CEN/TS 17688-3:2021
(Main)Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for Fine Needle Aspirates (FNAs) - Part 3: Isolated genomic DNA
Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for Fine Needle Aspirates (FNAs) - Part 3: Isolated genomic DNA
This document gives guidelines on the handling, documentation, storage and processing of fine needle aspirates (FNAs) intended for gDNA examination during the pre-examination phase before a molecular examination is performed.
This document is applicable to molecular in vitro diagnostic examinations including laboratory developed tests performed by medical laboratories and molecular pathology laboratories that examine gDNA isolated from FNAs. It is also intended to be used by laboratory customers, in vitro diagnostics developers and manufacturers, biobanks, institutions and commercial organisations performing biomedical research, and regulatory authorities.
Different dedicated measures are taken for collecting, stabilizing, transporting and storing of core needle biopsies (FNA Biopsy or FNA B) and are not covered in this document, but EN ISO 20184-3, Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for frozen tissue - Part 3: Isolated DNA and EN ISO 20166-3, Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for formalin-fixed and paraffin-embedded (FFPE) tissue - Part 3: Isolated DNA.
This document is not applicable for pathogen DNA examination and gDNA examination by in situ detection.
NOTE International, national or regional regulations or requirements can also apply to specific topics covered in this document.
Molekularanalytische in‐vitro‐diagnostische Verfahren - Spezifikationen für präanalytische Prozesse für Feinnadelaspirate - Teil 3: Isolierte genomische DNA
Dieses Dokument enthält Leitlinien zur Handhabung, Dokumentation, Lagerung und Verarbeitung von Feinnadelaspiraten (FNAs) zur gDNA Untersuchung während der präanalytischen Phase vor Beginn der molekularen Analyse.
Dieses Dokument gilt für molekulare in vitro-diagnostische Untersuchungen, wozu auch laboreigene Prüfungen zählen, die von medizinischen Laboratorien und Laboratorien der molekularen Pathologie zur Untersuchung der aus FNAs isolierten gDNA durchgeführt werden. Es soll auch von Laborkunden, Entwicklern und Herstellern von In vitro-Diagnostika, Biobanken, Einrichtungen und kommerziellen Organisationen, die in der biomedizinischen Forschung tätig sind, sowie Aufsichtsbehörden eingesetzt werden.
Für die Entnahme, die Stabilisierung, den Transport und die Lagerung von Stanzbiopsien (FNA Biopsie oder FNA B) werden verschiedene spezielle Maßnahmen ergriffen, die nicht in diesem Dokument, sondern in EN ISO 20184 3 Molekularanalytische in vitro-diagnostische Verfahren — Spezifikationen für präanalytische Prozesse für gefrorene Gewebeproben — Teil 3: Isolierte DNA und EN ISO 20166 3 Molekularanalytische in vitro-diagnostische Verfahren — Spezifikationen für präanalytische Prozesse für formalinfixierte und paraffineingebettete (FFPE)-Gewebeproben — Teil 3: Isolierte DNA behandelt werden.
Dieses Dokument findet keine Anwendung auf Untersuchungen pathogener DNA und gDNA Untersuchungen durch In situ-Nachweis.
ANMERKUNG Zu bestimmten Bereichen, die in diesem Dokument behandelt werden, können auch internationale, nationale oder regionale Bestimmungen oder Anforderungen gelten.
Analyses moléculaires de diagnostic in vitro - Spécifications pour les processus préanalytiques pour les ponctions à l'aiguille fine - Partie 3: ADN génomique isolé
Molekularne diagnostične preiskave in vitro - Specifikacije za predpreiskovalne procese pri aspiraciji s tanko iglo (FNA) - 3. del: Iz genoma izolirana DNK
Ta dokument podaja smernice za obravnavo, dokumentiranje, shranjevanje in obdelavo aspiratov, pridobljenih z aspiracijsko biopsijo s tanko iglo (FNA), namenjenih za pregled gDNK med predpreiskovalno fazo, preden se izvede molekularna preiskava.
Ta dokument se uporablja za molekularne diagnostične preiskave in vitro, vključno z laboratorijsko razvitimi preskusi, ki jih izvajajo v medicinskih laboratorijih in laboratorijih za molekularno patologijo, kjer preiskujejo gDNK, izolirano iz aspiratov, pridobljenih z aspiracijsko biopsijo s tanko iglo. Namenjen je tudi temu, da ga uporabljajo laboratorijske stranke, razvijalci in proizvajalci diagnostike in vitro, biobanke, institucije in komercialne organizacije, ki izvajajo biomedicinske raziskave, ter regulativni organi.
Za zbiranje, stabiliziranje, prevoz in shrambo aspiratov, pridobljenih z aspiracijsko biopsijo z debelo iglo (biopsija FNA oz. FNA B) se uporabljajo drugačni namenski ukrepi, ki niso zajeti v tem dokumentu, temveč v standardih EN ISO 20184-3, Molekularne diagnostične preiskave in vitro – Specifikacije za predpreiskovalne procese za zamrznjena tkiva – 3. del: Izolirana DNK in EN ISO 20166-3, Molekularne diagnostične preiskave in vitro – Specifikacije za predpreiskovalne procese za tkiva, ki so fiksirana v formalinu ter položena v parafin – 3. del: Izolirana DNK.
Ta dokument se ne uporablja za preiskave patogene DNK in preiskave gDNK z odkrivanjem in situ.
OPOMBA: Za določene teme, ki so zajete v tem dokumentu, lahko veljajo tudi mednarodni, nacionalni ali regionalni predpisi ali zahteve.
