ISO 29943-2:2017
(Main)Condoms — Guidance on clinical studies — Part 2: Female condoms, clinical function studies based on self-reports
Condoms — Guidance on clinical studies — Part 2: Female condoms, clinical function studies based on self-reports
ISO 29943-2:2017 is intended to help in the design, execution, analysis, and interpretation of clinical function studies conducted in accordance with the requirements of ISO 25841 for female condoms. These clinical studies compare the performance of a new female condom to an established female condom during vaginal intercourse (not anal intercourse). In particular, these studies are designed to assess acute failure events during use. ISO 29943-2:2017 also provides direction on the analysis of data when the study is completed, as well as interpretation of these results by manufacturers and regulatory bodies. Certain clinical trial elements are not addressed in this document, including compensation, confidentiality of individuals and their records, use of local ethics committees, etc. These and many other clinical trial design issues are covered in greater detail in ISO 14155.
Préservatifs — Lignes directrices relatives aux études cliniques — Partie 2: Préservatifs féminins, analyse fonctionnelle des défaillances graves sur la base d'auto-déclarations
General Information
- Status
- Published
- Publication Date
- 05-Jul-2017
- Technical Committee
- ISO/TC 157 - Non-systemic contraceptives and STI barrier prophylactics
- Drafting Committee
- ISO/TC 157/WG 20 - Clinical trials
- Current Stage
- 9093 - International Standard confirmed
- Start Date
- 08-Dec-2023
- Completion Date
- 12-Feb-2026
Overview
ISO 29943-2:2017 - Condoms: Guidance on clinical studies - Part 2: Female condoms, clinical function studies based on self‑reports provides practical guidance for designing, conducting, analysing and interpreting clinical function studies of female condoms. It focuses on comparative trials that assess a new female condom against an established product during vaginal intercourse (not anal intercourse) and is targeted at detecting acute failure events (e.g., breakage, slippage, invagination, misdirection) as reported by study participants.
Key topics and requirements
- Study scope and objectives: Guidance for clinical validation investigations aligned with the requirements of ISO 25841 for female condoms, with emphasis on acute failure outcomes rather than direct assessment of pregnancy or STI protection.
- Risk assessment and pilot studies: Recommendations to identify device‑specific failure modes and plan pilot investigations before full trials.
- Study design elements: Instructions on outcome measures, enrolment criteria, informed consent, test vs control condom selection, randomization, allocation concealment, and masking.
- Data collection and integrity: Detailed approaches for interviews, Case Report Forms (CRFs), interactive voice response systems (IVRS), web/mail reporting, and compiling use‑event data from self‑reports.
- Product handling: Control of the distribution chain and protocols for analysis of returned used condoms.
- Statistical analysis: Advice on statistical analysis plans, primary/secondary hypotheses, sample size/power considerations, and interpretation of non‑inferiority or superiority results.
- Annexes and templates: Informative annexes with sample CRFs, protocol outlines, time/event schedules, a power calculation formula and a protocol for evaluating returned condoms.
Applications
- Supporting regulatory submissions that require clinical function evidence for a new female condom design.
- Designing randomized or crossover human use studies that rely on self‑reported user data.
- Developing study protocols, CRFs and data collection systems for condom validation trials.
- Interpreting clinical failure rates to inform product development, lab testing, and risk mitigation.
Who should use this standard
- Medical device and condom manufacturers developing female condoms.
- Clinical researchers and investigators planning human use studies.
- Contract Research Organizations (CROs) executing comparative function trials.
- Regulatory reviewers and quality/regulatory affairs professionals evaluating clinical data.
Related standards
- ISO 25841 - normative requirements for female condoms.
- ISO 14155 - clinical investigation of medical devices (ethical and trial conduct requirements).
- ISO 14971 - risk management for medical devices (risk assessment guidance).
ISO 29943-2:2017 is a practical, study‑focused reference to ensure consistent, robust clinical function evidence for female condom performance based on participant self‑reports.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
ISO 29943-2:2017 is a standard published by the International Organization for Standardization (ISO). Its full title is "Condoms — Guidance on clinical studies — Part 2: Female condoms, clinical function studies based on self-reports". This standard covers: ISO 29943-2:2017 is intended to help in the design, execution, analysis, and interpretation of clinical function studies conducted in accordance with the requirements of ISO 25841 for female condoms. These clinical studies compare the performance of a new female condom to an established female condom during vaginal intercourse (not anal intercourse). In particular, these studies are designed to assess acute failure events during use. ISO 29943-2:2017 also provides direction on the analysis of data when the study is completed, as well as interpretation of these results by manufacturers and regulatory bodies. Certain clinical trial elements are not addressed in this document, including compensation, confidentiality of individuals and their records, use of local ethics committees, etc. These and many other clinical trial design issues are covered in greater detail in ISO 14155.
