ISO/TR 24971:2020
(Main)Medical devices — Guidance on the application of ISO 14971
Medical devices — Guidance on the application of ISO 14971
This document provides guidance on the development, implementation and maintenance of a risk management system for medical devices according to ISO 14971:2019. The risk management process can be part of a quality management system, for example one that is based on ISO 13485:2016[24], but this is not required by ISO 14971:2019. Some requirements in ISO 13485:2016 (Clause 7 on product realization and 8.2.1 on feedback during monitoring and measurement) are related to risk management and can be fulfilled by applying ISO 14971:2019. See also the ISO Handbook: ISO 13485:2016 — Medical devices — A practical guide[25].
Dispositifs médicaux — Recommandations relatives à l'application de l'ISO 14971
Le présent document fournit des recommandations relatives au développement, à la mise en œuvre et à la tenue à jour d'un système de gestion des risques pour les dispositifs médicaux conformément à l'ISO 14971:2019. Le processus de gestion des risques peut faire partie d'un système de management de la qualité qui s'appuie, par exemple, sur l'ISO 13485:2016[24], mais cela n'est pas requis par l'ISO 14971:2019. Certaines exigences de l'ISO 13485:2016 (Article 7 relatif à la réalisation du produit et 8.2.1[eXtyles1] relatives aux retours d'information au cours de la surveillance et du mesurage) portent sur la gestion des risques et peuvent être satisfaites en appliquant l'ISO 14971:2019. Voir également le manuel ISO: ISO 13485:2016 — Medical devices — A practical guide[25]. [eXtyles1]No section matches the in-text citation "8.2.1". Please supply the missing section or delete the citation.
General Information
- Status
- Published
- Publication Date
- 15-Jun-2020
- Current Stage
- 6060 - International Standard published
- Start Date
- 16-Jun-2020
- Completion Date
- 16-Jun-2020
Relations
- Consolidates
CEN ISO/TR 24971:2020 - Medical devices - Guidance on the application of ISO 14971 (ISO/TR 24971:2020) - Effective Date
- 12-Feb-2026
- Effective Date
- 06-Jun-2022
- Effective Date
- 02-Sep-2017
- Effective Date
- 02-Sep-2017
Overview
ISO/TR 24971:2020 - "Medical devices - Guidance on the application of ISO 14971" is a technical report that provides practical guidance for the development, implementation and maintenance of a medical device risk management system in accordance with ISO 14971:2019. It clarifies concepts, illustrates risk management tasks and expands on topics such as hazard identification, risk estimation, risk control, and evaluation of overall residual risk. The guidance can be used within a standalone risk management system or as part of a quality management system (for example one based on ISO 13485:2016).
Key topics and technical requirements
- Risk management process: guidance on planning, responsibilities, competence, risk management file and review activities.
- Risk analysis: identification of intended use, reasonably foreseeable misuse, characteristics related to safety, and techniques for hazard identification.
- Risk estimation and assessment: advice on probability, severity, and handling risks when probability cannot be reliably estimated.
- Risk control: option analysis, design and manufacturing controls, implementation and verification of controls, and completeness of risk control measures.
- Benefit‑risk analysis: methods and criteria for comparing benefits against residual risks.
- Information for safety vs. disclosure of residual risk: how to document user information and label warnings versus residual risk reporting.
- Evaluation of overall residual risk: inputs, possible approaches and management review.
- Production and post‑production activities: surveillance, information collection and feedback loop for continuous risk control.
- Special topics in annexes: use of international standards in risk management, security-related risks, in vitro diagnostic (IVD) guidance, and techniques supporting risk analysis.
Practical applications
ISO/TR 24971:2020 is used to:
- Implement and document a compliant risk management system aligned with ISO 14971 requirements.
- Inform design decisions, verification/validation activities and risk control selection.
- Support regulatory submissions and audits by providing structured approaches to hazard identification, residual risk evaluation and post‑market surveillance.
- Integrate risk activities with quality systems (e.g., ISO 13485) and manufacturing processes.
Who should use this standard
- Medical device manufacturers (design, development and manufacturing teams)
- Risk managers and safety engineers
- Quality and regulatory affairs professionals preparing technical files and compliance evidence
- Auditors, notified bodies and conformity assessment personnel assessing risk management practices
Related standards
- ISO 14971:2019 - the primary standard for medical device risk management
- ISO 13485:2016 - quality management for medical devices (cross-references in the TR)
- Developed jointly with IEC technical committees (see foreword for IEC/SC 62A liaison)
Keywords: ISO/TR 24971:2020, ISO 14971 guidance, risk management for medical devices, residual risk evaluation, benefit-risk analysis, medical device safety.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
ISO/TR 24971:2020 is a technical report published by the International Organization for Standardization (ISO). Its full title is "Medical devices — Guidance on the application of ISO 14971". This standard covers: This document provides guidance on the development, implementation and maintenance of a risk management system for medical devices according to ISO 14971:2019. The risk management process can be part of a quality management system, for example one that is based on ISO 13485:2016[24], but this is not required by ISO 14971:2019. Some requirements in ISO 13485:2016 (Clause 7 on product realization and 8.2.1 on feedback during monitoring and measurement) are related to risk management and can be fulfilled by applying ISO 14971:2019. See also the ISO Handbook: ISO 13485:2016 — Medical devices — A practical guide[25].