General Information
- Status
- Published
- Publication Date
- 21-Dec-2021
- Technical Committee
- CEN/TC 140 - In vitro diagnostic systems
- Drafting Committee
- CEN/TC 140/WG 3 - Quality management in the medical laboratory
- Current Stage
- 9060 - Closure of 2 Year Review Enquiry - Review Enquiry
- Start Date
- 04-Jun-2025
- Completion Date
- 04-Jun-2025
Relations
- Refers
EN ISO 15189:2022 - Medical laboratories - Requirements for quality and competence (ISO 15189:2022) - Effective Date
- 28-Jan-2026
- Effective Date
- 28-Jan-2026
Overview
CEN/TS 17688-3:2021 provides technical guidance for the pre‑examination handling of Fine Needle Aspirates (FNAs) when the intended downstream test is analysis of isolated genomic DNA (gDNA). It covers specimen collection, documentation, stabilization, transport, reception, processing, gDNA isolation, and storage during the pre‑analytical phase for molecular in vitro diagnostics. The document is a European Technical Specification aimed at improving sample quality and preserving DNA integrity for reliable molecular diagnostic results.
Key topics and requirements
The specification addresses practical pre‑analytical requirements and recommendations to reduce variability and DNA damage before molecular testing:
- Specimen collection and stabilization: selection of primary FNA collection devices and stabilizers appropriate for preserving cellular material and gDNA.
- Documentation and patient/specimen information: essential metadata to accompany FNAs for traceability and correct interpretation.
- Transport and storage conditions: guidance on ambient vs stabilized sample handling to minimize degradation during transit.
- Laboratory reception and sample processing: receipt procedures, aliquoting, cytological processing (cell suspensions, cell blocks, slides) and handling to maximize gDNA yield.
- gDNA isolation considerations: options for using commercial diagnostic kits or laboratory-developed procedures and special handling for low‑cellularity FNAs.
- Quantity and quality assessment: recommended approaches to assess gDNA concentration and integrity to meet analytical test performance.
- Storage of isolated gDNA: conditions for short‑ and long‑term storage to preserve nucleic acid quality.
- Impact of pre‑analytical variables: annexed experimental data and discussion on how stabilization methods and storage impact cell quality and gDNA yield.
The specification uses standardized language for obligations: “shall” for requirements, “should” for recommendations.
Practical applications
CEN/TS 17688-3:2021 is directly applicable to:
- Medical laboratories and molecular pathology laboratories performing in vitro diagnostic tests and laboratory‑developed tests on gDNA from FNAs.
- IVD developers and manufacturers designing collection devices, stabilizers, and gDNA extraction kits.
- Biobanks, research institutions, and commercial biomedical organizations that collect, store, or analyze FNA biospecimens.
- Regulatory bodies and quality managers seeking standardized pre‑analytical workflows to improve diagnostic accuracy and reproducibility.
Keywords: pre-examination, fine needle aspirates, FNA, genomic DNA, gDNA, molecular diagnostics, sample handling, specimen collection, storage, transport.
Related standards
- EN ISO 20184-3 - pre‑examination processes for frozen tissue (isolated DNA)
- EN ISO 20166-3 - pre‑examination processes for FFPE tissue (isolated DNA)
Note: CEN/TS 17688-3:2021 does not apply to pathogen DNA testing or in situ gDNA detection; national or regional regulations may also apply.
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
CEN/TS 17688-3:2021 is a technical specification published by the European Committee for Standardization (CEN). Its full title is "Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for Fine Needle Aspirates (FNAs) - Part 3: Isolated genomic DNA". This standard covers: This document gives guidelines on the handling, documentation, storage and processing of fine needle aspirates (FNAs) intended for gDNA examination during the pre-examination phase before a molecular examination is performed. This document is applicable to molecular in vitro diagnostic examinations including laboratory developed tests performed by medical laboratories and molecular pathology laboratories that examine gDNA isolated from FNAs. It is also intended to be used by laboratory customers, in vitro diagnostics developers and manufacturers, biobanks, institutions and commercial organisations performing biomedical research, and regulatory authorities. Different dedicated measures are taken for collecting, stabilizing, transporting and storing of core needle biopsies (FNA Biopsy or FNA B) and are not covered in this document, but EN ISO 20184-3, Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for frozen tissue - Part 3: Isolated DNA and EN ISO 20166-3, Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for formalin-fixed and paraffin-embedded (FFPE) tissue - Part 3: Isolated DNA. This document is not applicable for pathogen DNA examination and gDNA examination by in situ detection. NOTE International, national or regional regulations or requirements can also apply to specific topics covered in this document.
This document gives guidelines on the handling, documentation, storage and processing of fine needle aspirates (FNAs) intended for gDNA examination during the pre-examination phase before a molecular examination is performed. This document is applicable to molecular in vitro diagnostic examinations including laboratory developed tests performed by medical laboratories and molecular pathology laboratories that examine gDNA isolated from FNAs. It is also intended to be used by laboratory customers, in vitro diagnostics developers and manufacturers, biobanks, institutions and commercial organisations performing biomedical research, and regulatory authorities. Different dedicated measures are taken for collecting, stabilizing, transporting and storing of core needle biopsies (FNA Biopsy or FNA B) and are not covered in this document, but EN ISO 20184-3, Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for frozen tissue - Part 3: Isolated DNA and EN ISO 20166-3, Molecular in vitro diagnostic examinations - Specifications for pre-examination processes for formalin-fixed and paraffin-embedded (FFPE) tissue - Part 3: Isolated DNA. This document is not applicable for pathogen DNA examination and gDNA examination by in situ detection. NOTE International, national or regional regulations or requirements can also apply to specific topics covered in this document.
CEN/TS 17688-3:2021 is classified under the following ICS (International Classification for Standards) categories: 11.100.10 - In vitro diagnostic test systems. The ICS classification helps identify the subject area and facilitates finding related standards.
