ISO 23500-5:2024
(Main)Preparation and quality management of fluids for haemodialysis and related therapies — Part 5: Quality of dialysis fluid for haemodialysis and related therapies
Preparation and quality management of fluids for haemodialysis and related therapies — Part 5: Quality of dialysis fluid for haemodialysis and related therapies
This document specifies the minimum chemical and microbiological quality requirements for dialysis fluids used in haemodialysis and related therapies. This document applies to — dialysis fluids used for haemodialysis and haemodiafiltration, — substitution fluid produced online for haemodiafiltration and haemofiltration based on dialysis fluid This document does not apply to — the water and concentrates used to prepare dialysis fluid or the equipment to produce dialysis fluid — sorbent-based dialysis fluid regeneration systems that regenerate and recirculate small volumes of dialysis fluid, — systems for continuous renal replacement therapy that use pre-packaged solutions, and — systems and solutions for peritoneal dialysis. The delivery and monitoring of the dialysis fluid composition and its permitted deviation from set points is governed by protective systems defined in IEC 60601-2-16.
Préparation et management de la qualité des liquides d'hémodialyse et de thérapies annexes — Partie 5: Qualité des liquides de dialyse pour hémodialyse et thérapies apparentées
Le présent document spécifie les exigences minimales de qualité chimique et microbiologique pour les liquides de dialyse dans le cadre d’hémodialyses et de thérapies apparentées. Le présent document s’applique à ce qui suit: — les liquides de dialyse utilisés à des fins d’hémodialyse et d’hémodiafiltration; — le liquide de substitution produit en ligne à des fins d’hémodiafiltration et d’hémofiltration sur la base du liquide de dialyse. Le présent document ne s’applique pas à ce qui suit: — l’eau et les concentrés utilisés pour préparer le liquide de dialyse ou l’équipement permettant de produire du liquide de dialyse; — les systèmes de régénération de liquide de dialyse à base de sorbants qui régénèrent et recyclent de petites quantités de liquide de dialyse; — les systèmes d’épuration extrarénale continue qui utilisent des solutions prêtes à l’emploi; et — les systèmes et solutions utilisés en dialyse péritonéale. La fourniture et la surveillance de la composition du liquide de dialyse et ses écarts admis par rapport aux points de consigne sont régis par des systèmes de protection définis dans l’IEC 60601-2-16.
General Information
- Status
- Published
- Publication Date
- 16-Apr-2024
- Technical Committee
- ISO/TC 150/SC 2 - Cardiovascular implants and extracorporeal systems
- Drafting Committee
- ISO/TC 150/SC 2 - Cardiovascular implants and extracorporeal systems
- Current Stage
- 9092 - International Standard to be revised
- Start Date
- 13-Oct-2025
- Completion Date
- 12-Feb-2026
Relations
- Effective Date
- 09-Feb-2026
- Effective Date
- 09-Feb-2026
- Effective Date
- 12-Feb-2026
- Effective Date
- 06-Jun-2022
Overview
ISO 23500-5:2024 - Preparation and quality management of fluids for haemodialysis and related therapies - Part 5: Quality of dialysis fluid for haemodialysis and related therapies defines minimum chemical and microbiological quality requirements for dialysis fluids. It covers dialysis fluid used in haemodialysis and haemodiafiltration and online-produced substitution fluid based on dialysis fluid. The standard complements ISO 23500-3 (water) and ISO 23500-4 (concentrates) and interfaces with equipment safety and monitoring requirements in IEC 60601-2-16.
Key topics and requirements
- Microbiological quality
- Standard dialysis fluid: total viable microbial count < 100 CFU/ml and endotoxin < 0.5 EU/ml.
- Ultrapure dialysis fluid: total viable microbial count < 0.1 CFU/ml and endotoxin < 0.03 EU/ml.
- Action levels: recommended (typically ~50% of maximum allowable) to trigger corrective measures such as disinfection and retesting.
- Online substitution fluid: must be sterile and nonpyrogenic; production systems (e.g., ultrafiltration with validated bacteria- and endotoxin-retentive filters) require validation and ongoing surveillance.
- Chemical composition and contaminants
- Dialysis fluid shall be prepared from water and acid/bicarbonate concentrates that meet ISO 23500-3 and ISO 23500-4.
- Delivery systems and materials must not leach chemical contaminants; trace element and heavy metal limits (referenced in Annex B) are specified.
- Testing and conformity
- Guidance on sampling (e.g., aseptic capture at the dialyser inlet or sampling ports), microbiological culture methods, endotoxin testing (including updated alternatives), and chemical analyses are provided.
- Where validated bacteria-/endotoxin-retentive filters are used and operated per manufacturer instructions, routine microbial testing may be waived unless specified by the manufacturer.
Practical applications
- Ensures patient safety by minimizing exposure to biological and chemical contaminants in dialysis fluid.
- Supports clinical protocols for routine surveillance, disinfection, and corrective actions in dialysis centers.
- Informs validation and commissioning of online substitution fluid systems for haemodiafiltration and haemofiltration.