This document provides guidance on the development, implementation and maintenance of a risk management system for medical devices according to ISO 14971:2019. The risk management process can be part of a quality management system, for example one that is based on ISO 13485:2016[24], but this is not required by ISO 14971:2019. Some requirements in ISO 13485:2016 (Clause 7 on product realization and 8.2.1 on feedback during monitoring and measurement) are related to risk management and can be fulfilled by applying ISO 14971:2019. See also the ISO Handbook: ISO 13485:2016 — Medical devices — A practical guide[25].
ISO/TR 24971:2020 is classified under the following ICS (International Classification for Standards) categories: 11.040.01 - Medical equipment in general. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO/TR 24971:2020 has the following relationships with other standards: It is inter standard links to CEN ISO/TR 24971:2020, ISO 20618:2015, ISO 14971:2007, ISO/TR 24971:2013. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
ISO/TR 24971:2020 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
TECHNICAL ISO/TR
REPORT 24971
Redline version
compares Second edition to
First edition
Medical devices — Guidance on the
application of ISO 14971
Dispositifs médicaux — Recommandations relatives à l'application
de l'ISO 14971
Reference number
ISO/TR 24971:redline:2020(E)
©
ISO 2020
ISO/TR 24971:redline:2020(E)
IMPORTANT
This marked-up version uses the following colour-coding in the marked-up text:
Text example 1 — Text has been added (in green)
— Text has been deleted (in red)
Text example 2
— Graphic figure has been added
— Graphic figure has been deleted
1.x . — If there are changes in a clause/subclause, the corresponding clause/
subclause number is highlighted in yellow in the Table of contents
DISCLAIMER
This marked-up version highlights the main changes in this edition of the document
compared with the previous edition. It does not focus on details (e.g. changes in
punctuation).
This marked-up version does not constitute the official ISO document and is not intended to
be used for implementation purposes.
© ISO 2020
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting
on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address
below or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Fax: +41 22 749 09 47
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii © ISO 2020 – All rights reserved
ISO/TR 24971:redline:2020(E)
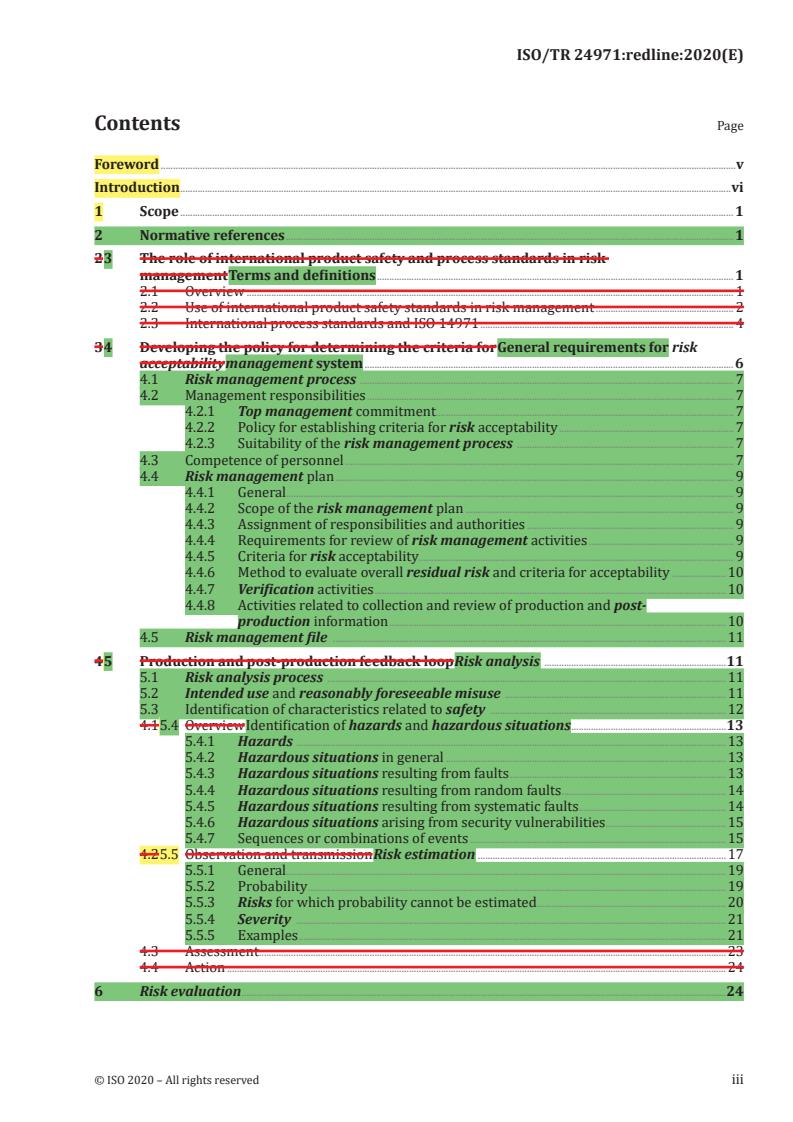
Contents Page
Foreword .v
Introduction .vi
1 Scope . 1
2 Normative references . 1
2 3 The role of international product safety and process standards in risk