CEN/TS 17688-3:2021 has the following relationships with other standards: It is inter standard links to EN ISO 15189:2022, CEN/TS 17981-1:2023. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
CEN/TS 17688-3:2021 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
SLOVENSKI STANDARD
01-februar-2022
Molekularne diagnostične preiskave in vitro - Specifikacije za predpreiskovalne
procese pri aspiraciji s tanko iglo (FNA) - 3. del: Iz genoma izolirana DNK
Molecular in vitro diagnostic examinations - Specifications for pre-examination processes
for Fine Needle Aspirates (FNAs) - Part 3: Isolated genomic DNA
Molekularanalytische in‐vitro‐diagnostische Verfahren - Spezifikationen für
präanalytische Prozesse für Feinnadelaspirate - Teil 3: Isolierte genomische DNA
Analyses moléculaires de diagnostic in vitro - Spécifications pour les processus
préanalytiques pour les ponctions à l'aiguille fine - Partie 3: ADN génomique isolé
Ta slovenski standard je istoveten z: CEN/TS 17688-3:2021
ICS:
11.100.10 Diagnostični preskusni In vitro diagnostic test
sistemi in vitro systems
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
CEN/TS 17688-3
TECHNICAL SPECIFICATION
SPÉCIFICATION TECHNIQUE
December 2021
TECHNISCHE SPEZIFIKATION
ICS 11.100.10
English Version
Molecular in vitro diagnostic examinations - Specifications
for pre-examination processes for Fine Needle Aspirates
(FNAs) - Part 3: Isolated genomic DNA
Analyses moléculaires de diagnostic in vitro - Molekularanalytische in-vitro-diagnostische Verfahren
Spécifications pour les processus préanalytiques pour - Spezifikationen für präanalytische Prozesse für
les ponctions à l'aiguille fine - Partie 3: ADN génomique Feinnadelaspirate - Teil 3: Isolierte genomische DNA
isolé
This Technical Specification (CEN/TS) was approved by CEN on 15 November 2021 for provisional application.
The period of validity of this CEN/TS is limited initially to three years. After two years the members of CEN will be requested to
submit their comments, particularly on the question whether the CEN/TS can be converted into a European Standard.
CEN members are required to announce the existence of this CEN/TS in the same way as for an EN and to make the CEN/TS
available promptly at national level in an appropriate form. It is permissible to keep conflicting national standards in force (in
parallel to the CEN/TS) until the final decision about the possible conversion of the CEN/TS into an EN is reached.
CEN members are the national standards bodies of Austria, Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia,
Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway,
Poland, Portugal, Republic of North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and
United Kingdom.
EUROPEAN COMMITTEE FOR STANDARDIZATION
COMITÉ EUROPÉEN DE NORMALISATION
EUROPÄISCHES KOMITEE FÜR NORMUNG
CEN-CENELEC Management Centre: Rue de la Science 23, B-1040 Brussels
© 2021 CEN All rights of exploitation in any form and by any means reserved Ref. No. CEN/TS 17688-3:2021 E
worldwide for CEN national Members.
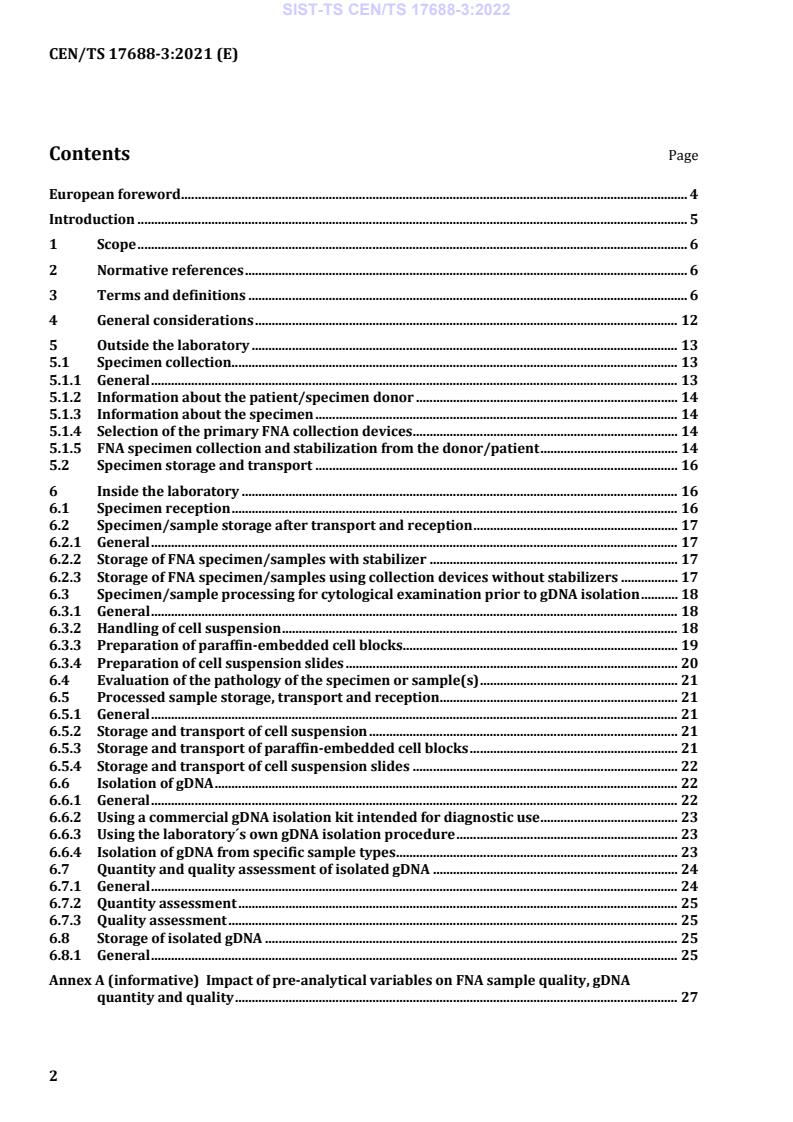
Contents Page
European foreword . 4
Introduction . 5
1 Scope . 6
2 Normative references . 6
3 Terms and definitions . 6
4 General considerations . 12
5 Outside the laboratory . 13
5.1 Specimen collection . 13
5.1.1 General . 13
5.1.2 Information about the patient/specimen donor . 14
5.1.3 Information about the specimen . 14
5.1.4 Selection of the primary FNA collection devices . 14
5.1.5 FNA specimen collection and stabilization from the donor/patient . 14
5.2 Specimen storage and transport . 16
6 Inside the laboratory . 16
6.1 Specimen reception . 16
6.2 Specimen/sample storage after transport and reception . 17
6.2.1 General . 17
6.2.2 Storage of FNA specimen/samples with stabilizer . 17
6.2.3 Storage of FNA specimen/samples using collection devices without stabilizers . 17
6.3 Specimen/sample processing for cytological examination prior to gDNA isolation . 18
6.3.1 General . 18
6.3.2 Handling of cell suspension . 18
6.3.3 Preparation of paraffin-embedded cell blocks. 19
6.3.4 Preparation of cell suspension slides . 20
6.4 Evaluation of the pathology of the specimen or sample(s) . 21
6.5 Processed sample storage, transport and reception . 21
6.5.1 General . 21
6.5.2 Storage and transport of cell suspension . 21
6.5.3 Storage and transport of paraffin-embedded cell blocks . 21
6.5.4 Storage and transport of cell suspension slides . 22
6.6 Isolation of gDNA . 22
6.6.1 General . 22
6.6.2 Using a commercial gDNA isolation kit intended for diagnostic use . 23
6.6.3 Using the laboratory´s own gDNA isolation procedure . 23
6.6.4 Isolation of gDNA from specific sample types . 23
6.7 Quantity and quality assessment of isolated gDNA . 24
6.7.1 General . 24
6.7.2 Quantity assessment . 25