ISO 29943-2:2017 is intended to help in the design, execution, analysis, and interpretation of clinical function studies conducted in accordance with the requirements of ISO 25841 for female condoms. These clinical studies compare the performance of a new female condom to an established female condom during vaginal intercourse (not anal intercourse). In particular, these studies are designed to assess acute failure events during use. ISO 29943-2:2017 also provides direction on the analysis of data when the study is completed, as well as interpretation of these results by manufacturers and regulatory bodies. Certain clinical trial elements are not addressed in this document, including compensation, confidentiality of individuals and their records, use of local ethics committees, etc. These and many other clinical trial design issues are covered in greater detail in ISO 14155.
ISO 29943-2:2017 is classified under the following ICS (International Classification for Standards) categories: 11.200 - Birth control. Mechanical contraceptives. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO 29943-2:2017 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
INTERNATIONAL ISO
STANDARD 29943-2
First edition
2017-07
Condoms — Guidance on clinical
studies —
Part 2:
Female condoms, clinical function
studies based on self-reports
Préservatifs — Lignes directrices relatives aux études cliniques —
Partie 2: Préservatifs féminins, analyse fonctionnelle des défaillances
graves sur la base d’auto-déclarations
Reference number
©
ISO 2017
© ISO 2017, Published in Switzerland
All rights reserved. Unless otherwise specified, no part of this publication may be reproduced or utilized otherwise in any form
or by any means, electronic or mechanical, including photocopying, or posting on the internet or an intranet, without prior
written permission. Permission can be requested from either ISO at the address below or ISO’s member body in the country of
the requester.
ISO copyright office
Ch. de Blandonnet 8 • CP 401
CH-1214 Vernier, Geneva, Switzerland
Tel. +41 22 749 01 11
Fax +41 22 749 09 47
copyright@iso.org
www.iso.org
ii © ISO 2017 – All rights reserved
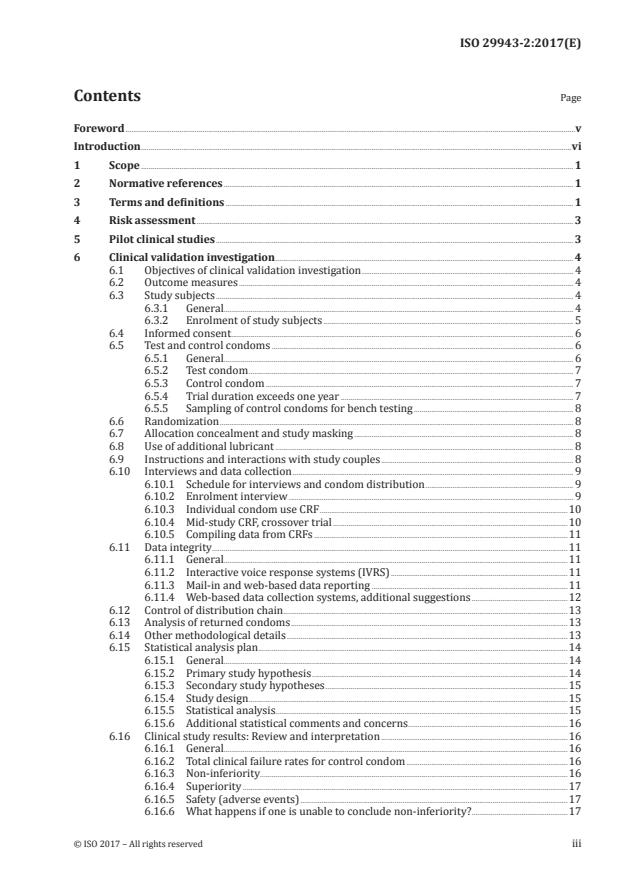
Contents Page
Foreword .v
Introduction .vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 1
4 Risk assessment . 3
5 Pilot clinical studies . 3
6 Clinical validation investigation . 4
6.1 Objectives of clinical validation investigation . 4
6.2 Outcome measures . 4
6.3 Study subjects . 4
6.3.1 General. 4
6.3.2 Enrolment of study subjects . 5
6.4 Informed consent . 6
6.5 Test and control condoms . 6
6.5.1 General. 6