- Guides laboratory testing strategies (microbiology, endotoxin, trace metals) and sampling procedures used by clinical labs and hospital quality teams.
Who uses this standard
- Nephrologists and physicians responsible for dialysis therapy
- Dialysis facility managers and infection-control teams
- Clinical engineers and biomedical technicians
- Medical device manufacturers of dialysis machines, filters and central delivery systems
- Regulatory and accreditation bodies
Related standards
- ISO 23500-1 - General requirements for preparation and quality management of dialysis fluids
- ISO 23500-3 - Quality of water for haemodialysis
- ISO 23500-4 - Concentrates for haemodialysis
- IEC 60601-2-16 - Safety/monitoring for haemodialysis equipment
Keywords: ISO 23500-5:2024, dialysis fluid quality, haemodialysis, ultrapure dialysis fluid, microbiological requirements, chemical contaminants, online substitution fluid, dialysis fluid testing.
ISO 23500-5:2024 - Preparation and quality management of fluids for haemodialysis and related therapies — Part 5: Quality of dialysis fluid for haemodialysis and related therapies Released:17. 04. 2024
REDLINE ISO 23500-5:2024 - Preparation and quality management of fluids for haemodialysis and related therapies — Part 5: Quality of dialysis fluid for haemodialysis and related therapies Released:4/17/2024
ISO 23500-5:2024 - Préparation et management de la qualité des liquides d'hémodialyse et de thérapies annexes — Partie 5: Qualité des liquides de dialyse pour hémodialyse et thérapies apparentées Released:17. 04. 2024
Get Certified
Connect with accredited certification bodies for this standard

BSI Group
BSI (British Standards Institution) is the business standards company that helps organizations make excellence a habit.

TÜV Rheinland
TÜV Rheinland is a leading international provider of technical services.

TÜV SÜD
TÜV SÜD is a trusted partner of choice for safety, security and sustainability solutions.
Sponsored listings
Frequently Asked Questions
ISO 23500-5:2024 is a standard published by the International Organization for Standardization (ISO). Its full title is "Preparation and quality management of fluids for haemodialysis and related therapies — Part 5: Quality of dialysis fluid for haemodialysis and related therapies". This standard covers: This document specifies the minimum chemical and microbiological quality requirements for dialysis fluids used in haemodialysis and related therapies. This document applies to — dialysis fluids used for haemodialysis and haemodiafiltration, — substitution fluid produced online for haemodiafiltration and haemofiltration based on dialysis fluid This document does not apply to — the water and concentrates used to prepare dialysis fluid or the equipment to produce dialysis fluid — sorbent-based dialysis fluid regeneration systems that regenerate and recirculate small volumes of dialysis fluid, — systems for continuous renal replacement therapy that use pre-packaged solutions, and — systems and solutions for peritoneal dialysis. The delivery and monitoring of the dialysis fluid composition and its permitted deviation from set points is governed by protective systems defined in IEC 60601-2-16.
This document specifies the minimum chemical and microbiological quality requirements for dialysis fluids used in haemodialysis and related therapies. This document applies to — dialysis fluids used for haemodialysis and haemodiafiltration, — substitution fluid produced online for haemodiafiltration and haemofiltration based on dialysis fluid This document does not apply to — the water and concentrates used to prepare dialysis fluid or the equipment to produce dialysis fluid — sorbent-based dialysis fluid regeneration systems that regenerate and recirculate small volumes of dialysis fluid, — systems for continuous renal replacement therapy that use pre-packaged solutions, and — systems and solutions for peritoneal dialysis. The delivery and monitoring of the dialysis fluid composition and its permitted deviation from set points is governed by protective systems defined in IEC 60601-2-16.
ISO 23500-5:2024 is classified under the following ICS (International Classification for Standards) categories: 11.040.40 - Implants for surgery, prosthetics and orthotics. The ICS classification helps identify the subject area and facilitates finding related standards.
ISO 23500-5:2024 has the following relationships with other standards: It is inter standard links to EN ISO 23500-1:2024, EN ISO 23500-4:2024, EN ISO 23500-5:2024, ISO 23500-5:2019. Understanding these relationships helps ensure you are using the most current and applicable version of the standard.
ISO 23500-5:2024 is available in PDF format for immediate download after purchase. The document can be added to your cart and obtained through the secure checkout process. Digital delivery ensures instant access to the complete standard document.