6.7.3 Quality assessment . 25
6.8 Storage of isolated gDNA . 25
6.8.1 General . 25
Annex A (informative) Impact of pre-analytical variables on FNA sample quality, gDNA
quantity and quality . 27
A.1 Introduction. 27
A.2 Method - FNA model sample . 27
A.3 Result - Impact of specimen stabilization method on FNA cell quality . 28
A.3.1 General . 28
A.3.2 Method . 28
A.3.3 Result/conclusion. 31
A.4 Impact of stabilization and storage duration on quantity and quality of isolated
gDNA . 31
Bibliography . 35
European foreword
This document (CEN/TS 17688-3:2021) has been prepared by Technical Committee CEN/TC 140 “In
vitro diagnostic medical devices”, the secretariat of which is held by DIN.
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. CEN shall not be held responsible for identifying any or all such patent rights.
Any feedback and questions on this document should be directed to the users’ national standards body.
A complete listing of these bodies can be found on the CEN website.
According to the CEN/CENELEC Internal Regulations, the national standards organisations of the
following countries are bound to announce this Technical Specification: Austria, Belgium, Bulgaria,
Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland,
Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Netherlands, Norway, Poland, Portugal, Republic of
North Macedonia, Romania, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey and the United
Kingdom.
Introduction
Molecular in vitro diagnostics has enabled significant progress in medicine. Further progress is expected
by new technologies analysing profiles of nucleic acids, proteins, and metabolites in human tissues and
body fluids. However, the profiles of these molecules can change drastically during the pre-examination
process, including the specimen collection, transport, storage and processing.
Examination of genomic DNA (gDNA) is commonly used in clinical practice. This includes e.g. prognostic
and predictive biomarker examinations. This is a fast growing field in molecular diagnostics.
Fine needle aspiration is a non-surgical procedure that uses a thin, hollow-bore needle and syringe to
collect a specimen from patients for cytopathological and molecular investigation. As a minimally-
invasive technique, fine needle aspirates (FNAs) are commonly used to diagnose and monitor for example
a range of cancer types e.g. breast, lung and thyroid cancer, and other diseases, such as inflammatory
diseases. FNAs also provide the opportunity to sample metastatic sites (e.g. lymph nodes) and otherwise
non-resectable tissues.
Besides cytological assessment, molecular biological analysis of FNAs is expected to become increasingly
used for cancer and other disease diagnostics, including companion diagnostics.
One of the challenges facing molecular analysis of FNA samples is their small size and diversity in
composition (cells, blood, body fluid). The low cellular content of FNAs means that the yield of isolated
gDNA is typically towards the lower end of detection for molecular examination. Therefore, the gDNA
isolation procedure should provide a sufficient amount of gDNA as required by the specific examination.
After specimen collection, gDNA can fragment and degrade by e.g. fixation, processing and storage.
Additionally, chemical modifications introduced into gDNA during FNA fixation might lead to sequence
alterations or changes in the methylation status. The described changes of the gDNA molecules can
impact the validity, reliability and sensitivity of the examination results.
Therefore, standardization of the entire process from specimen collection to gDNA examination is needed
to minimize gDNA changes introduced by e.g. degradation, fragmentation and modification after FNA
collection. This document describes special measures which need to be taken to obtain good quality FNA
specimens/samples and isolated gDNA therefrom for molecular examination.
In this document, the following verbal forms are used:
— “shall” indicates a requirement;
— “should” indicates a recommendation;
— “may” indicates a permission;
— “can” indicates a possibility or a capability.
1 Scope
This document gives guidelines on the handling, documentation, storage and processing of fine needle
aspirates (FNAs) intended for gDNA examination during the pre-examination phase before a molecular
examination is performed.
This document is applicable to molecular in vitro diagnostic examinations including laboratory developed
tests performed by medical laboratories and molecular pathology laboratories that examine gDNA
isolated from FNAs. It is also intended to be used by laboratory customers, in vitro diagnostics developers
and manufacturers, biobanks, institutions and commercial organisations performing biomedical
research, and regulatory authorities.