6.5.2 Test condom . 7
6.5.3 Control condom . 7
6.5.4 Trial duration exceeds one year . 7
6.5.5 Sampling of control condoms for bench testing . 8
6.6 Randomization . 8
6.7 Allocation concealment and study masking . 8
6.8 Use of additional lubricant . 8
6.9 Instructions and interactions with study couples . 8
6.10 Interviews and data collection . 9
6.10.1 Schedule for interviews and condom distribution . 9
6.10.2 Enrolment interview . 9
6.10.3 Individual condom use CRF .10
6.10.4 Mid-study CRF, crossover trial .10
6.10.5 Compiling data from CRFs .11
6.11 Data integrity .11
6.11.1 General.11
6.11.2 Interactive voice response systems (IVRS) .11
6.11.3 Mail-in and web-based data reporting .11
6.11.4 Web-based data collection systems, additional suggestions .12
6.12 Control of distribution chain .13
6.13 Analysis of returned condoms .13
6.14 Other methodological details .13
6.15 Statistical analysis plan .14
6.15.1 General.14
6.15.2 Primary study hypothesis .14
6.15.3 Secondary study hypotheses .15
6.15.4 Study design .15
6.15.5 Statistical analysis . .15
6.15.6 Additional statistical comments and concerns .16
6.16 Clinical study results: Review and interpretation .16
6.16.1 General.16
6.16.2 Total clinical failure rates for control condom .16
6.16.3 Non-inferiority .16
6.16.4 Superiority .17
6.16.5 Safety (adverse events) .17
6.16.6 What happens if one is unable to conclude non-inferiority? .17
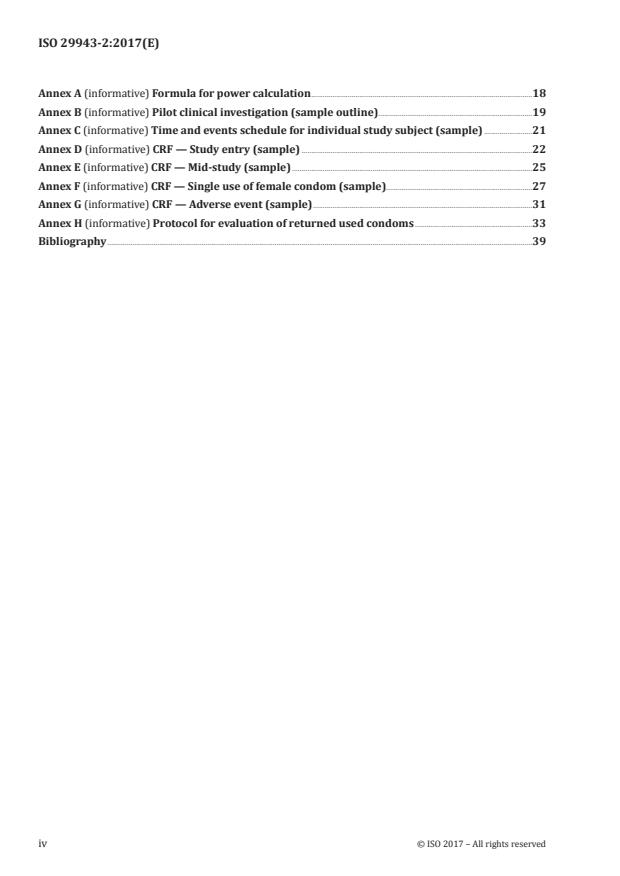
Annex A (informative) Formula for power calculation .18
Annex B (informative) Pilot clinical investigation (sample outline) .19
Annex C (informative) Time and events schedule for individual study subject (sample) .21
Annex D (informative) CRF — Study entry (sample) .22
Annex E (informative) CRF — Mid-study (sample) .25
Annex F (informative) CRF — Single use of female condom (sample).27
Annex G (informative) CRF — Adverse event (sample) .31
Annex H (informative) Protocol for evaluation of returned used condoms .33
Bibliography .39
iv © ISO 2017 – All rights reserved
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www .iso .org/ directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received (see www .iso .org/ patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation on the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO’s adherence to the
World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT) see the following
URL: w w w . i s o .org/ iso/ foreword .html.
This document was prepared by Technical Committee ISO/TC 157, Non-systemic contraceptives and STI
barrier prophylactics.
A list of all the parts of ISO 29943 can be found on the ISO website.
