ISO/PRF TR 29322
(Main)Health informatics — Guidance on the management of clinical risk relating to the deployment and use of health software systems
Health informatics — Guidance on the management of clinical risk relating to the deployment and use of health software systems
ISO/TR 29322:2008 considers the risk management processes required to ensure patient safety in respect to the deployment and use of health software products either as a new system within a health organization or as changes to an existing system's environment. It is addressed to those persons in health organizations who are responsible for ensuring the safety of health software in health organizations through the application of risk management. Whilst it is therefore principally addressed to healthcare organizations, ISO/TR 29322:2008 will also prove useful reference to those involved in the manufacture of health software products. Equally, readers of this Technical Report are recommended to review ISO/TS 29321:2008.
Informatique de santé — Directives relatives à la gestion du risque clinique lié au déploiement et à l'utilisation des systèmes de logiciel de santé
General Information
Relations
Standards Content (Sample)
TECHNICAL ISO/TR
REPORT 29322
First edition
2008-##-##
Health informatics — Guidance on the
management of clinical risk relating to
the deployment and use of health
software systems
Informatique de santé — Directives relatives à la gestion du risque
clinique lié au déploiement et à l'utilisation des systèmes de logiciel de
santé
PROOF/ÉPREUVE
Reference number
ISO/TR 29322:2008(E)
©
ISO 2008
---------------------- Page: 1 ----------------------
ISO/TR 29322:2008(E)
PDF disclaimer
This PDF file may contain embedded typefaces. In accordance with Adobe's licensing policy, this file may be printed or viewed but
shall not be edited unless the typefaces which are embedded are licensed to and installed on the computer performing the editing. In
downloading this file, parties accept therein the responsibility of not infringing Adobe's licensing policy. The ISO Central Secretariat
accepts no liability in this area.
Adobe is a trademark of Adobe Systems Incorporated.
Details of the software products used to create this PDF file can be found in the General Info relative to the file; the PDF-creation
parameters were optimized for printing. Every care has been taken to ensure that the file is suitable for use by ISO member bodies. In
the unlikely event that a problem relating to it is found, please inform the Central Secretariat at the address given below.
COPYRIGHT PROTECTED DOCUMENT
© ISO 2008
All rights reserved. Unless otherwise specified, no part of this publication may be reproduced or utilized in any form or by any means,
electronic or mechanical, including photocopying and microfilm, without permission in writing from either ISO at the address below or
ISO's member body in the country of the requester.
ISO copyright office
Case postale 56 • CH-1211 Geneva 20
Tel. + 41 22 749 01 11
Fax + 41 22 749 09 47
E-mail copyright@iso.org
Web www.iso.org
Published in Switzerland
ii PROOF/ÉPREUVE © ISO 2008 – All rights reserved
---------------------- Page: 2 ----------------------
ISO/TR 29322:2008(E)
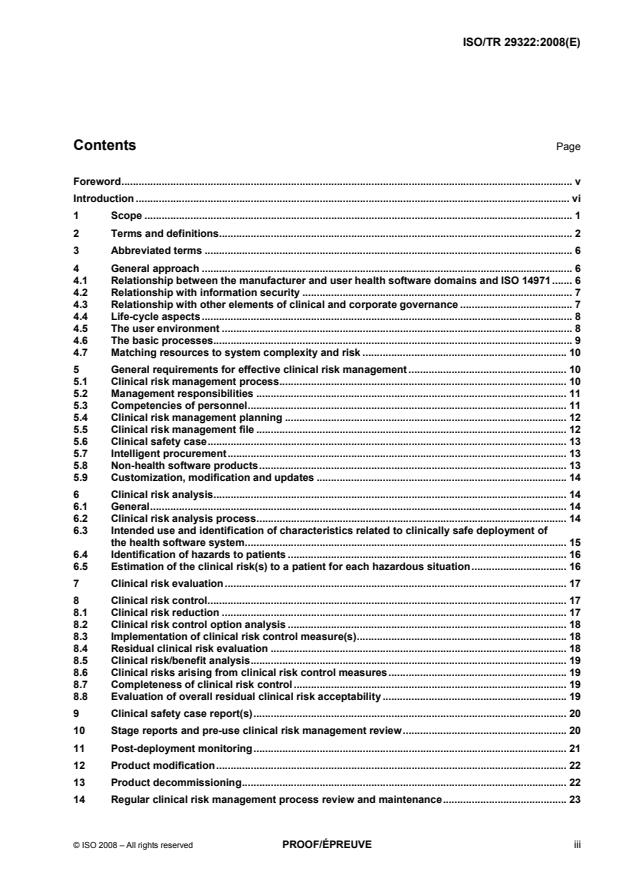
Contents Page
Foreword. v
Introduction . vi
1 Scope . 1
2 Terms and definitions. 2
3 Abbreviated terms . 6
4 General approach . 6
4.1 Relationship between the manufacturer and user health software domains and ISO 14971. 6
4.2 Relationship with information security . 7
4.3 Relationship with other elements of clinical and corporate governance . 7
4.4 Life-cycle aspects. 8
4.5 The user environment . 8
4.6 The basic processes. 9
4.7 Matching resources to system complexity and risk . 10
5 General requirements for effective clinical risk management . 10
5.1 Clinical risk management process. 10
5.2 Management responsibilities . 11
5.3 Competencies of personnel. 11
5.4 Clinical risk management planning . 12
5.5 Clinical risk management file . 12
5.6 Clinical safety case. 13