Different dedicated measures are taken for collecting, stabilizing, transporting and storing of core needle
biopsies (FNA Biopsy or FNA B) and are not covered in this document, but EN ISO 20184-3, Molecular in
vitro diagnostic examinations — Specifications for pre-examination processes for frozen tissue — Part 3:
Isolated DNA and EN ISO 20166-3, Molecular in vitro diagnostic examinations — Specifications for pre-
examination processes for formalin-fixed and paraffin-embedded (FFPE) tissue — Part 3: Isolated DNA.
This document is not applicable for pathogen DNA examination and gDNA examination by in situ
detection.
NOTE International, national or regional regulations or requirements can also apply to specific topics covered
in this document.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
EN ISO 15189, Medical laboratories — Requirements for quality and competence (ISO 15189)
3 Terms and definitions
For the purposes of this document, the terms and definitions given in EN ISO 15189 and the following
apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https://www.iso.org/obp
— IEC Electropedia: available at https://www.electropedia.org/
3.1
aliquot
portion of a larger amount of homogenous material, assumed to be taken with negligible sampling error
Note 1 to entry: The term is usually applied to fluids. Tissues are heterogeneous and therefore cannot be
aliquoted.
Note 2 to entry: The definition is derived from the Compendium of Chemical Terminology Gold Book.
International Union of Pure and Applied Chemistry. Version 2.3.3., 2014; the PAC, 1990,62,1193 (Nomenclature for
sampling in analytical chemistry (Recommendations 1990)) p. 1206; and the PAC 1990, 62, 2167 (Glossary of
atmospheric chemistry terms (Recommendations 1990)) p. 2173.
3.2
ambient temperature
unregulated temperature of the surrounding air
[SOURCE: EN ISO 20166-1:2018, 3.2]
3.3
analyte
component represented in the name of a measurable quantity
[SOURCE: ISO 17511:2020, 3.2, modified — Deleted example.]
3.4
analytical test performance
analytical performance
accuracy, precision, and sensitivity of a test to measure the analyte of interest
Note 1 to entry: Other test performance characteristics such as robustness, repeatability can apply as well.
[SOURCE: EN ISO 20184-1:2018, 3.4]
3.5
biomolecule
organic molecule produced by living organisms that is involved in the maintenance and metabolic
processes of organisms
Note 1 to entry: Examples of organic molecules are protein, carbohydrate, lipid, or nucleic acid.
3.6
cell block
paraffin-embedded cell clot
3.7
cell clot
cell-rich liquid specimen/sample concentrated into a compact cell aggregate for subsequent processing
3.8
closed system
non-modifiable system provided by the vendor including all necessary components for the analysis (i.e.,
hardware, software, procedures and reagents)
3.9
cytocentrifugation
cytology method that is specifically designed to concentrate cells on a slide by centrifugation
3.10
deoxyribonucleic acid
DNA
polymer of deoxyribonucleotides occurring in a double-stranded (dsDNA) or single-stranded (ssDNA)
form
[SOURCE: EN ISO 22174:2005, 3.1.2]
3.11
deoxyribonuclease
DNase
enzyme that catalyses the degradation of DNA into smaller components
3.12
diagnosis
identification of a disease from its signs and symptoms, where the diagnostic process can involve
examinations and tests for classification of an individual's condition into separate and distinct categories
or subclasses that allow medical decisions about treatment and prognosis to be made
[SOURCE: EN ISO 20166-1:2018, 3.7]
3.13
examination
analytical test
set of operations with the objective of determining the value or characteristics of a property
Note 1 to entry: Processes that include all kinds of parameter testing or chemical manipulation for quantitative
or qualitative examination.
[SOURCE: EN ISO 15189:2012, 3.7, modified — Notes to entry 1 to 3 have been removed. Note 1 to entry
has been added and “analytical test” has been added as a preferred term.]
3.14
examination manufacturer
analytical test manufacturer
entity that manufactures and/or produces a specific analytical test
3.15
examination performance
analytical test performance
analytical performance
accuracy, precision, and sensitivity of a test to measure the analyte of interest
Note 1 to entry: Other test performance characteristics such as robustness, repeatability can apply as well.
[SOURCE: EN ISO 20184-1:2018, 3.4]
3.16
fixative
solution used to preserve or harden FNA specimens for microscopic and molecular examination
3.17
formalin
saturated aqueous formaldehyde solution which at 100 % contains 37 % formaldehyde by mass
(corresponding to 40 % by volume)
[SOURCE: EN ISO 20166-1:2018, 3.11]
3.18
fine needle aspirate
FNA
specimen withdrawn by a non-operative procedure that uses a thin, hollow-bore needle
3.19
FNA primary collection device
thin, hollow-bore needle or syringe used for collecting the FNA specimen from the donor/patient
3.20
FNA secondary collection device
suitable container into which the specimen is transferred from the FNA primary collection device
3.21
genomic DNA
gDNA
chromosomal DNA, in contrast to extra-chromosomal DNAs such as mitochondrial DNA
3.22
homogeneous
uniform in structure and composition
[SOURCE: EN ISO 20166-1:2018, 3.31]
3.23
interfering substances
endogenous substances of a specimen/sample or exogenous substances that can alter an examination
result
Note 1 to entry: Examples of endogenous substances include blood components in the FNA specimen.
Note 2 to entry: Examples of exogenous substances include compounds of stabilization solutions.