Introduction
There is limited information on the safety and effectiveness of female condoms. Therefore, clinical
validation of any new female condom is necessary to ensure that its performance during actual use is
not inferior to the performance of female condoms of existing designs.
This clinical study guidance is intended to help in the design, execution, analysis, and interpretation
of clinical function studies conducted in accordance with requirements of ISO 25841 for female
condoms. In addition to information regarding the clinical validation study, this document provides
recommendations on risk assessment, pilot studies, and statistical analysis plans. Annexes include
previously used case report forms (CRF) and protocols that can be modified or adapted.
To date, there has been considerable variation in female condom designs and materials. Many female
condoms are held in place with external rings and are often anchored within the vagina using rings,
sponges or other unique designs. From the published literature, the most common acute failure events
associated with female condom use are breakage, slippage, invagination and misdirection. However, the
definitions for these acute failure events have been inconsistent from one published study to another. A
sponsor planning to conduct a female condom study should review the definitions in this document to
determine their applicability for the product.
For further information regarding definitions of female condom failures, refer to Reference [12] and
Reference [16]. Also, note that the definitions used in this document are based on existing designs and
might need to be expanded or adapted according to the female condom under investigation. Other types
of acute failure events (unique to a particular design) can be identified as part of the risk assessment
per ISO 14971 or during the pilot study.
NOTE Based on the normative clinical requirement of relevant standards, these studies are designed to
recruit participating couples who agree to use the test and control condoms for vaginal intercourse. Such studies
can also collect incidental data on condom use during anal sex; however, that is not the primary objective. To
satisfy study power requirements, it is critical that sufficient reports are collected on condom use during vaginal
intercourse. Study sponsors typically take preventive measures, such as initial screening and consenting of study
couples, and obtain agreement that study couples will use condoms this way.
It should also be noted that these clinical function studies are not typically designed to directly evaluate
condom protection against pregnancy or sexually transmitted infections (STIs).
Finally, it is important to recognize that clinical function studies of condoms are human research
studies. Therefore, all persons designing, conducting, and analysing clinical studies of new female
condoms should be familiar with all relevant requirements for research involving human subjects,
including ethical considerations. For additional information, refer to ISO 14155.
vi © ISO 2017 – All rights reserved
INTERNATIONAL STANDARD ISO 29943-2:2017(E)
Condoms — Guidance on clinical studies —
Part 2:
Female condoms, clinical function studies based on self-
reports
1 Scope
This document is intended to help in the design, execution, analysis, and interpretation of clinical
function studies conducted in accordance with the requirements of ISO 25841 for female condoms.
These clinical studies compare the performance of a new female condom to an established female
condom during vaginal intercourse (not anal intercourse). In particular, these studies are designed to
assess acute failure events during use.
This document also provides direction on the analysis of data when the study is completed, as well as
interpretation of these results by manufacturers and regulatory bodies.
Certain clinical trial elements are not addressed in this document, including compensation,
confidentiality of individuals and their records, use of local ethics committees, etc. These and many
other clinical trial design issues are covered in greater detail in ISO 14155.
2 Normative references
There are no normative references in this document.
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at http:// www .iso .org/ obp
— IEC Electropedia: available at http:// www .electropedia .org/
NOTE All of the clinical failure events defined below represents potential vaginal exposure to semen and
other penile discharge. Non-clinical failure events do not risk exposure.
3.1
clinical breakage
breakage or tearing of the condom during intercourse or withdrawal from the vagina
Note 1 to entry: This might not be noticed until after inspection of the condom following intercourse.
Note 2 to entry: Any breakages that do not meet the definition of clinical breakage are considered “non-clinical
breakage” (e.g. tearing the condom when opening the package).
3.2
clinical breakage rate
number of female condoms broken or torn during intercourse or withdrawal divided by the number of
female condoms used during intercourse
Note 1 to entry: The clinical breakage rate is typically reported as a percentage.
3.3
clinical slippage
condom slipping completely out of the vagina during intercourse
Note 1 to entry: If a condom slips off primarily as a result of breakage, do not count that as a slippage event.
3.4
clinical slippage rate
number of female condoms that slipped completely out of the vagina divided by the number of female
condoms used during intercourse
Note 1 to entry: The clinical slippage rate is typically reported as a percentage.
3.5
clinical misdirection
insertion of the penis between the female condom and the vaginal wall
3.6
clinical misdirection rate
number of female condoms that misdirect divided by the number of female condoms used during
intercourse
Note 1 to entry: The clinical misdirection rate is typically reported as a percentage.
