Allergy LOINC LOINC 48765-2 Text/Code (SNOMED O
703925004)
Allergies and adverse reactions
and document
Presence of heart failure LOINC 88020-3 LOINC Answer List O
(LL4734-1, NYHA FA:
Functional capacity NYHA
Class I | Class II | Class
III | Class IV)
Heart ejection fraction LOINC 10230-1 Numeric (%) O
left ventricular ejection
fraction
Haemodialysis access LOINC DateTime O
construction date
a
R = required; C = conditionally required; O = optional.
6.2 Fields of required data
6.2.1 General
The required data set is composed of information that helps clinicians making critical decisions and making
sessions manageable by haemodialysis staff. For example, when medical staff are about to start a dialysis
session, the data set helps them choose which machine to use and setting the parameters of a procedure.
Infectious markers, such as HIV, HCV and HBV shall be included in the required data set. The information
is important when a dialysis is prepared and during the initial stage of the procedure. When a patient is
referred, all required data field shall be filled. The data elements are summarized in Table 2. The table covers
terminology, data type and meta data.
6.2.2 Last dialysis date
6.2.2.1 Purpose
It is the date of most recent haemodialysis, which is required for deciding next dialysis schedule. Patients
will suffer accumulation of toxins, fluid retention and electrolyte imbalance if they don’t follow prescribed
schedule of haemodialysis. Usually, patients are also instructed on the importance of haemodialysis schedule.
6.2.2.2 Business rules
a) This is a required element and shall be in the data set.
b) Unknown and known absence should be stated explicitly.
6.2.2.3 Missing data
This is a required element for conformance and shall not be empty; at least, a statement shall be given
explaining the missing data.
6.2.2.4 Example
“url”: “last-dialysis-date”
“performedDateTime”: “2022-08-22”
6.2.3 Haemodialysis interval
6.2.3.1 Purpose
It refers to currently prescribed interval between haemodialysis sessions. It provides information on when
to st
...
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...