Standards Content (Sample)
International
Standard
ISO 23500-5
Second edition
Preparation and quality
2024-04
management of fluids for
haemodialysis and related
therapies —
Part 5:
Quality of dialysis fluid for
haemodialysis and related therapies
Préparation et management de la qualité des liquides
d'hémodialyse et de thérapies annexes —
Partie 5: Qualité des liquides de dialyse pour hémodialyse et
thérapies apparentées
Reference number
© ISO 2024
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
Contents Page
Foreword .iv
Introduction .v
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 1
4 Requirements . 2
4.1 Microbiological contaminants in dialysis fluid .2
4.1.1 General .2
4.1.2 Microbiological requirements for standard dialysis fluid .2
4.1.3 Microbiological requirements for ultrapure dialysis fluid .2
4.1.4 Microbiological requirements for online prepared substitution fluid .2
4.2 Chemical composition of dialysis fluid .3
4.3 Chemical contaminants in dialysis fluid .3
5 Tests for conformity . 3
5.1 Microbiological requirements.3
5.1.1 Sampling .3
5.1.2 Culture methods .3
5.2 Chemical requirements . .5
Annex A (informative) Rationale for the development and provisions of this document . 6
Annex B (informative) Reference tables . 9
Bibliography .11
iii
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out through
ISO technical committees. Each member body interested in a subject for which a technical committee
has been established has the right to be represented on that committee. International organizations,
governmental and non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely
with the International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are described
in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the different types
of ISO document should be noted. This document was drafted in accordance with the editorial rules of the
ISO/IEC Directives, Part 2 (see www.iso.org/directives).
ISO draws attention to the possibility that the implementation of this document may involve the use of (a)
patent(s). ISO takes no position concerning the evidence, validity or applicability of any claimed patent
rights in respect thereof. As of the date of publication of this document, ISO had not received notice of (a)
patent(s) which may be required to implement this document. However, implementers are cautioned that
this may not represent the latest information, which may be obtained from the patent database available at
www.iso.org/patents. ISO shall not be held responsible for identifying any or all such patent rights.
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and expressions
related to conformity assessment, as well as information about ISO's adherence to the World Trade
Organization (WTO) principles in the Technical Barriers to Trade (TBT), see www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 150, Implants for surgery, Subcommittee
SC 2, Cardiovascular implants and extracorporeal systems, in collaboration with the European Committee for
Standardization (CEN) Technical Committee CEN/TC 205, Non-active medical devices, in accordance with the
Agreement on technical cooperation between ISO and CEN (Vienna Agreement).
This second edition cancels and replaces the first edition (ISO 23500-5:2019), which has been technically
revised.
The main changes are: alternatives to classic microbial analytical methods [endotoxin testing using rFC (tp)]
have been incorporated.
A list of all parts of the ISO 23500 series can be found on the ISO website.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
iv
Introduction
Haemodialysis patients are directly exposed to large volumes of dialysis fluid, with the dialyser membrane
being the only barrier against transfer of hazardous contaminants from the dialysis fluid to the patient. It has
long been known that there can be hazardous contaminants in the water and concentrates used to prepare
the dialysis fluid. To minimize this hazard, ISO 23500-3 and ISO 23500-4 set forth quality requirements
for the water and concentrates used to prepare dialysis fluid. However, if the dialysis fluid is not prepared
carefully, it can contain unacceptable levels of contaminants even though it is prepared from water and
concentrates, conforming to the requirements of ISO 23500-3 and ISO 23500-4. Further, the dialysis fluid
can be used as the starting material for the online preparation of fluids intended for infusion into the
patient, for example, in therapies such as online haemodiafiltration. For these reasons, this document was
developed to complement the existing International Standards for water and concentrates, ISO 23500-3 and
ISO 23500-4, respectively. Guidelines to aid the user in routinely meeting the requirements of this document
and ISO 23500-3 can be found in ISO 23500-1.
Within these International Standards, measurement techniques current at the time of preparation have been
cited. Other standard methods can be used, provided that such methods have been appropriately validated
and are comparable to the cited methods. The rationale for the development of this document is given in
Annex A.
This document reflects the conscientious efforts of healthcare professionals, patients and medical device
manufacturers to develop recommendations for the quality of dialysis fluid. This document is applicable to
healthcare professionals involved in the management of dialysis facilities and the routine care of patients
treated in dialysis facilities, since they are responsible for the final preparation of dialysis fluid.
This document aims to help protect haemodialysis patients from adverse effects arising from known
chemical and microbiological contaminants that can be found in improperly prepared dialysis fluid.
However, the physician in charge of dialysis has the ultimate responsibility for ensuring that the dialysis
fluid is correctly formulated and meets the applicable quality standards.
The concepts incorporated in this document should not be considered inflexible or static. The requirements
and recommendations presented in this document should be reviewed periodically in order to assimilate
increased understanding of the role of dialysis fluid purity in patient outcomes and technological
developments.
v
International Standard ISO 23500-5:2024(en)
Preparation and quality management of fluids for
haemodialysis and related therapies —
Part 5:
Quality of dialysis fluid for haemodialysis and related
therapies
1 Scope
This document specifies the minimum chemical and microbiological quality requirements for dialysis fluids
used in haemodialysis and related therapies.
This document applies to
— dialysis fluids used for haemodialysis and haemodiafiltration,
— substitution fluid produced online for haemodiafiltration and haemofiltration based on dialysis fluid
This document does not apply to
— the water and concentrates used to prepare dialysis fluid or the equipment to produce dialysis fluid
— sorbent-based dialysis fluid regeneration systems that regenerate and recirculate small volumes of
dialysis fluid,
— systems for continuous renal replacement therapy that use pre-packaged solutions, and
— systems and solutions for peritoneal dialysis.