3.24
laboratory developed procedure
modified commercially available in vitro diagnostic device or fully in house developed procedure
3.25
paraffin embedding
process in which a sample is placed in paraffin to generate a hard surrounding matrix so that thin
microscopic sections can be cut
3.26
pre-examination process
pre-analytical workflow
pre-analytical phase
pre-examination phase
process that starts, in chronological order, from the clinician’s request and includes the examination
request, preparation and identification of the patient, collection of the primary sample(s), transportation
to and within the analytical laboratory, isolation of analytes, and ends when the analytical examination
begins
Note 1 to entry: The pre-examination phase includes preparative processes that influence the outcome of the
intended examination.
[SOURCE: EN ISO 15189:2012, 3.15, modified — An additional term was added and more detail was
included.]
3.27
primary sample
specimen
discrete portion of a body fluid, breath, hair or tissue taken for examination, study or analysis of one or
more quantities or properties assumed to apply for the whole
[SOURCE: EN ISO 15189:2012, 3.16, modified — The term and definition is used here without the original
notes.]
3.28
proficiency test
evaluation of participant performance against pre-established criteria by means of inter-laboratory
comparisons
[SOURCE: EN ISO/IEC 17043:2010, 3.7, modified — Term and definition are used here without the
original notes.]
3.29
ribonucleic acid
RNA
polymer of ribonucleotides occurring in a double-stranded or single-stranded form
[SOURCE: EN ISO 22174:2005, 3.1.3]
3.30
ribonuclease
RNase
enzyme that catalyses the degradation of RNA into smaller components
3.31
room temperature
temperature in the range of 18 °C to 25 °C
Note 1 to entry: Local or national regulations can have different definitions.
[SOURCE: EN ISO 20166-1:2018, 3.22]
3.32
sample
one or more parts taken from a specimen
[SOURCE: EN ISO 15189:2012, 3.24, modified — Example has been removed.]
3.33
stability
ability of a sample material, when stored under specified conditions, to maintain a stated property value
within specified limits for a specified period of time
[SOURCE ISO Guide 30:2015, 2.1.15, modified — The words “reference material” were replaced by
“sample material”.]
3.34
stabilizer
substance which has the ability to maintain a stated property value within specified limits for a specified
period of time of a sample material
Note 1 to entry: The substance can contain a fixative belonging to different fixative subgroups e.g. crosslinking
fixatives (e.g. formalin) or coagulating fixatives (e.g. methanol, ethanol).
3.35
stabilization
process of maintaining a stated property value within specified limits for a specified period of time of a
specimen/sample material
3.36
standard buffered formalin solution
neutral buffered formalin
NBF
10 % formalin solution in water with a mass fraction of 3,7 % (corresponding to a volume fraction of 4 %)
formaldehyde, buffered to pH 6,8 to pH 7,2
Note 1 to entry: Standard buffered formalin solutions often contain small amounts of methanol to inhibit
oxidation and polymerisation of formaldehyde.
[SOURCE: EN ISO 20166-1:2018, 3.25]
3.37
storage
prolonged interruption of the pre-analytical workflow of a sample or analyte respectively, or of their
derivatives, under appropriate conditions in order to preserve their properties
Note 1 to entry: Long-term storage typically occurs in laboratory archives or in biobanks.
[SOURCE: EN ISO 20184-1:2018, 3.21, modified — Example has been removed.]
3.38
tissue processor
automated instrument where tissue fixation, dehydration, clearing and impregnation (with paraffin)
occur
[SOURCE: EN ISO 20166-1:2018, 3.27]
3.39
validation
confirmation, through the provision of objective evidence, that the requirements for a specific intended
use or application have been fulfilled
Note 1 to entry: The term “validated” is used to designate the corresponding status.
[SOURCE: EN ISO 9000:2015, 3.8.13, modified — Note 1 and Note 3 have been omitted.]
3.40
verification
confirmation, through the provision of objective evidence, that specified requirements have been fulfilled
Note 1 to entry: The term “verified” is used to designate the corresponding status.
Note 2 to entry: Confirmation can comprise activities such as:
— performing alternative calculations;
— comparing a new design specification with a similar proven design specification;
— undertaking tests and demonstrations;
— reviewing documents prior to issue.
[SOURCE: EN ISO 9000:2015, 3.8.12, modified — Note 1 and Note 2 have been omitted.]
3.41
workflow
series of activities necessary to complete a task
[SOURCE: EN ISO 20166-1:2018, 3.30]
4 General considerations
For general statements on medical laboratory quality management systems and in particular on
specimen collection, reception and handling (including avoidance of cross contaminations) see
EN ISO 15189, EN ISO/IEC 17020 or EN ISO/IEC 17025. ISO/TS 20658 and EN ISO 20387 (for
biobanking) can also apply. The requirements on laboratory equipment, reagents, and consumables
according to EN ISO 15189 shall be followed; EN ISO/IEC 17020 and EN ISO/IEC 17025 can also apply.
All steps of the pre-examination, examination and post-examination processes (i.e. the entire workflow)
can influence the diagnosis or research study results.
Different examinations, even if they are based on same technology (e.g. different targets of mutation
analysis by qPCR or NGS, SNP analysis by SSCP) can have different requirements regarding the quality
(e.g. integrity, purity, methylation pattern) and quantity of gDNA.
Thus, this entire workflow shall be specified, verified and validated during the development of the
examination, including the development of in vitro diagnostic (IVD) medical devices. This includes
specifically all pre-examination process steps such as the examination request, preparation and
identification of the patient, collection of the primary sample(s), transport to and within the medical
laboratory, storage and isolation of gDNA. The specifications about the specimen transport and storage
shall also take into account the specimen's gDNA quality required for the intended examination (e.g.
integrity and chemical modifications such as methylation patterns). This should include the timeframe
between collecting the specimen and the gDNA isolation as well as storage conditions such as duration,
temperature limits and freeze/thaw cycles. The verification and validation shall take into account the
impact of the FNA specimen's variability, e.g. by tissue type, heterogeneity, specimen quantity, presence
of blood and inflammatory cells, on examinations.