3.7
clinical invagination
external retention feature of the female condom that is partially or fully pushed into the vagina during
intercourse
3.8
clinical invagination rate
number of female condoms that invaginate divided by the number of female condoms used during
intercourse
Note 1 to entry: The clinical invagination rate is typically reported as a percentage.
3.9
clinical failure event
clinical breakage (3.1), clinical slippage (3.3), clinical misdirection (3.5) or clinical invagination (3.7)
3.10
total clinical failure
number of female condoms with at least one acute failure event that results in potential vaginal
exposure to semen and other penile discharge
Note 1 to entry: Any condom that experiences multiple clinical failure events (3.9) only counts as a single clinical
failure.
Note 2 to entry: Includes condoms with the following failures: clinical breakage (3.1), slippage (3.3), misdirection
(3.5), invagination (3.7), or any failure event(s) in the risk assessment as described in Clause 4.
3.11
total clinical failure rate
number of female condoms with clinical failure divided by the number of female condoms used during
intercourse
Note 1 to entry: The total clinical failure rate is typically reported as a percentage.
2 © ISO 2017 – All rights reserved
3.12
bias
systematic error caused by a variable not considered in the calculation of results
Note 1 to entry: Three common causes of bias in this type of clinical study are (1) selection bias, where certain
types of study subjects are not representative for the outcome being assessed, (2) recall bias, where poor
questionnaire design or lengthy time between when condom is used and when the use events are recorded, and
(3) misclassification, where the outcome of interest (e.g. breakage, slippage, invagination, or misdirection) is
recorded erroneously.
Note 2 to entry: The term bias is used in statistics to refer to how far the expected value of a statistic lies from the
parameter it is estimating.
3.13
non-inferiority margin
δ
statistical term used to identify a clinically meaningful difference between products
Note 1 to entry: Differences between product means which are less than δ are interpreted as noise inherent in
the study while differences between product means which are greater than δ are attributed to a meaningful
difference between products.
4 Risk assessment
A risk assessment for the product shall be conducted in accordance with ISO 14971. This assessment
should identify all safety and effectiveness concerns, including potential mechanisms of condom failure
and the results of the pilot study. All possible acute failure events should be considered in the design
of the female condom, and clinical investigations should be designed to capture information on each
possible type of failure.
The risk assessment should address whether each acute failure event leads to potential vaginal
exposure to semen and other penile discharge during condom use, and therefore whether each failure
event is designated clinical or non-clinical.
Manufacturers should make this risk assessment available to regulatory bodies.
5 Pilot clinical studies
A pilot study helps to identify and evaluate the different types of acute failure events of the new female
condom prior to initiation of a larger clinical investigation (see ISO 25841:2014, Clause 8). The acute
failure rates obtained in the pilot study will influence the statistical calculations of power and sample
size for the pivotal study. The risk assessment (see Clause 4) should be conducted prior to the pilot
study and then repeated after the pilot study, with any new types of failure events reported in the pilot
study to be classified as either clinical or non-clinical failures.
In addition, the pilot study can help identify potential safety concerns, including condom features that
could cause abrasions or irritation during use. It is recommended that study subjects in the pilot study
undergo a post-coital physical examination as soon after condom use as practicable. Such exams should
be conducted by an experienced clinician.
Investigators should provide detailed verbal and written instructions on appropriate condom insertion
and use to all study participants and demonstrate correct condom placement using a pelvic model.
Collection of user acceptability information will be useful to evaluate product acceptability and to guide
further product improvements prior to the larger clinical investigation.
For additional information, see 6.15 and 6.16.
Annex B contains a sample outline for a pilot clinical study.
6 Clinical validation investigation
6.1 Objectives of clinical validation investigation
The protocol should state the purpose of the study, e.g. to evaluate the performance of a new female
condom (test condom) during vaginal intercourse compared to a control female condom. The protocol
should clearly state the hypothesis being tested (i.e. whether the non-inferiority margin between the
total clinical failure rates for test and control condoms complies with the requirements specified in of
ISO 25841:2014, 8.3).
NOTE Please refer to the WHO guidelines on clinical studies for additional information.
The primary objective of this study is to compare the total clinical failure rates of the test and control
condoms.
Secondary objectives are to evaluate each different type of failure event identified in the risk analysis
(e.g. slippage, breakage, invagination, misdirection, etc.) by comparing the new female condom to the
control female condom for each type of failure event. In addition, there should be an evaluation of total
condom failure (i.e. sum of total clinical and total non-clinical failures).