The delivery and monitoring of the dialysis fluid composition and its permitted deviation from set points is
governed by protective systems defined in IEC 60601-2-16.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content constitutes
requirements of this document. For dated references, only the edition cited applies. For undated references,
the latest edition of the referenced document (including any amendments) applies.
ISO 23500-1, Preparation and quality management of fluids for haemodialysis and related therapies — Part 1:
General requirements
ISO 23500-3, Preparation and quality management of fluids for haemodialysis and related therapies — Part 3:
Quality of water for haemodialysis and related therapies
ISO 23500-4, Preparation and quality management of fluids for haemodialysis and related therapies — Part 4:
Concentrates for haemodialysis and related therapies
3 Terms and definitions
For the purposes of this document, the terms and definitions given in ISO 23500-1 apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
4 Requirements
4.1 Microbiological contaminants in dialysis fluid
4.1.1 General
The requirements contained in Clause 4 apply to a sample of the dialysis fluid collected at the inlet to the
dialyser or the reinfusion point.
4.1.2 Microbiological requirements for standard dialysis fluid
Standard dialysis fluid shall contain a total viable microbial count of less than 100 CFU/ml (when tested in
accordance with Clause 5) and an endotoxin concentration of less than 0,5 EU/ml (when tested in accordance
with Clause 5).
Action levels for the total viable microbial count and endotoxin concentration in dialysis fluid should also be
set based on knowledge of the microbial dynamics of the system. Typically, the action levels are set at 50 %
of the maximum allowable levels for total viable microbial count and endotoxin; other levels can be set.
If microbial counts exceeding the action levels are observed in the dialysis fluid, corrective measures, such
as disinfection and retesting, should be taken promptly to reduce the levels.
Associated with the presence of bacteria and endotoxin in dialysis fluid is the likely presence of fungi (yeasts
and filamentous fungi).
Tests for microbial growth and endotoxins are not required if the dialysis machine fluid pathway is fitted
with an appropriate capacity bacteria-retentive and endotoxin-retentive filter validated by the manufacturer,
and operated and surveyed according to the manufacturer's instructions, unless the manufacturer requires
such tests in the instructions for use.
4.1.3 Microbiological requirements for ultrapure dialysis fluid
Ultrapure dialysis fluid shall contain a total viable microbial count of less than 0,1 CFU/ml (when tested in
accordance with Clause 5) and an endotoxin concentration less than 0,03 EU/ml (when tested in accordance
with Clause 5). If those limits are exceeded in ultrapure dialysis fluid, corrective measures should be taken to
reduce the levels to an acceptable level. The user is responsible for surveying the dialysis fluid bacteriology
of the system following installation. It is incumbent on the user to establish a regular surveillance routine.
Tests for microbial growth and endotoxins are not required if the dialysis machine fluid pathway is fitted
with an appropriate capacity bacteria-retentive and endotoxin-retentive filter validated by the manufacturer,
and operated and surveyed according to the manufacturer's instructions, unless the manufacturer requires
such tests in the instructions for use.
4.1.4 Microbiological requirements for online prepared substitution fluid
The requirements contained in this subclause apply to online prepared fluid intended to be infused into the
patient as it enters the patient's blood.
This fluid shall be sterile and nonpyrogenic.
Substitution fluid for convective therapies, such as haemodiafiltration and haemofiltration, can be produced
online by a process of ultrafiltration with bacteria- and endotoxin-retentive filters. This online process shall
be validated to produce fluid that is sterile and nonpyrogenic.
Conformity of online produced fluid with the requirements of this document cannot be demonstrated with
traditional test procedures. For this reason, conformity with this document shall be ensured by proper
operation of a validated system, verified in accordance with the manufacturer's instructions at the time
of installation, and confirmed by the user with a regular surveillance and maintenance schedule. The user
shall follow the manufacturer’s instructions for use of the validated system and the user’s surveillance and
maintenance schedule shall be designed to confirm that the water and concentrates used to prepare the
substitution fluid continue to meet the specifications of ISO 23500-3 and ISO 23500-4.
4.2 Chemical composition of dialysis fluid
Dialysis fluid shall be prepared from water meeting the requirements of ISO 23500-3 and acid and
bicarbonate concentrates meeting the requirements of ISO 23500-4. The water and concentrates shall be
combined in accordance with the concentrate manufacturers dilution instructions using individual dialysis
fluid delivery systems as specified in IEC 60601-2-16 or a central dialysis fluid delivery system.
4.3 Chemical contaminants in dialysis fluid
The water and concentrates shall be combined using individual dialysis fluid delivery systems or a central
dialysis fluid delivery system constructed from materials that do not contribute chemical contaminants to
the final dialysis fluid.