During the design and development of a FNA gDNA based examination, a risk assessment shall be
performed (see also ISO 14971). Mitigation measures for eliminating or reducing identified risks shall be
established, where required, for ensuring the performance of the examination. It shall especially be
investigated and ensured that the gDNA intended to be analysed is not compromised in a manner
impacting the examination performance. This includes investigations on whether and/or how the gDNA
intended to be examined changes during storage and transport. This can be done, e.g. by applying the
intended examination to specimens/samples which underwent time course studies reflecting the
individual pre-examination process steps such as transport and storage and by implementing measures
to prevent or reduce impacts by the identified pre-analytical variables.
NOTE A time course experiment is a research design that involves repeated observations of the same variables
at specific intervals over a relevant time period (e.g. time 0, 12 h, 24 h, 36 h, 48 h). This is expected to reflect any
knowledge on the stability of the gDNA sequences of interest. Typically, this involves using aliquots from a
homogeneous starting material (see Annex A).
During the whole pre-examination process precautions shall be taken to avoid cross contamination
between different specimens/samples (e.g. using single-use material whenever feasible or appropriate
cleaning procedures between processing of different specimens/samples), and to avoid mixing up of
specimens/samples.
During transportation and transient storage between pre-analytical workflow steps, gDNA can fragment
and degrade and can also be modified (e.g. by methylation). Where the examination is impacted by such
pre-analytical variables, the specimen should therefore be placed in a collection device containing an
appropriate stabilizer solution. The maximum duration until the specimen is placed into stabilizer
solution should be specified and verified. The duration and the temperature before stabilization shall be
documented.
Safety instructions for the whole pre-examination process shall be in place and followed. Safety
regulations on specimen/sample transport and handling shall be considered (see EN ISO 15189,
ISO 15190 and ISO/TS 20658). If transport is required over public areas, corresponding regulations or
laws for packaging and transport apply (e.g. International Air Transport Association (IATA) for air
transport).
The manufacturer's material safety data sheet shall be considered for any potentially hazardous material
(e.g. stabilizers such as formaldehyde and methanol).
For all pre-examination steps, the examination manufacturer's instructions shall be followed.
Where, for justified reasons (e.g. unmet patient needs), a commercial product is not used in accordance
to the manufacturer's instructions, responsibility for its verification, validation, use and performance lies
with the laboratory.
5 Outside the laboratory
5.1 Specimen collection
5.1.1 General
For the collection of the FNA specimen, the requirements for the intended molecular examination (e.g.
disease condition, specimen type; see also Clause 6) shall be considered.
See also EN ISO 15189.
5.1.2 Information about the patient/specimen donor
The documentation shall include the identity of the patient/specimen donor, which can be in the form of
a code.
The documentation should include, but is not limited to:
a) the relevant health status of the patient/specimen donor (e.g. disease type, concomitant disease,
demographics [e.g. age and gender]);
b) the information about routine medical treatment and special treatment prior to FNA collection (e.g.
anaesthetics, medications, surgical or diagnostic procedures);
c) the appropriate consent from the patient/specimen donor.
5.1.3 Information about the specimen
The documentation should include, but is not limited to:
a) the type and the purpose of the examination requested including type and location of the FNA
procedure (e.g. lung, lymph node, thyroid gland, breast, head and neck, pancreas);
b) the time and date when the FNA specimen is removed from the body;
c) the aspiration technique used (e.g. suction, capillary method, ultrasound-guided FNA, device used);
d) the tissue condition (e.g. diseased, unaffected by the disease), including references to any
topographic description made by e.g. a surgeon, radiologist or oncologist;
e) the documentation of steps described under 6.2, if the FNA specimen/sample stabilization starts
outside the laboratory at the collection facility.
The documentation should also include the name/identity of the responsible person for collecting the
specimen.
5.1.4 Selection of the primary FNA collection devices
The FNA gDNA integrity and other quality parameters can be influenced by inadequate collection
procedures and inappropriate storage/transport conditions (see 4), FNA specimen/sample preparation
(see 6.3) as well as by gDNA isolation procedures (see 6.6).
FNA specimens should be collected from the donor/patient using appropriate FNA primary collection
devices (needles and syringes) enabling conventional slide preparation techniques.
The gDNA examination manufacturer instructions should contain specifications on the FNA primary
collection device (needle and syringe) to be used. Where the examination manufacturer specifies usage
of FNA primary collection devices, these shall be used. Where the examination manufacturer does not
provide such specifications (e.g. due to (a) former less stringent legal framework(s)), the primary
collection device shall be specified, verified and documented by the laboratory.
5.1.5 FNA specimen collection and stabilization from the donor/patient
5.1.5.1 General
The gDNA examination manufacturer shall provide specified and verified instructions on the FNA
collection and stabilization procedure. These shall be followed.
Where the examination manufacturer does not provide such specifications (e.g. due to (a) former less
stringent legal framework(s)) the instructions provided by the FNA collection device manufacturer shall
be verified by the laboratory for the intended gDNA examination.
Where the examination manufacturer and the FNA collection device manufacturer do not provide such
specifications (e.g. due to (a) former less stringent legal framework(s)), the procedure shall be specified,
verified and documented by the laboratory. Instructions shall be written accordingly for the user and
followed.
For transport, storage, processing and for subsequent gDNA examination, the FNA specimen/samples are
usually transferred into a FNA secondary collection device. This device should be suitable for
centrifugation and should either contain or allow adding a stabilizer (e.g. 15-50 ml polypropylene tubes).
The stabilizer to FNA volume ratio depends on the type of stabilizer and the type of FNA
specimen/sample. This shall be specified and verified.
Where the examination manufacturer specifies usage of FNA secondary collection devices, these shall be
used. Where the examination manufacturer does not provide such specifications (e.g. due to (a) former
less stringent legal framework(s)), the secondary collection device shall be specified, selected, verified
and documented by the laboratory.