The secondary objectives of the research should also include safety and acceptability. Safety will be
determined by the proportion of women reporting adverse events reported during condom uses and
by condom type. Acceptability will be measured by the calculated frequency of key acceptability end
points including ease of insertion and removal, like or dislike of product attributes, adequacy and feel of
lubrication, etc.
These studies might also collect incidental data on female condom use during anal sex; however, that is
not the primary objective.
6.2 Outcome measures
The protocol should prospectively state and define the outcome measures to be evaluated when the
study is completed, as well as the means by which such data will be collected.
a) The primary outcome measure is total clinical failure, representing the total number of test or
control condoms for which one or more acute failure events (as defined in Clause 3) are reported by
the users.
b) Secondary outcome measures should include all types of acute failure events, reported individually.
c) Adverse events. The protocol should contain provisions for collecting data on safety outcomes, e.g.
pain, discomfort, bleeding, penile or vaginal irritation, etc.
d) Other outcome measures (optional):
1) any non-clinical failure rates;
2) total failure rate (clinical and non-clinical);
3) user acceptability.
6.3 Study subjects
6.3.1 General
The protocol should describe the exact method(s) of recruiting subjects. Recruitment should attempt
to draw from a representative target population that includes various socio-economic, ethnic, and
4 © ISO 2017 – All rights reserved
cultural, and condom user experience backgrounds. The study should include multiple investigational
sites, and the number of study subjects enrolled should be evenly distributed across sites.
NOTE Selection bias can be introduced into a study by recruiting or oversampling couples who do not
represent the target population. For example, highly experienced condom users (such as commercial sex workers)
might not challenge the condom as much as inexperienced users and so targeting these couples for recruitment
can result in artificially low failure rates.
The various stages and elements of the study are described below. Annex C provides a sample timetable
of events for the individual study subject. It may be configured to the specifics of a given study.
6.3.2 Enrolment of study subjects
6.3.2.1 General
The following inclusion and exclusion criteria are examples for a low risk study. However, other entry
criteria can be used depending on the study context.
6.3.2.2 Inclusion criteria
The following is a list of recommended criteria for selection of study couples:
a) mutually monogamous; current relationship ≥ 3 months;
b) already protected from pregnancy, e.g. oral contraceptive, intrauterine device, subdermal implant,
injectable, patch, male or female sterilization;
c) 18 years to 45 years of age;
d) sexually active, sufficient to meet protocol requirements; agree to have penile-vaginal intercourse
with frequency sufficient to meet protocol requirements;
e) agree to use only study female condoms during time of participation;
f) agree not to use male condom when using female condom in a single sex act;
g) agree not to use drugs or non-study devices that can affect sexual performance;
h) able to understand instructions for correct use of female condoms;
i) no known sexually transmitted infections, including HIV/AIDS;
j) agree to use only lubricant(s) provided by the study;
k) agree not to wear any genital piercing jewellery while using study condoms;
l) willing and capable of following requirements of protocol, including willingness to respond to
questions about reproductive and contraceptive history and use of condoms during interviews and
on self-administered questionnaires;
m) available for follow-up.
If self-administered questionnaires are used in the study, the study subjects should have an adequate
level of literacy commensurate with the questionnaires.
6.3.2.3 Exclusion criteria
The following is a list of recommended criteria for excluding a couple from the study, at the time of
entry or at any time during the study.
If either partner is (or becomes) aware that
a) he/she is allergic or sensitive to the material(s) of the test or control condoms,
b) female partner is pregnant or desires to become so while participating in study,
c) either partner knowingly has a sexually transmitted infection,
d) an itinerant person who might not be able to complete the study, e.g. migrant workers,
e) male partner has known erectile or ejaculatory dysfunction,
f) either partner is using any medications or preparation applied topically or intravaginally to the
genitalia, other than that supplied for the study,
g) either partner is an employee of study sponsor or affiliated with clinical research centre,
it is possible to conduct a condom clinical function study in a population at risk of pregnancy, i.e. not
using a back-up contraceptive. In fact, this might be more representative of the target population in
the commercial market. However, the risk of pregnancy during the study should be considered, as
well as any measures in the protocol to manage that risk. Such a study might be subject to additional
requirements from the local regulatory body.
Commercial sex workers (CSWs) represent an important target population of female condom users.
However, including them in this kind of study poses some unique challenges. While this document does
not specifically recommend excluding CSWs, great care should be taken when considering this during
the study design phase, including provisions to ensure proper steps taken for data collection, as well as
applicability to other target populations.