The maximum levels of chemical contaminants permitted in water used to prepare dialysis fluid and
concentrates are given in ISO 23500-3 and are also shown in Annex B (see Tables B.1 and B.2) together with
methods of determination (see Table B.3). Other equivalent analytical methods can be used. Where testing
for the individual trace elements listed in Table B.2 is not available, an analysis for total heavy metals can be
used with a maximum allowable level of 0,1 mg/l.
5 Tests for conformity
5.1 Microbiological requirements
5.1.1 Sampling
In some newer dialysis machines, dialysis fluid flow stops when the effluent line is disconnected from
the dialyser. In these instances, the machines are equipped with dialysis fluid sampling ports that can be
accessed using a syringe. Sample ports can be disinfected with alcohol and allowed to air-dry. A sterile
syringe should be used to aspirate at least 10 ml of dialysis fluid out of the sampling port. The filled syringe
is discarded and a fresh sample of dialysis fluid collected using a new sterile syringe. For sample ports
consisting of a simple septum penetrated with a needle, the use of a second syringe is not necessary. If no
sampling port is available and if the dialysis machine permits, samples can be collected immediately before
the dialyser by disconnecting the inlet connector and aseptically collecting a “free/clean” catch sample after
allowing dialysis fluid to run for at least 60 s unless manufacturers’ instructions state otherwise.
Microbial analysis of any fluid sample should be conducted as soon as possible after collection to avoid
unpredictable changes in the microbial population. If samples cannot be analysed within 4 h of collection,
they should be stored at <10 °C without freezing and during transit to the laboratory. Sample storage for
more than 24 h should be avoided and sample shipping should be according to the laboratory’s instructions.
5.1.2 Culture methods
Accurate microbiological surveillance is important in the indication of the microbial content of dialysis water
and dialysis fluid. Culture results obtained using the methods outlined in this document and summarized in
Table 1 are only a relative indicator of the bioburden and do not provide an absolute measure of the absolute
microbial burden.
Total viable microbial counts (standard plate counts) shall be obtained using conventional microbiological
assay procedures (pour plate, spread plate, membrane filter techniques). The calibrated loop technique shall
not be used.
Preferred methods and sample volumes are:
— for standard dialysis fluid:
— spread plate, 0,1 ml to 0,3 ml;
— pour plate, typically 1 ml;
— for ultrapure dialysis fluid: membrane filtration, 10 ml to 1 000 ml;
— for substitution fluid: sterility cannot be proven by sampling.
Different media types and incubation periods can result in varying colony concentrations and types of
microorganisms recovered.
The use of Reasoner’s 2A agar (R2A) has been shown in published studies to result in higher colony
[20][21]
counts than tryptic soy agar (TSA) for water and dialysis fluids samples . However, in a more recent
[22]
publication , the authors indicated that there were no significant differences for comparisons of bacterial
burden of standard dialysis water and standard dialysis fluid yielding colony counts ≥50 CFU/ml when
assayed using R2A and TSA at the conditions stated in Table 1.
Tryptone glucose extract agar (TGEA) incubated at 17 °C to 23 °C for a period of 7 d in previous studies also
yielded higher colony counts than TSA. In Reference [22], a comparison of this medium with TSA showed
that the proportion of standard dialysis water samples yielding colony counts ≥50 CFU/ml was significantly
different from that found using TSA at an incubation temperature of 35 °C to 37 °C and an incubation time of
48 h (p = 0,001). The proportions of dialysis fluid samples in which microbial burden was ≥50 CFU/ml were
not significantly different on the two media and incubation conditions.
The culture medium and incubation times selected should be based on the type of fluid to be analysed, for
example, standard dialysis fluid, water used in the preparation of standard dialysis fluid, ultrapure dialysis
fluid, water used for the preparation of ultrapure dialysis fluid or fluid used for on line therapies such as
haemodiafiltration. The method selected should be based on the analysis of the advantages, disadvantages and
sensitivity of each of the suggested methods. It should also ensure that patient safety is safeguarded and allow
for consideration of local laboratory working practices, and that reimbursement requirements can be met.
Blood agar and chocolate agar shall not be used.
Table 1 — Culture techniques
Culture medium Incubation temperature Incubation time
TGEA 17 °C to 23 °C 7 d
R2A 17 °C to 23 °C 7 d
a
TSA 35 °C to 37 °C 48 h
a [22]
The use of TSA has only been validated for dialysis water and standard dialysis fluid .
Other medium, incubation conditions and colony counting times can be used provided it has been
demonstrated that such methods have been appropriately validated and are comparable to the cited
methods.
Currently there are no requirements for routine surveillance for the presence of fungi (i.e. yeasts and
filamentous fungi), however if quantification is required, membrane filtration is suggested as the method
for obtaining a sample suitable for analysis. For culture, Sabouraud or malt extract agar (MEA) are
recommended.
The detection of bacterial endotoxins, which originate from gram-negative bacteria, is mainly carried out
using Limulus amoebocyte lysate (LAL), which is obtained from horseshoe crab blood (Limulus polyphemus
or Tachypleus tridentatus). The corresponding chapters have been harmonized between the European
[16] [13]
Pharmacopoeia ((EP) <2.6.14>), the Pharmacopoeia of the United States-National Formulary, (<85>)
[19]
and the Japanese Pharmacopoeia (<4.01>) .