management Terms and definitions . 1
2.1 Overview . 1
2.2 Use of international product safety standards in risk management . 2
2.3 International process standards and ISO 14971 . 4
3 4 Developing the policy for determining the criteria for General requirements for risk
acceptability management system . 6
4.1 Risk management process . 7
4.2 Management responsibilities . 7
4.2.1 Top management commitment . 7
4.2.2 Policy for establishing criteria for risk acceptability . 7
4.2.3 Suitability of the risk management process . 7
4.3 Competence of personnel . 7
4.4 Risk management plan . 9
4.4.1 General. 9
4.4.2 Scope of the risk management plan . 9
4.4.3 Assignment of responsibilities and authorities . 9
4.4.4 Requirements for review of risk management activities . 9
4.4.5 Criteria for risk acceptability . 9
4.4.6 Method to evaluate overall residual risk and criteria for acceptability .10
4.4.7 Verification activities .10
4.4.8 Activities related to collection and review of production and post-
production information .10
4.5 Risk management file .11
4 5 Production and post-production feedback loop Risk analysis .11
5.1 Risk analysis process .11
5.2 Intended use and reasonably foreseeable misuse .11
5.3 Identification of characteristics related to safety .12
4.1 5.4 Overview Identification of hazards and hazardous situations .13
5.4.1 Hazards .13
5.4.2 Hazardous situations in general .13
5.4.3 Hazardous situations resulting from faults .13
5.4.4 Hazardous situations resulting from random faults .14
5.4.5 Hazardous situations resulting from systematic faults .14
5.4.6 Hazardous situations arising from security vulnerabilities .15
5.4.7 Sequences or combinations of events .15
4.2 5.5 Observation and transmission Risk estimation .17
5.5.1 General.19
5.5.2 Probability .19
5.5.3 Risks for which probability cannot be estimated .20
5.5.4 Severity .21
5.5.5 Examples .21
4.3 Assessment .23
4.4 Action .24
6 Risk evaluation .24
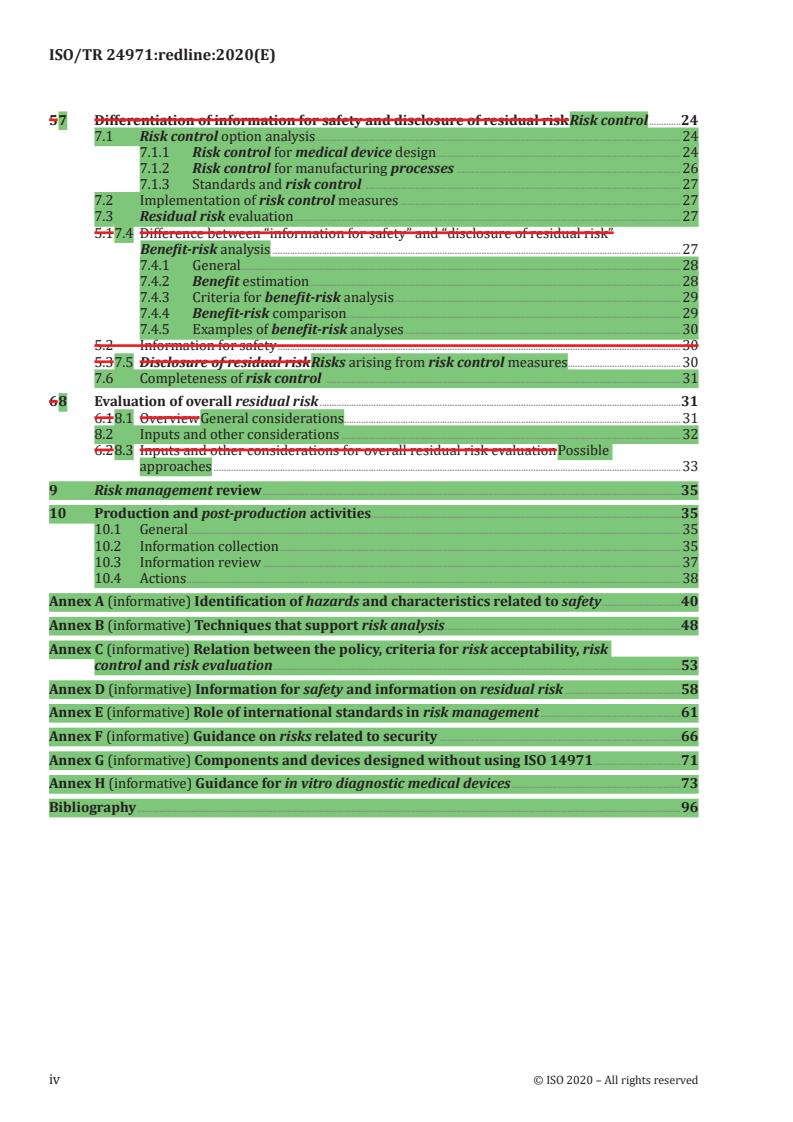
ISO/TR 24971:redline:2020(E)
5 7 Differentiation of information for safety and disclosure of residual risk Risk control .24
7.1 Risk control option analysis .24
7.1.1 Risk control for medical device design .24
7.1.2 Risk control for manufacturing processes .26
7.1.3 Standards and risk control .27
7.2 Implementation of risk control measures .27
7.3 Residual risk evaluation .27
5.1 7.4 Difference between “information for safety” and “disclosure of residual risk”
Benefit-risk analysis .27
7.4.1 General.28
7.4.2 Benefit estimation .28
7.4.3 Criteria for benefit-risk analysis .29
7.4.4 Benefit-risk comparison.29
7.4.5 Examples of benefit-risk analyses .30
5.2 Information for safety .30