5.7 Intelligent procurement. 13
5.8 Non-health software products. 13
5.9 Customization, modification and updates . 14
6 Clinical risk analysis. 14
6.1 General. 14
6.2 Clinical risk analysis process. 14
6.3 Intended use and identification of characteristics related to clinically safe deployment of
the health software system. 15
6.4 Identification of hazards to patients . 16
6.5 Estimation of the clinical risk(s) to a patient for each hazardous situation. 16
7 Clinical risk evaluation. 17
8 Clinical risk control. 17
8.1 Clinical risk reduction . 17
8.2 Clinical risk control option analysis . 18
8.3 Implementation of clinical risk control measure(s). 18
8.4 Residual clinical risk evaluation . 18
8.5 Clinical risk/benefit analysis. 19
8.6 Clinical risks arising from clinical risk control measures. 19
8.7 Completeness of clinical risk control. 19
8.8 Evaluation of overall residual clinical risk acceptability . 19
9 Clinical safety case report(s). 20
10 Stage reports and pre-use clinical risk management review. 20
11 Post-deployment monitoring. 21
12 Product modification. 22
13 Product decommissioning. 22
14 Regular clinical risk management process review and maintenance. 23
© ISO 2008 – All rights reserved PROOF/ÉPREUVE iii
---------------------- Page: 3 ----------------------
ISO/TR 29322:2008(E)
Annex A (informative) Examples of potential harm presented by health software . 24
Annex B (informative) Conclusions of the CEN/ISO/TR measures for ensuring patient safety of
health software. 27
Annex C (informative) Clinical risk management plan. 29
Annex D (informative) Components of a generic risk management process . 31
Annex E (informative) Relationship between clinical risk management file, clinical safety case,
clinical safety case reports, stage reports and product life-cycle. 35
Annex F (informative) Clinical risk estimation and evaluation guidance . 39
Annex G (informative) Risk control guidance. 48
Annex H (informative) Some particular risks. 57
Annex I (informative) Requirements of a clinical safety case report . 60
Annex J (informative) Matching resources to organizational complexity and risk . 61
Bibliography . 64
iv PROOF/ÉPREUVE © ISO 2008 – All rights reserved
---------------------- Page: 4 ----------------------
ISO/TR 29322:2008(E)
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards bodies
(ISO member bodies). The work of preparing International Standards is normally carried out through ISO
technical committees. Each member body interested in a subject for which a technical committee has been
established has the right to be represented on that committee. International organizations, governmental and
non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely with the
International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
International Standards are drafted in accordance with the rules given in the ISO/IEC Directives, Part 2.
The main task of technical committees is to prepare International Standards. Draft International Standards
adopted by the technical committees are circulated to the member bodies for voting. Publication as an
International Standard requires approval by at least 75 % of the member bodies casting a vote.
In exceptional circumstances, when a technical committee has collected data of a different kind from that
which is normally published as an International Standard (“state of the art”, for example), it may decide by a
simple majority vote of its participating members to publish a Technical Report. A Technical Report is entirely
informative in nature and does not have to be reviewed until the data it provides are considered to be no
longer valid or useful.
Attention is drawn to the possibility that some of the elements of this document may be the subject of patent
rights. ISO shall not be held responsible for identifying any or all such patent rights.
ISO/TR 29322 was prepared by Technical Committee ISO/TC 215, Health informatics in collaboration with
Technical Committee CEN/TC 251, Health informatics.