The LAL test is based on the humoral coagulation cascade of the horseshoe crab Limulus polyphemus. The
first enzyme in this coagulation cascade reacts with endotoxin and is called Factor C. This factor is now
produced recombinantly (i.e. with biotechnology) and offered as the rFC test by several manufacturers for
the determination of bacterial endotoxins. Compared to the LAL test, the rFC test has proven to be at least
as sensitive and reliable, but less susceptible to certain interfering factors and b
...
International
Standard
Redline version
compares Second edition
to First edition
ISO 23500-5
Preparation and quality
management of fluids for
haemodialysis and related
therapies —
Part 5:
Quality of dialysis fluid for
haemodialysis and related therapies
Préparation et management de la qualité des liquides
d'hémodialyse et de thérapies annexes —
Partie 5: Qualité des liquides de dialyse pour hémodialyse et
thérapies apparentées
Reference number
ISO 23500-5:redline:2024(en) © ISO 2024
ISO 23500-5:redline:2024(en)
IMPORTANT — PLEASE NOTE
This is a provisional mark-up copy and uses the following colour coding:
Text example 1 — indicates added text (in green)
— indicates removed text (in red)
Text example 2
— indicates added graphic figure
— indicates removed graphic figure
1.x . — Heading numbers containg modifications are highlighted in yellow in
the Table of Contents
All changes in this document have yet to reach concensus by vote and as such should only
be used internally for review purposes.
DISCLAIMER
This Redline version is not an official IEC Standard and is intended only to provide the
user with an indication of what changes have been made to the previous version. Only the
current version of the standard is to be considered the official document.
This Redline version provides you with a quick and easy way to compare all the changes
between this standard and its previous edition. A vertical bar appears in the margin
wherever a change has been made. Additions and deletions are displayed in red, with
deletions being struck through.
© ISO 2024
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
ISO 23500-5:redline:2024(en)
Contents Page
Foreword .iv
Introduction .v
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 2
4 Requirements . 2
4.1 Microbiological contaminants in dialysis fluid .2
4.1.1 General .2
4.1.2 Microbiological requirements for standard dialysis fluid .2
4.1.3 Microbiological requirements for ultrapure dialysis fluid .2
4.1.4 Microbiological requirements for online prepared substitution fluid .3
4.2 Chemical composition of dialysis fluid .3
4.2 4.3 Chemical contaminants in dialysis fluid .3
5 Tests for conformity with microbiological requirements . 3
5.1 Sampling .3
5.2 Culture methods.4
5.1 Microbiological requirements.5
5.1.1 Sampling .5
5.1.2 Culture methods .5
5.2 Chemical requirements . .7
Annex A (informative) Rationale for the development and provisions of this document . 8
Annex B (informative) Reference tables .12
Bibliography .16
iii
ISO 23500-5:redline:2024(en)
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out through
ISO technical committees. Each member body interested in a subject for which a technical committee
has been established has the right to be represented on that committee. International organizations,
governmental and non-governmental, in liaison with ISO, also take part in the work. ISO collaborates closely
with the International Electrotechnical Commission (IEC) on all matters of electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are described
in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the different types
of ISO documentsdocument should be noted. This document was drafted in accordance with the editorial
rules of the ISO/IEC Directives, Part 2 (see www .iso .org/ directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of patent
rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of any patent
rights identified during the development of the document will be in the Introduction and/or on the ISO list of
patent declarations received (see www .iso .org/ patents).
ISO draws attention to the possibility that the implementation of this document may involve the use of (a)
patent(s). ISO takes no position concerning the evidence, validity or applicability of any claimed patent rights
in respect thereof. As of the date of publication of this document, ISO had not received notice of (a) patent(s)
which may be required to implement this document. However, implementers are cautioned that this may not
represent the latest information, which may be obtained from the patent database available at www .iso .org/
patents. ISO shall not be held responsible for identifying any or all such patent rights.
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and expressions
related to conformity assessment, as well as information about ISO's adherence to the World Trade
Organization (WTO) principles in the Technical Barriers to Trade (TBT), see www .iso .org/ iso/ foreword .html.
This document was prepared by Technical Committee ISO/TC 150, Implants for surgery, Subcommittee
SC 2, Cardiovascular implants and extracorporeal systems, in collaboration with the European Committee for
Standardization (CEN) Technical Committee CEN/TC 205, Non-active medical devices, in accordance with the
Agreement on technical cooperation between ISO and CEN (Vienna Agreement).
This firstsecond edition cancels and replaces the first edition (ISO 11663:201423500-5:2019), which has
been technically revised. The main changes compared to the previous edition are as follows:
— The document forms part of a revised and renumbered series dealing with the preparation and quality
management of fluids for haemodialysis and related therapies. The series comprise ISO 23500-1
(previously ISO 23500), ISO 23500-2, (previously ISO 26722), ISO 23500-3, (previously ISO 13959),
ISO 23500-4, (previously ISO 13958), and ISO 23500-5, (previously ISO 11663).