5.3 7.5 Disclosure of residual risk Risks arising from risk control measures .30
7.6 Completeness of risk control .31
6 8 Evaluation of overall residual risk .31
6.1 8.1 Overview General considerations.31
8.2 Inputs and other considerations .32
6.2 8.3 Inputs and other considerations for overall residual risk evaluation Possible
approaches .33
9 Risk management review .35
10 Production and post-production activities.35
10.1 General .35
10.2 Information collection .35
10.3 Information review .37
10.4 Actions .38
Annex A (informative) Identification of hazards and characteristics related to safety .40
Annex B (informative) Techniques that support risk analysis .48
Annex C (informative) Relation between the policy, criteria for risk acceptability, risk
control and risk evaluation .53
Annex D (informative) Information for safety and information on residual risk .58
Annex E (informative) Role of international standards in risk management .61
Annex F (informative) Guidance on risks related to security .66
Annex G (informative) Components and devices designed without using ISO 14971 .71
Annex H (informative) Guidance for in vitro diagnostic medical devices .73
Bibliography .96
iv © ISO 2020 – All rights reserved
ISO/TR 24971:redline:2020(E)
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2. (see www .iso .org/ directiveswww .iso .org/ directives
-and -policies).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received. (see www .iso .org/ patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation on the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO’s adherence to the
World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT), see the following
URL: www .iso .org/ iso/ foreword .html.
ISO/TR 24971This document was prepared jointly by Technical Committee ISO/TC 210,
Quality management and corresponding general aspects for medical devices, and Technical
CommitteeSubcommittee IEC/SC 62A, Common aspects of electrical equipment used in medical practice.
The draft was circulated for voting to the national bodies of both ISO and IEC.
This second edition cancels and replaces the first edition, which has been technically revised. The main
changes compared to the previous edition are as follows:
— The clauses of ISO/TR 24971:2013 and some informative annexes of ISO 14971:2007 are merged,
restructured, technically revised, and supplemented with additional guidance.
— To facilitate the use of this document, the same structure and numbering of clauses and subclauses
as in ISO 14971:2019 is employed. The informative annexes contain additional guidance on specific
aspects of risk management.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www .iso .org/ members .html.