© ISO 2008 – All rights reserved PROOF/ÉPREUVE v
---------------------- Page: 5 ----------------------
ISO/TR 29322:2008(E)
Introduction
The threat to patient safety
There is mounting concern around the world about the substantial number of avoidable clinical incidents which
have an adverse effect on patients, of which a significant proportion result in avoidable death or serious
disability, see References [1], [2], [3], [4], [5] and [6]. A number of such avoidable incidents involved poor or
“wrong” diagnoses or other decisions. A contributing factor is often missing or incomplete information, or
simply ignorance, e.g. of clinical options in difficult circumstances or of the cross-reaction of treatments (a
substantial percentage of clinical incidents are related to missing or incomplete information).
It is increasingly claimed that information systems such as decision support, protocols, guidelines and
pathways could markedly reduce such adverse effects. If for no other reason – and there are others – this is
leading to increasing deployment and use of increasingly complex health software systems, such as for
decision support and disease management. It can also be anticipated that, due to pressures on time and to
medico-legal aspects, clinicians will increasingly rely on such systems, with less questioning of their “output”,
as a “foreground” part of care delivery rather than as a “background” adjunct to it. Indeed, as such systems
become integrated with medical care, any failure by clinicians to use standard support facilities may be
criticised on legal grounds.
Increased use of such systems is not only in clinical treatment but also in areas just as important to patient
safety, such as referral decision-making. Failure to make a “correct” referral, or to make one “in time”, can
have serious consequences.
Economic pressures are also leading to more decision support systems. The area of generic and/or economic
prescribing is the most obvious, but achieving economy in the number and costs of clinical investigative tests
is another.
Thus the use of health software and medical devices in increasingly integrated systems, e.g. networks, can
bring substantial benefit to patients. However unless they are proven to be safe and fit for purpose they may
also present potential for harm or at least deter clinical and other health delivery staff from making use of them,
to the ultimate detriment of patients. Annex A provides some examples of the potential for harm.
Harm can of course result from unquestioning and/or non-professional use, although the manufacturers of
health software products, and those in health organizations deploying and using such products within systems,
can mitigate such circumstances through, for example, instructions for use, training and on-screen
presentation techniques, guidance, warnings or instructions.
Some of these system deficiencies are insidious, may be invisible to the end user and are typically out of the
sole control of either the manufacturer or the deploying health organization.
Failures and deficiencies in health software systems can, of course, have adverse impacts other than causing
harm to patients. They may, for example, create administrative inconvenience or even administrative chaos,
with a range of impacts on the organization including financial loss. Harm to a patient may also have a
consequent impact on the organization such as financial loss resulting from litigation. Whereas these adverse
organizational impacts will be significant, they are not the subject of this document unless they result in harm
to a patient. It is the potential harm to the patient which is the subject of this document.
Controlling the risks
The safety of medicines and medical devices is ensured in many countries through a variety of legal and
administrative measures which bear on manufacture. In the European Union, the safety of medical devices is
subject to several EU directives, see References [7], [8], [9] and [36]. These measures are often backed by a
range of safety related standards from a number of sources, both national and international, including the
International Organization for Standardization (ISO), the International Electrotechnical Commission (IEC), the
vi PROOF/ÉPREUVE © ISO 2008 – All rights reserved
---------------------- Page: 6 ----------------------
ISO/TR 29322:2008(E)
European Committee for Standardization (CEN), the European Committee for Electrotechnical
Standardization (CENELEC) and others. Some software, such as that necessary for the proper application or
functioning of a medical device, is often encompassed by these legislative controls. Some software may be
considered a medical device in its own right. However, there is software applied to health whose manufacture
is not covered or is encompassed in a less than clear manner or is currently not a primary focus of some
regulatory body. Thus there is health software whose safety in manufacture is not ensured by regulatory
controls as a precursor to deployment and use.
This Technical Report applies to deployment and use to which such regulatory controls do not apply.
Nevertheless, ensuring safe deployment and use of health software is greatly assisted if the software's
manufacture has been conducted in conformance with relevant standards within or without the regulatory
environment (see 4.1).
A necessary pre-cursor for determining and implementing controls to minimize risks to patients, from a health
software systems that is manufactured and then deployed and used within a health organization, is a clear
understanding of the risks which the deployed system might present to patients if malfunction or an
unintended event were to occur, and the likelihood of such a malfunction or event causing harm to the patient.