The main changes are: alternatives to classic microbial analytical methods [endotoxin testing using rFC (tp)]
have been incorporated.
A list of all parts inof the ISO 23500 series can be found on the ISO website.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www .iso .org/ members .html.
iv
ISO 23500-5:redline:2024(en)
Introduction
Haemodialysis patients are directly exposed to large volumes of dialysis fluid, with the dialyser membrane
being the only barrier against transfer of hazardous contaminants from the dialysis fluid to the patient.
It has long been known that there couldcan be hazardous contaminants in the water and concentrates
used to prepare the dialysis fluid. To minimize this hazard, ISO 23500-3 and ISO 23500-4 set forth quality
requirements for the water and concentrates used to prepare dialysis fluid. However, if the dialysis fluid is
not prepared carefully, it couldcan contain unacceptable levels of contaminants even though it is prepared
from water and concentrates, conforming to the requirements of ISO 23500-3 and ISO 23500-4. Further,
the dialysis fluid mightcan be used as the starting material for the online preparation of fluids intended for
infusion into the patient, for example, in therapies such as online haemodiafiltration. For these reasons, this
document for dialysis fluid quality was developed to complement the existing International Standards for
water and concentrates, ISO 23500-3 and ISO 23500-4, respectively. Guidelines to aid the user in routinely
meeting the requirements of this document and ISO 23500-3 can be found in ISO 23500-1.
Within these International Standards, measurement techniques current at the time of preparation have been
cited. Other standard methods can be used, provided that such methods have been appropriately validated
and are comparable to the cited methods. The rationale for the development of this document is given in
Annex A.
This document reflects the conscientious efforts of healthcare professionals, patients and medical device
manufacturers to develop recommendations for the quality of dialysis fluid. This document is directed at
theapplicable to healthcare professionals involved in the management of dialysis facilities and the routine
care of patients treated in dialysis facilities, since they are responsible for the final preparation of dialysis
fluid. The recommendations contained in this document are not intended for regulatory application.
This document aims to help protect haemodialysis patients from adverse effects arising from known
chemical and microbiological contaminants that can be found in improperly prepared dialysis fluid.
However, the physician in charge of dialysis has the ultimate responsibility for ensuring that the dialysis
fluid is correctly formulated and meets the applicable quality standards.
The concepts incorporated in this document should not be considered inflexible or static. The requirements
and recommendations presented herein this document should be reviewed periodically in order to
assimilate increased understanding of the role of dialysis fluid purity in patient outcomes and technological
developments.
v
ISO 23500-5:redline:2024(en)
Preparation and quality management of fluids for
haemodialysis and related therapies —
Part 5:
Quality of dialysis fluid for haemodialysis and related
therapies
1 Scope
This document specifies minimumthe minimum chemical and microbiological quality requirements for
dialysis fluids used in haemodialysis and related therapies.
This document includes dialysis fluids used for haemodialysis and haemodiafiltration, including substitution
fluid for haemodiafiltration and haemofiltration.
This document excludes the water and concentrates used to prepare dialysis fluid or the equipment used in
its preparation. Those areas are covered by other International Standards.
Sorbent-based dialysis fluid regeneration systems that regenerate and recirculate small volumes of dialysis
fluid, systems for continuous renal replacement therapy that use pre-packaged solutions, and systems and
solutions for peritoneal dialysis are excluded from this document.
This document applies to
— dialysis fluids used for haemodialysis and haemodiafiltration,
— substitution fluid produced online for haemodiafiltration and haemofiltration based on dialysis fluid
This document does not apply to
— the water and concentrates used to prepare dialysis fluid or the equipment to produce dialysis fluid
— sorbent-based dialysis fluid regeneration systems that regenerate and recirculate small volumes of
dialysis fluid,
— systems for continuous renal replacement therapy that use pre-packaged solutions, and
— systems and solutions for peritoneal dialysis.
The delivery and monitoring of the dialysis fluid composition and its permitted deviation from set points is
governed by protective systems defined in IEC 60601-2-16.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content constitutes
requirements of this document. For dated references, only the edition cited applies. For undated references,
the latest edition of the referenced document (including any amendments) applies.
ISO 23500-1, Preparation and quality management of fluids for haemodialysis and related therapies — Part 1:
General requirements
ISO 23500-3, Preparation and quality management of fluids for haemodialysis and related therapies — Part 3:
Quality of water for haemodialysis and related therapies
ISO 23500-5:redline:2024(en)
ISO 23500-4, Preparation and quality management of fluids for haemodialysis and related therapies — Part 4:
Concentrates for haemodialysis and related therapies
3 Terms and definitions
For the purposes of this document, the terms and definitions given in ISO 23500-1 apply.