ISO/TR 24971:redline:2020(E)
Introduction
Experience indicates thatThis document provides guidance to assist manufacturers have difficulty
with practical implementation of some clauses of the in the development, implementation and
maintenance of a risk management International Standard, process for medical devices that aims to meet
the requirements of ISO 14971:20072019, Medical devices — Application of risk management to medical
devices. This Technical Report provides guidance to assist in the development, implementation and
maintenance of risk management for medical devices that aim to meet the requirements of It provides
guidance on the application of ISO 14971:2019. It provides guidance for specific aspects of for ISO 14971
for a wide variety of medical devices. These medical devices include active, non-active, implantable, and
non-implantable medical devices, software as medical devices and in vitro diagnostic medical devices.
This Technical Report is not intended to be an overall guidance document on the implementationThe
clauses and subclauses in this document have the same structure and numbering as the clauses
and subclauses of ISO 14971:2019 for organizations. It supplements the guidance contained in the
informative annexes, to facilitate the use of this guidance in applying the requirements of the standard.
Further division into subclauses is applied where considered useful. The informative annexes contain
additional guidance on specific aspects of risk management. The guidance consists of the clauses
of ISO 14971/TR 24971:2013 related to the following areasand some of the informative annexes of
ISO 14971:2007, which are merged, restructured, technically revised, and supplemented with additional
guidance.
— Guidance on the role of international product safety and process standards in risk management
— Guidance on developing the policy for determining the criteria for risk acceptability
— Guidance on how the production and post-production feedback loop can work
— Guidance on the differentiation of information for safety as a risk control measure and disclosure of
residual risk
— Guidance on the evaluation of overall residual risk
Annex H was prepared in cooperation with Technical Committee ISO/TC 212, Clinical laboratory testing
and in vitro diagnostic test systems.
This Technical Report provides somedocument describes approaches that manufacturersan organization
can use to develop, implement and maintain some aspects of a risk management process system that
conformsconforming to ISO 14971:2019. Alternative approaches can be used if thesealso satisfy the
requirements of ISO 14971:2019.
When judging the applicability of the guidance in this Technical Reportdocument, one should consider
the nature of the medical device(s) to which it will apply, the risks associated with the use ofhow and by
whom these medical devices are used, and the applicable regulatory requirements.
vi © ISO 2020 – All rights reserved
TECHNICAL REPORT ISO/TR 24971:redline:2020(E)
Medical devices — Guidance on the application of ISO 14971
1 Scope
This Technical Report provides guidance in addressing specific areasdocument provides guidance on
the development, implementation and maintenance of ISO 14971 when implementing risk managementa
risk management system for medical devices according to ISO 14971:2019.
The risk management processguidance is intended can be part of a quality management system, for
[24]
example one that is based on ISO 13485:2016 , but this is not required by ISO 14971:2019. Some
requirements in ISO 13485:2016 (Clause 7 on product realization and 8.2.1 on feedback during
monitoring and measurement) are related to risk managementassist manufacturers and other
users of and the standard tocan be fulfilled by applying ISO 14971:2019. See also the ISO Handbook:
[25]
ISO 13485:2016 — Medical devices — A practical guide .
— understand the role of international product safety and process standards in risk management;
— develop the policy for determining the criteria for risk acceptability;
— incorporate production and post-production feedback loop into risk management;
— differentiate between “information for safety” and “disclosure of residual risk”; and
— evaluate overall residual risk.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 14971:2019, Medical devices — Application of risk management to medical devices
2 3 The role of international product safety and process standards in risk
management Terms and definitions
2.1 Overview
International product safety and process standards play a significant role in risk management as
described by ISO 14971. In principle, these standards are developed using a type of risk management
that can include identifying hazards and hazardous situations, estimating risks, evaluating risks,
and specifying risk control measures. More information on a process for developing medical device
standards using a type of risk management can be found in documents such as ISO/IEC Guide 51 and
ISO/IEC Guide 63. International product safety and process standards are developed by experts in the
field and represent the generally accepted state of the art (see D.4 of ISO 14971:2007).
These standards can have an important role in risk management. When performing risk management,
the manufacturer first needs to consider the medical device being designed, its intended use and the
hazards/hazardous situations related to it. Manufacturers can, if they choose, identify standard(s)
that contain specific requirements that help manage the risks related to those hazards/hazardous
situations.
For medical devices that satisfy the requirements and compliance criteria of these standards, the
residual risks related to those hazards/hazardous situations can be considered acceptable unless there
ISO/TR 24971:redline:2020(E)
is objective evidence to the contrary. Some potential sources of objective evidence to the contrary can
include reports of adverse events, product recalls and complaints. The requirements of International
Standards, such as engineering or analytical processes, specific output limits, warning statements, or
design specifications, can be considered risk control measures established by the standards writers
that are intended to address the risks of specific hazardous situations that have been identified and
evaluated as needing risk control.