For the labelling (sample/specimen identification) of the FNA secondary collection device, a routine
procedure (e.g. as specified in EN ISO 15189 for medical laboratories or EN ISO 20387 for biobanks) shall
be used. Where appropriate, additional information can be provided (e.g. in form of a 2D-barcode).
The procedure of the FNA specimen collection shall be documented, including the collection devices.
Several FNA specimens from the same patient/donor and the same lesion or site may be put into a single
secondary collection device.
The following steps shall be performed (but are not limited to):
a) the documentation of any additions or modifications to the specimen after removal from the body
(e.g. wash of needle and syringe, addition of reagents);
b) the labelling of the primary and/or secondary collection device (e.g. barcode, specimen type,
quantity, and organ tissue of origin) and additional documentation (information as specified in 5.1.2,
5.1.3);
c) the selection and use of stabilization procedures and packages used for transport according to
applicable regulations (e.g. cooling box for storing and transportation).
5.1.5.2 FNA specimen/sample collection with stabilizers
FNA specimens/samples are usually examined for primary diagnosis with conventional cytological
staining procedures (e.g. May–Grünwald and/or Giemsa staining, PAP stain). The same
specimens/samples can also be used for gDNA examinations thereafter. Stabilization reagents used for
preservation of gDNA (i.e. minimizing DNA degradation, modification and fragmentation) should
therefore also fulfil the cytological examination requirements, where the same sample is used for both,
cytological and gDNA examinations (see Annex A). Where such different examinations are performed, the
stabilizer containing secondary collection device or the stabilization bulk reagent should be selected
appropriately and shall be verified for these examinations by the cytological and/or gDNA examination
laboratory.
FNA stabilizers should sufficiently prevent microbial growth for avoiding impacts on the examination
performance caused by microbial contamination (e.g. target degradation).
If the FNA specimen/sample(s) is/are intended to be directly fixed or stabilized at the collection facility
before transport to the laboratory, the specimen/samples should be transferred from the FNA
syringe/needle to the secondary collection device, containing the stabilization reagent. The duration
between collection and transfer to the stabilization reagent shall be specified and verified according to
the intended examination requirements. The FNA syringe/needle should be rinsed with an appropriate
solution, e.g. stabilizer, buffer or Ringer solution, to collect all residual specimen material after transfer
of specimen. Where the stabilizer manufacturer or the examination manufacturer has specified a rinsing
solution, this shall be used.
5.1.5.3 FNA specimen/sample collection without stabilizers
Where required for justified diagnostic reasons (e.g. dedicated cytological examination not compatible
with the gDNA stabilizer), the cytological and/or the gDNA examination laboratory shall decide whether
to use a FNA specimen/sample collection without a stabilizer.
The storage conditions and maximum duration under these conditions until optional stabilization at a
later workflow step and/or gDNA isolation shall be specified and verified according to the examination
requirements.
5.2 Specimen storage and transport
The examination manufacturer should provide specified and verified instructions for the storage and
transport of the collected FNA specimen (e.g. duration, temperature) and these shall be followed.
Where the examination manufacturer does not provide such specifications (e.g. due to (a) former less
stringent legal framework(s)), the procedure shall be specified, verified and documented by the
laboratory. Instructions shall be written accordingly for the user and followed.
When selecting and using transport packages (e.g. box for storing and transportation), transport
regulations apply.
The temperatures of the primary or secondary collection device’s surroundings should be measured and
documented. If the temperature cannot be measured, the temperature shall be estimated and
documented (e.g. as ambient temperature, room temperature, at 2 °C to 8 °C or wet ice).
Unintended freeze–thawing of the FNA specimen and/or sample(s) (e.g. by incorrectly using cool packs)
can impact the gDNA integrity. It can also impact the cytological characterization. This can be mitigated
by processing the specimen/sample(s) directly or by transferring them into a stabilizer solution.
Any deviations to nonconformities from the verified storage and transport conditions in the written
instructions shall be documented.
6 Inside the laboratory
6.1 Specimen reception
The identity of the person receiving the specimen and/or sample(s) shall be documented. This can e.g. be
done in the form of the name or a code.
The correct identity of the specimen/sample(s) shall be checked. This should include the clinical
information (see 5.1.1 and 5.1.2) of the specimen/sample(s), hospital admission number and/or
patient/specimen donor identity, name of the patient/specimen donor and date of birth of the
patient/specimen donor. In certain instances, e.g. in research studies, it might be necessary to only work
with a code.
The arrival date, time and nonconformities of labelling, storage and transport conditions (e.g.
temperature, duration) and leaking/broken tubes, etc. shall be documented. Any deviations from the
established procedures for collection (see 5.1), storage and transport (see 5.2) shall be documented.
NOTE This includes for example a note, when specimen/sample(s) have been accidentally frozen.
Where there are nonconformities in collection, labelling, transport and storage of the FNA
specimen/sample(s) that could affect the validity and reliability of the examination, a new specimen
should be obtained, where possible.
6.2 Specimen/sample storage after transport and reception
6.2.1 General
The storage temperature at the laboratory shall be documented.
The total storage duration includes storage durations at the FNA specimen collection facility, the first
examination laboratory (e.g. cytology laboratory), the gDNA examination laboratory and all transport
durations between these.
The maximum storage duration specified by the examination manufacturer or, if this is not available, by
the collection device manufacturer shall not be exceeded.
Where none of these are available, the maximum storage duration for defined temperature ranges shall
be specified and verified by the laboratory for the intended examination.
6.2.2 Storage of FNA specimen/samples with stabilizer
For storing the FNA in devices with stabilizers, the examination manufacturer's instructions on storage
conditions before processing the FNA for gDNA isolation shall be followed.
Where the examination manufact
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...