Additionally, if guidance is to be given to deployers and users of health software products then it will need to
be recognised that the controls necessary for products presenting low risks are unlikely to be the same, or
applied with the same rigour, as for those presenting high risks. The controls that are selected need to match
both the level and types of risk that a product might present to a patient when deployed.
What control measures might be necessary for the safety of health software has been considered by
[11]
CEN/TC 251 in EN TR 15640 . The latter contains eleven conclusions which are reproduced in Annex B.
Conclusion 10 reads:
“Standards for ensuring the safety of health software in the user environment should be addressed.”
In the document “Measures for ensuring patient safety of health software (APSOHIP): Proposed next
[19]
steps” , CEN/TC251 considered this conclusion a priority. This Technical Report addresses that conclusion.
[33]
A companion Technical Specification ISO/TS 29321 provides processes and other mechanisms for use by
health software product manufacturers, whether these be commercial entities or internal providers. Users of
this Technical Report can, and should, place a greater degree of reliance upon commercial health software
products that are manufactured and provided to them in accordance with ISO/TS 29321, than those that are
not.
Relationship to Medical Devices
[13]
ISO 14971 is widely used throughout the world for compliance with medical device manufacturing safety
regulations. Such regulations for medical devices in most countries encompass software that is necessary for
the proper application of a medical device or software that is an accessory to a medical device. In some
jurisdictions, regulations also cover some other software. Thus medical device manufacturers have
considerable experience in the application of ISO 14971 and many manufacturers, particularly of electrical
medical devices, are now also involved in the manufacture of health software and it can be reasonably
assumed that their approach to patient safety will be equally applicable to health software.
It is clearly advantageous to manufacturers, any future regulators of health software, and especially to those
deploying and using such software, if the standard for the application of risk management to health software
bears as close a relationship as practicable to ISO 14971. This may in particular be an advantage in
circumstances where software that is part of a medical device complying with ISO 14971 or ISO/TS 29321,
interacts with software not controlled as a medical device but compliant with this Technical Report. Each may
contribute a hazard to the other and thus access to the risk information for both may be necessary.
For these reasons this Technical Report takes as its baseline ISO/TS 29321, that in turn was based upon
ISO 14971 for the same reasons. As far as practicable and appropriate the layout and requirements of the
main text of ISO 14971 have been retained in both this Technical Report and in ISO/TS 29321. As most of the
annexes to ISO 14971 are clearly not applicable to health software, and especially to its deployment and use,
these have been replaced or amended as appropriate.
© ISO 2008 – All rights reserved PROOF/ÉPREUVE vii
---------------------- Page: 7 ----------------------
TECHNICAL REPORT ISO/TR 29322:2008(E)
Health informatics — Guidance on the management of clinical
risk relating to the deployment and use of health software
systems
1 Scope
This Technical Report considers the risk management processes required to ensure patient safety in respect
to the deployment and use of health software products either as a new system within a health organization or
as changes to an existing system's environment.
It is addressed to those persons in health organizations who are responsible for ensuring the safety of health
software in health organizations through the application of risk management (“the responsible person” – see
definition 2.31). Whilst it is therefore principally addressed to healthcare organizations, it will also prove a
useful reference to those involved in the manufacture of health software products. Equally, readers of this
[33]
Technical Report are recommended also to review ISO/TS 29321 (see 4.1).
NOTE 1 The overall life cycle of a health software system includes its concept realization, design, production,
deployment, use and eventual decommissioning. This Technical Report provides guidance to the responsible person for
the application of risk management to the last three stages of the life cycle whereas the manufacturer is responsible for
the first three stages (by applying ISO/TS 29321). As discussed in 4.1, it is recognised that, depending upon contractual
conditions, the manufacturer may be involved in deployment and, in some circumstances, in use and decommissioning.
However, the basic processes recommended in this Technical Report are the same as those required of a manufacturer in
ISO/TS 29321 so the same processes can be applied throughout and should essentially be applied with the responsible
person and manufacturers working together whenever possible. These matters are addressed further in Clause 4.
NOTE 2 Throughout this document the term “clinical” is used to make clear that the scope is limited to matters of risks
to patient safety as distinct from other types of risk such as financial. The use of the term “clinical” should not be taken to
mean that the persons involved in deployment and use are expected to be involved in clinical decisions affecting the
treatment of patients in the direct clinical settings, unless this is consistent with some other aspect of their duties. This
Technical Report however, makes clear that the assessment of risks to patients in the deployment and use of health
software, and in decisions taken about those risks, needs to involve appropriate, experienced and knowledgeable
clinicians.