In many cases, the standards writers have taken on and completed elements of risk management
and provided manufacturers with answers in the form of design requirements and test methods for
establishing conformity. When performing risk management activities, manufacturers can take
advantage of the work of the standards writers and need not repeat the analyses leading to the
requirements of the standard. International standards, therefore, provide valuable information on risk
acceptability that has been validated during a worldwide evaluation process, including multiple rounds
of review, comment, and voting.
2.2 Use of international product safety standards in risk management
An international product safety standard can establish requirements that, when implemented, result in
acceptable risk for specific hazardous situations (e.g. safety limits). The manufacturer can apply these
requirements in the following way when managing risk.
a) Where an international product safety standard specifies technical requirements addressing
particular hazards or hazardous situations, together with specific acceptance criteria, compliance
with those requirements is presumed to establish that the residual risks have been reduced to
acceptable levels unless there is objective evidence to the contrary. For example, in IEC 60601-
1, Medical electrical equipment — Part 1: General requirements for basic safety and essential
performance, leakage current must be controlled to achieve an acceptable level of risk. IEC 60601-1
provides leakage current limits that are considered to result in an acceptable level of risk when
measured under the conditions stated in 8.7 of IEC 60601-1:2005. For this example, further risk
management would not be necessary. The following steps need to be taken in this case.
1) Implement 4.2 and 4.3 of ISO 14971:2007 to identify characteristics related to safety and
identify hazards and hazardous situations associated with the device as completely as possible.
2) Identify those hazards and hazardous situations relevant to the particular medical device that
are exactly covered by the international product safety standard.
3) For those identified hazards and hazardous situations exactly covered by the international
product safety standard, the manufacturer may choose not to estimate (4.4 of ISO 14971:2007)
or evaluate (Clause 5 of ISO 14971:2007) the risks so identified but rather rely on the
requirements contained in the international standard to demonstrate the completion of risk
estimation and risk evaluation.
4) To the extent possible, the manufacturer should identify the design specifications that satisfy
the requirements in the standard and serve as risk control measures (6.2 of ISO 14971:2007).
NOTE For some international product safety standards, the possibility of identifying all the specific
risk control measures is limited. One example is electromagnetic compatibility testing in IEC 60601–1-2,
Medical electrical equipment — Part 1-2: General requirements for basic safety and essential performance
— Collateral standard: Electromagnetic compatibility — Requirements and tests, for complex medical
devices.
5) Verification of the implementation of the risk control measures for these hazardous situations
is obtained from the design documents. Verification of the effectiveness of the risk control
measures is obtained from the tests and test results demonstrating that the device meets the
relevant requirements of the international product safety standard.
6) If the relevant requirements are met, the associated residual risk is considered acceptable.
b) Where an international product safety standard does not completely specify technical requirements
and associated tests and test acceptance criteria, the situation is more complex. In some cases, the
2 © ISO 2020 – All rights reserved
ISO/TR 24971:redline:2020(E)
standard directs the manufacturer to perform specific tests related to known hazards or hazardous
situations but does not provide specific test acceptance criteria (e.g. IEC 60601-2-16, Medical
electrical equipment — Part 2-16: Particular requirements for basic safety and essential performance of
haemodialysis, haemodiafiltration and haemofiltration equipment). In some other cases, the standard
can simply direct the manufacturer to investigate specific hazards or hazardous situations in
their risk analysis (e.g. 10.2 of IEC 60601-1:2005). The range of alternatives is too large to provide
specific guidance on how to use such standards in the risk management process. Manufacturers
are encouraged, however, to use the content of such standards in their risk management of the
particular medical device.
c) For hazards or hazardous situations that are identified for the particular medical device but are
not specifically addressed in any standard, the manufacturer needs to address those hazards or
hazardous situations in the risk management process. The manufacturer is required to estimate
and evaluate the risks and, if necessary, control these risks (see 4.4 and Clauses 5 and 6 of
ISO 14971:2007).
See Figure 1 for a flowchart and an example outlining the use of international product safety standards.
Identify Hazards/Hazardous situations Hazardous situation identi€ied: patient (and medical device)
(H/HS)
needs to be transfered from one room to another; if put in
(4.3 of ISO 14971:2007).
transport position, equipment overbalances and patient falls
2 c) Input the identi€ied Are the H/HS
hazards and hazardous addressed in international
No Yes: IEC 60601-1:2005, Subclause 9.4.2.1
situations into the risk product safety
management process. standard(s)?
Yes
2 b) Use the identi€ied hazards,
hazardous situations, test How is it
methods, or other relevant 2 b) addressed? Choose between 2 a)
information in the risk 2 a) and 2 b).
management process.