6.4 Informed consent
The purpose and requirements of the study should be explained before prospective subjects are
presented with the informed consent form. Subjects should also be advised that more detailed
information about sexual activity will be collected than is typical of most family planning visits. Subjects
should be given an opportunity to ask questions about the study and/or the content of the informed
consent. Subjects should provide written informed consent before they are enrolled in the study. All
participants should receive a copy of their signed informed consent form. If the subject recruitment (see
6.3) focuses on monogamous couples, then both partners should be given separate informed consent
forms to sign; if the recruitment focuses on female subjects only, then the male partner(s) do not need
to sign informed consent forms.
Subjects should be informed about the potential for condom failure and the availability of emergency
contraception in the event of condom failure (if not otherwise using a highly effective alternate method
of contraception).
NOTE Useful information regarding informed consent is available in Reference [11]. Also see Reference [12].
6.5 Test and control condoms
6.5.1 General
Both control and test condoms should be tested to establish baseline properties as specified in
ISO 25841. This is important because these results are used to establish or verify the specifications of
the new condom and to verify that the control condom represents typical production. Sufficient sample
sizes should be used.
6 © ISO 2017 – All rights reserved
6.5.2 Test condom
The test condom should continue to meet performance specifications throughout the study.
a) Test condoms used in the clinical study should be manufactured using the same manufacturing
process(es), equipment, specifications, and quality assurance procedures as the eventual product
to be commercially marketed. Recognizing that the scale of manufacture can be different than
normal production runs, the use of pilot manufacturing equipment is acceptable, so long as it is
similar to the equipment to be used during normal production.
b) Test condoms should be selected from a single lot. The compliance of the lot with the specification
should be assessed using the sample plans specified in ISO 25841:2014, Annex B.
If test condoms for the clinical study are selected from more than one lot, then this should be
documented and precautions should be taken to ensure that the individual lots comply with
the specification and are of a similar age and from a similar period of production, e.g. within
three months. It is not acceptable to mix samples drawn from lots produced using significantly
different processes or equipment.
c) As specified in ISO 25841:2014, Clause 9, the airburst properties of test condoms from all lots
(preferably only a single lot) used in the study should be determined using a sample size of at least
2 000 condoms. Other properties of the condom should be determined and recorded by adapting
the principles described in ISO 16037.
d) For the purposes of the trial, the test condoms may be packed in non-standard packaging, i.e.
sequence number and randomization allocation without typical brand. However, the packaging
should provide the same level of protection to the condom as normal production packaging. If non-
standard packaging is used, the manufacturer or the organization responsible for the trial should
ensure that the labelling information specified in ISO 25841:2014, 13.3 is made available to the
study participants.
NOTE Local regulations can require additional labelling.
6.5.3 Control condom
The control condom should continue to meet performance specifications throughout the study.
a) The control condom selected for this study should comply with the requirements in ISO 25841:2014,
Clause 8. Normal production condoms should be used, subject to any special packaging required to
mask the product for the trial.
b) If possible, control condoms should be selected from a single manufacturing lot that is at least
2 years before the expiration date at the commencement of the trial. Quality of the control condoms
should be fully characterized by testing and, if possible, by information from the manufacturer, i.e.
expiry date.
c) Control condoms should be distributed and stored under such conditions that they are protected
from prolonged exposure to temperatures in excess of 32 °C and any other environmental factors
that could affect their quality. Storage conditions should be recorded and fully traceable.
6.5.4 Trial duration exceeds one year
If the duration of the trial exceeds one year (dating from when the condoms were first tested), the study
sponsor should retain samples of both the test and control condoms (per initial sampling plan) and
store them under the same conditions as the trial condoms. The retained samples should be re-tested
at the end of the trial to confirm ongoing compliance with the specifications for airburst properties,
freedom from holes, and any other key condom properties, as established with baseline testing. The
results of any re-tests should be included in the trial report.
Manufacturers may retain additional condom samples and re-test them at regular intervals (e.g. every
six months) during the trial. If the retained samples fail to meet the airburst and freedom from holes’
requirements of ISO 25841, then consideration should be given to terminating the trial.
6.5.5 Sampling of control condoms for bench testing
Sampling plans based on ISO 25841:2014, Annex B, should be used to confirm compliance with
appropriate statistical principles.
6.6 Randomization
Typically, the most efficient design for a condom functionality study, in terms of subjects and condom
numbers, is a randomized, crossover study. With the crossover study design, study subjects are first
given a set of one condom type, use them, and then return for a set of the other condom type. The
protocol should contain a provision for the randomization scheme designating the sequence, e.g. test
condoms first and control condoms second, or the other way around.