NOTE 3 Failures and deficiencies in software products used in the health environment can, of course, have adverse
impacts other than causing harm to patients. They may, for example, create administrative inconvenience with a range of
impacts on the organization, including financial loss. Harm to a patient may also have a consequent impact on the
organization such as loss of reputation and financial loss resulting from litigation. Whereas these adverse organizational
impacts will be significant to an organization they are not the subject of this document unless they can result in harm to a
patient. It is the potential harm to the patient which is the subject of this document.
NOTE 4 Whereas this document is restricted to health software, the recommended risk analysis should be conducted
within the context of any overall risk management system in place in the health organization and any wider health
information governance processes.
NOTE 5 This document is restricted to health software but the risk management processes can readily be applied to
hardware on which the software runs.
© ISO 2008 – All rights reserved PROOF/ÉPREUVE 1
---------------------- Page: 8 ----------------------
ISO/TR 29322:2008(E)
2 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
2.1
clinical hazard
potential source of harm to a patient
[ISO/IEC Guide 51:1999, definition 3.5]
2.2
clinical risk
combination of the likelihood of occurrence of harm to a patient and the severity of that harm
NOTE Adapted from ISO/IEC Guide 51:1999 (definition 3.2).
2.3
clinical risk analysis
systematic use of available information to identify and estimate a risk
NOTE Adapted from ISO/IEC Guide 51:1999 (definition 3.10).
2.4
clinical risk assessment
overall process comprising a clinical risk analysis and a clinical risk evaluation
[ISO/IEC Guide 51:1999, definition 3.12]
2.5
clinical risk control
process in which decisions are made and measures implemented by which clinical risks are reduced to, or
maintained within, specified levels
2.6
clinical risk estimation
process used to assign values to the likelihood of occurrence of harm to a patient and the severity of that
harm
2.7
clinical risk evaluation
process of comparing the estimated clinical risk against given risk criteria to determine the acceptability of the
clinical risk
2.8
clinical risk management
systematic application of management policies, procedures and practices to the tasks of analysing, evaluating
and controlling clinical risk
2.9
clinical risk management file
repository of all records and other documents that are produced by the clinical risk management process
2.10
clinical safety
freedom from unacceptable clinical risk to patients
NOTE Adapted from ISO/IEC Guide 51:1999 (definition 3.1).
2 PROOF/ÉPREUVE © ISO 2008 – All rights reserved
---------------------- Page: 9 ----------------------
ISO/TR 29322:2008(E)
2.11
clinical safety case
accumulation, through the life cycle of the health software system, of product and business process
documentation and of evidence structured such as to enable a safety argument to be developed to provide a
compelling, comprehensible and valid case that a system is, as far as the clinical risk management process
can realistically ascertain, free from unacceptable clinical risk for its intended use
2.12
clinical safety case report
report that summarises the arguments and supporting evidence of the clinical safety case at a defined point in
the health software's life cycle
2.13
clinical safety management system
organizational structure, processes, procedures and methodologies that enable the direction and control of the
activities necessary to meet clinical safety requirements and clinical safety policy objectives
2.14
harm
death, physical injury and/or damage to the health or well-being of a patient
NOTE Adapted from ISO/IEC Guide 51:1999.
2.15
hazardous situation
circumstance in which a patient is exposed to one or more hazard(s)
NOTE Adapted from ISO/IEC Guide 51:1999 (definition 3.6).
2.16
health organization
organization within which health software is deployed or used for a health purpose
2.17
health software product
software product for use in the health sector for health related purposes
NOTE A software product will typically be part of a system.
2.18
health software system
one or more software products from one or more manufacturers who operate together to support a health
purpose
2.19
intended use
use of a product, process or service in accordance with the specifications, instructions and information
provided by the manufacturer to customers
NOTE Information provided should contain references to the specific usages and environment to which the health
software product, as part of a system, is intended to be put.
2.20
life cycle
all phases in the life of a health software product, from the initial conception to final decommissioning and
disposal
© ISO 2008 – All rights reserved PROOF/ÉPREUVE 3
---------------------- Page: 10 ----------------------
ISO/TR 29322:2008(E)
2.21
manufacturer
natural or legal person with responsibility for the design, manufacture, packaging or labelling of a health
software product, assembling a system, or adapting a health software system before it is placed on the market
and/or put into service, regardless of whether these operations are carried out by that person or on that
person's behalf by a third party
2.22
medical device
any instrument, apparatus, implement, machine, a
...
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.