2 a)
Yes: there is a speci€ied requirement:
2 a): International product
The equipment shall not overbalance when placed in any
safety standard speci€ies
transport position of normal use on a plane inclined at an angle
requirements and provides
of 10° from the horizontal plane, and speci€ic acceptance criteria
speci€ic test acceptance
(de€ined test). If the equipment overbalances, it does not comply
criteria.
with the requirement.
Use the identi€ied hazards,
Do
hazardous situations, test
requirement(s) fully match Yes, equipment is transportable, and it can be transported with
methods, or other relevant No
the design including the patient on it to accommodate patient transfers.
information in the risk
intended use?
management process.
Yes
No need to estimate (4.4) Risk is not estimated nor evaluated prior to implementation of
or evaluate risk (5) risk control measure.
Identify the design
speci€ications that achieve
Identi€ied in the risk management €ile
the requirement in the
standard (6.2).
Verify the effectiveness Test performed: equipment placed on a plane inclined at an
(6.3) by performing test(s) angle 10º from the horizontal plane. Result: medical device does
according to the standard. not overbalance
If the test is passed,
related residual risks Medical device does not overbalance, so the related residual risk
are considered is considered acceptable.
acceptable (6.4).
Figure 1 — Use of international product safety standards and example of such standard that
specifies requirements and provides specific test acceptance criteria
ISO/TR 24971:redline:2020(E)
2.3 International process standards and ISO 14971
International process standards, as shown in the examples below, can often be used in conjunction with
ISO 14971. This is performed in one of two ways:
— The international process standard requires application of ISO 14971 as part of the implementation
of the international process standard, e.g. IEC 62304 on software life cycle processes; or
— The international process standard is intended to be used in risk management, e.g. IEC 62366 on
usability engineering and the ISO 10993 series on biological evaluation.
In either case, proper use of the international process standard requires attention to the interfaces
between that standard and ISO 14971 in order to achieve acceptable levels of risk for the medical device.
The two standards should work together such that inputs, outputs and their timing are optimized.
Three examples are given below to demonstrate this ideal situation.
a) IEC 62304, Medical device software — Software life cycle processes
The relationship between IEC 62304 and ISO 14971 is well-described in the introduction to IEC 62304:
As a basic foundation it is assumed that medical device software is developed and maintained within
a quality management system (see 4.1 of IEC 62304:2006) and a risk management process (see
4.2 of IEC 62304:2006). The risk management process is already very well addressed by the
International Standard ISO 14971. Therefore IEC 62304 makes use of this advantage simply by a
normative reference to ISO 14971. Some minor additional risk management requirements are
needed for software, especially in the area of identification of contributing software factors related
to hazards. These requirements are summarized and captured in Clause 7 of IEC 62304:2006 as
the software risk management process.
Whether software is a contributing factor to a hazard is determined during the hazard identification
activity of the risk management process. hazards that could be indirectly caused by software
(for example, by providing misleading information that could cause inappropriate treatment to be
administered) need to be considered when determining whether software is a contributing factor.
The decision to use software to control risk is made during the risk control activity of the risk
management process. The software risk management process required in this standard has to
be embedded in the device risk management process according to ISO 14971.
IEC 62304 makes a normative reference to ISO 14971 and specifically requires:
— software development planning (5.1 of IEC 62304:2006) that is consistent with the risk
management plan required by ISO 14971; and
— a software risk management process (Clause 7 of IEC 62304:2006) based upon ISO 14971.
b) IEC 62366, Medical devices — Application of usability engineering to medical devices
The flow diagram in Figure A.1 of IEC 62366:2007 demonstrates the relationship and interconnection
of the two parallel and interconnecting processes. In addition to making a normative reference to
ISO 14971, IEC 62366:2007 identifies three specific clauses where the usability engineering process
can supplement and interact with risk management as described in ISO 14971:
— 5.3.1 of IEC 62366:2007 requires: “An identification of characteristics related to safety (part
of a risk analysis) that focuses on usability shall be performed according to ISO 14971:2007,
4.2.”
— 5.3.2 of IEC 62366:2007 requires: “The manufacturer shall identify known or foreseeable
hazards (part of a risk analysis) related to usability according to ISO 14971:2007, 4.3.”
— 5.9 of IEC 62366:2007 on Usability Validation makes several references to activities that would
be undertaken as part of risk management.
4 © ISO 2020 – All rights reserved
ISO/TR 24971:redline:2020(E)
c) ISO 10993 (all parts), Biological evaluation of medical devices
The introduction to ISO 10993-1 states that ISO 10993-1 is intended to be a guidance document for the
biological evaluation of medical devices within risk management, as part of the overall evaluation
and development of each device.
Annex B of ISO 10993-1:2009 applies ISO 14971 to provide guidance on the risk management approach
for identification of biological hazards associated with medical devices, estimation and evaluation
of the risks, control of the risks, and monitoring the effectiveness of the risk control measures.