6.7 Allocation concealment and study masking
To the degree possible, product assignment should be masked from study couples, investigators and
data analysts after randomization. The study protocol should describe such masking procedures.
6.8 Use of additional lubricant
Lubricant is normally applied to the test and control condom before packaging. However, some test
condoms can require users to apply lubricant. In addition, some users can desire additional lubricant.
The study protocol should address whether additional lubricants can be used with the condoms. The
protocol should also specify the type and amount of lubricant available for the user. In addition, the
case report forms (CRF) should capture the use of any lubricants, including the type, amount (to the
degrees possible), and location applied.
If the lubricant supplied to the study subjects is different from the lubricant applied prior to packaging,
then material screening and testing should be conducted to ensure that any additional lubrication does
not have any deleterious effects on either the test or control condoms.
NOTE It might be possible to adapt the testing principles of ASTM D7661 for testing the effects of lubricant
on condom properties. ASTM D7661 is a test method to assess the compatibility of unlubricated natural rubber
latex male condoms with lubricants.
6.9 Instructions and interactions with study couples
Detailed verbal and written instructions, as well as training, on correct condom use should be
documented in the protocol and provided to all study participants.
The training and instructions should carefully address:
a) purpose of study and duration of participation;
b) clear definitions (with illustrations) of the key outcome measures (acute failure events) that study
participants are expected to report, e.g. breakage, slippage, invagination, misdirection, and any
adverse events (there should be a thorough explanation and demonstration of each type of acute
failure event, preferably using a pelvic model);
c) correct condom use;
d) time frames for using test and control condoms and recording data;
e) careful review of the “individual condom use” CRF and any other CRFs, with instructions on how to
properly complete them;
8 © ISO 2017 – All rights reserved
f) telephone and/or other contact information for study coordinator.
In addition, couples should be instructed to contact research staff immediately if they encounter any
problems related to the study. Serious adverse reactions should be reported immediately to the study
sponsor and the ethics committee.
6.10 Interviews and data collection
6.10.1 Schedule for interviews and condom distribution
The protocol should have a schedule for:
a) enrolment interview:
— questionnaire, enrolment including training on device use and different types of failure events;
— provide condoms and condom use CRFs
b) mid-study interview, if crossover design:
— collect condom use forms from first set, any unused condoms;
— provide second set of condoms and individual condom use CRFs;
NOTE If three different types of condoms are being tested (i.e. for a three-arm study), collect CRFs for
the second set and any unused condoms. Provide a third set of condoms and individual condom use CRFs.
c) exit interview:
— collect condom use forms from the second (or third) set, any unused condoms.
For the purpose of this document, CRFs might be paper-based or electronic. Examples of CRFs are
provided in the annexes.
6.10.2 Enrolment interview
The protocol should have provisions for an initial interview for obtaining informed consent from both
partners, ensuring that inclusion/exclusion criteria are met, and to provide study participants with
instructions and initial set of condoms.
There should be an Enrolment CRF to collect data on the study participant:
a) age, condom experience, reproductive history and other demographic information;
b) risk of STI and pregnancy;
c) method of contraception used during study;
d) ability to complete the study protocol (e.g. length of relationship, frequency of intercourse,
problems with erection/ejaculation, use of genital jewellery, etc.);
e) others, e.g. data on circumcision, genital mutilation (modification), as appropriate.
If desired, the protocol might contain provisions for a penis measurement kit. The kit should allow for
a consistent means of measuring erect penis length and circumference. This information should be
turned in to the investigator at a later visit.
Annex D is a sample form for initial entry into the study (study entry CRF).
6.10.3 Individual condom use CRF
Per the randomization scheme, the protocol should contain a provision for providing the designated
number of condoms (test or control) to the participating couples together with sufficient number of
individual condom use CRFs for self-reports of acute failure events and other information.
Clinical function studies of condoms are heavily reliant on user reports and memory recall. To minimize
the impact of recall bias, it is recommended that a limited number of condoms (e.g. five) of each type be
used in less than a two-week to three-week time period. Study instructions should direct participating
couples to complete the CRF for individual condom use as soon as possible after each sex act. To
reduce memory recall bias, every effort should be made to minimize the time between the sex act and
completion of the CRF, i.e. no more than a few hours.
The individual condom use CRF should provide for entries to collect the following even
...


Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...