This approach combines the review and evaluation of existing data from all sources, with the selection
and application of additional tests (where necessary), thus enabling a full evaluation to be made of
the biological responses to each medical device, relevant to its safety in use.
ISO 10993-1:2009 aligns itself explicitly within risk management as described in ISO 14971.
The biological evaluation should be conducted in a manner similar to that used for other product risks,
and should include:
— Risk analysis (What are the hazards and associated risks?)
— Risk evaluation (Are they acceptable?)
— Risk control (How will they be controlled?)
— Overall residual risk/benefit evaluation
Following the processes defined in ISO 14971, if the overall residual risk evaluation concludes from
existing data that the identified risks are acceptable, no further risk control is needed. Otherwise,
appropriate measures should be taken to further evaluate or mitigate the risks.
The output of this evaluation is a Biological Evaluation Report.
Application
— Conditions identified as hazards in ISO 10993-1 include:
— Acute toxicity
— Chronic toxicity
— Irritation (skin, eye, mucosal surfaces)
— Hypersensitivity
— Genotoxicity
— Carcinogenicity
— Do the proposed materials in the particular medical device cause such conditions?
Methods that are used to determine if a material in the particular medical device can result in
the conditions listed above include:
— Chemical characterization and assessment
— Literature review
— Testing (in vitro/in vivo, non-clinical)
— Field experience
ISO/TR 24971:redline:2020(E)
— Are the exposure levels acceptable?
According to ISO 10993-1, expert assessors should determine if the available information/data are
sufficient to determine if the overall residual risk associated with biological hazards is acceptable.
This conclusion is documented in the Biological Evaluation Report, which becomes an element of
the risk management file.
For the purposes of this document, the terms and definitions given in ISO 14971:2019 apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at http:// www .electropedia .org/
[20]
NOTE The defined terms in ISO 14971:2019 are derived as much as possible from ISO/IEC Guide 63:2019
which was developed specifically for the medical device sector.
3 4 Developing the policy for determining the criteria for General requirements
for risk acceptability management system
According to 3.2 of ISO 14971:2007, top management is required to define and document the policy for
determining the criteria for risk acceptability. This policy is intended to ensure that criteria:
a) are based upon applicable national or regional regulations;
b) are based upon relevant International Standards;
c) take into account available information such as the generally accepted state of the art and known
stakeholder concerns.
NOTE Other relevant information can also be included.
The policy could cover the entire range of a manufacturer's medical devices or it can take different
forms depending on whether the medical devices are similar to each other, or whether the differences
between groups of medical devices are significant.
When developing or maintaining the policy the following should be taken into consideration:
— The applicable regulatory requirements in the regions where the medical device is to be marketed.
— The relevant International Standards for the particular medical device or an intended use of the
medical device that can help identify principles for setting the criteria for risk acceptability (see 2.2).
— Information on the state of the art can be obtained from review of the literature and other
information on similar medical devices the manufacturer has marketed, as well as those from
competing companies.
— The validated and comprehensive concerns from the main stakeholders. Some potential sources of
information on the patient and clinician perspective can include news media, social media, patient
forums, as well as input from internal departments with expert knowledge of stakeholder concerns
such as the clinical department.
The manufacturer should provide guidelines for developing the actual criteria for risk acceptability to
be used in the risk management plan for the particular medical device being considered (see 3.4 of
ISO 14971:2007).
The review of the suitability of the risk management process at planned intervals, as required by 3.2 of
ISO 14971:2007, can demonstrate the appropriateness of previously used criteria for risk acceptability
or lead to changes in the policy. Such changes can also lead to reviewing the appropriateness of previous
risk acceptability decisions.
6 © ISO 2020 – All rights reserved
ISO/TR 24971:redline:2020(E)
4.1 Risk management process
ISO 14971:2019requires that the manufacturer establishes, implements, documents and maintains an
ongoing risk management process throughout the life cycle of the medical device. The required elements
in this process and the responsibilities of top management are given in ISO 14971:2019 and explained in
further detail in this document.
4.2 Management responsibilities
4.2.1 Top management commitment
Top management has the responsibility to establish and maintain an effective risk management process.
It is important to note the emphasis on top management in ISO 14971:2019 Top management has the
power to assign authorities and responsibilities, to set priorities and to provide resources within the
organization. Commitment at the highest level of the organization is essential for the risk management
process to be effective.
If the manufacturer’s organization consists of separate entities, for example business units or divisions,
then top management can refer to those individuals who direct and control the entity implementing the
risk management process. Each entity can have its own risk management process (and its own quality
management system).
4.2.2 Policy for establishing cri
...
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...