ISO and IEC maintain terminologicalterminology databases for use in standardization at the following
addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at httphttps:// www .electropedia .org/
4 Requirements
4.1 Microbiological contaminants in dialysis fluid
4.1.1 General
The requirements contained in thisClause 4 clause apply to a sample of the dialysis fluid collected at the
inlet to the dialyser or the reinfusion point.
4.1.2 Microbiological requirements for standard dialysis fluid
Standard dialysis fluid shall contain a total viable microbial count of less than 100 CFU/ml (when tested in
accordance with Clause 5) and an endotoxin concentration of less than 0,5 EU/ml (when tested in accordance
with Clause 5).
Action levels for the total viable microbial count and endotoxin concentration in dialysis fluid should also be
set based on knowledge of the microbial dynamics of the system. Typically, the action levels are set at 50 %
of the maximum allowable levels for total viable microbial count and endotoxin; other levels can be set.
If microbial counts exceeding the action levels are observed in the dialysis fluid, corrective measures, such
as disinfection and retesting, should be taken promptly to reduce the levels.
Associated with the presence of bacteria and endotoxin in dialysis fluid is the likely presence of fungi (yeasts
and filamentous fungi). After extensive discussion, the working group has not recommended maximum
limits, for such contaminants.
Tests for bacterialmicrobial growth and endotoxins are not required if the dialysis machine fluid pathway
is fitted with an appropriate capacity bacteria-retentive and endotoxin-retentive filter validated by the
manufacturer, and operated and surveilledsurveyed according to the manufacturer's instructions, unless
the manufacturer requires such tests in the instructions for use.
4.1.3 Microbiological requirements for ultrapure dialysis fluid
Ultrapure dialysis fluid shall contain a total viable microbial count of less than 0,1 CFU/ml (when tested in
accordance with Clause 5) and an endotoxin concentration less than 0,03 EU/ml (when tested in accordance
with Clause 5). If those limits are exceeded in ultrapure dialysis fluid, corrective measures should be taken
to reduce the levels to an acceptable level. The user is responsible for surveillingsurveying the dialysis
fluid bacteriology of the system following installation. It is incumbent on the user to establish a regular
surveillance routine.
Tests for bacterialmicrobial growth and endotoxins are not required if the dialysis machine fluid pathway
is fitted with an appropriate capacity bacteria-retentive and endotoxin-retentive filter validated by the
manufacturer, and operated and surveilledsurveyed according to the manufacturer's instructions, unless
the manufacturer requires such tests in the instructions for use.
ISO 23500-5:redline:2024(en)
4.1.4 Microbiological requirements for online prepared substitution fluid
The requirements contained in this clausesubclause apply to online prepared fluid intended to be infused
into the patient as it enters the patient's blood.
This fluid shall be sterile and nonpyrogenic.
Substitution fluid for convective therapies, such as haemodiafiltration and haemofiltration, can be produced
online by a process of ultrafiltration with bacteria-retentive and endotoxin-retentive filters. This online
process shall be validated to produce fluid that is sterile and nonpyrogenic.
Conformity of online produced fluid with the requirements of this document cannot be demonstrated with
traditional test procedures. For this reason, conformity with this document shall be ensured by proper
operation of a validated system, verified according toin accordance with the manufacturer's instructions at
the time of installation, and confirmed by the user with a regular surveillance and maintenance schedule. The
user shall follow the manufacturer’s instructions for use of the validated system and the user’s surveillance
and maintenance schedule shall be designed to confirm that the water and concentrates used to prepare the
substitution fluid continue to meet the specifications of ISO 23500-3 and ISO 23500-4.
4.2 Chemical composition of dialysis fluid
Dialysis fluid shall be prepared from water meeting the requirements of ISO 23500-3 and acid and
bicarbonate concentrates meeting the requirements of ISO 23500-4. The water and concentrates shall be
combined in accordance with the concentrate manufacturers dilution instructions using individual dialysis
fluid delivery systems as specified in IEC 60601-2-16 or a central dialysis fluid delivery system.
4.2 4.3 Chemical contaminants in dialysis fluid
Dialysis fluid shall be prepared from water meeting the requirements of ISO 23500-3 and acid and
bicarbonate concentrates meeting the requirements of ISO 23500-4. The water and concentrates shall
be combined using individual dialysis fluid delivery systems or a central dialysis fluid delivery system
constructed from materials that do not contribute chemical contaminants to the final dialysis fluid.
The maximum levels of chemical contaminants permitted in water used to prepare dialysis fluid and
concentrates are given in ISO 23500-3 and are also shown in informative Annex B of this document ((see
Tables B.1 and B.2) together with methods of determination (see Table B.3). Other equivalent analytical
methods can be used. Where testing for the individual trace elements listed in Table B.2 is not available, an
analysis for total heavy metals can be used with a maximum allowable level of at 0,1 mg/l.
5 Tests for conformity with microbiological requirements
5.1 Sampling
In some newer dialysis machines, dialysis fluid flow stops when the effluent line is disconnected from the
dialyser. In these instances, the machines are equipped with dialysis fluid sampling ports that can be accessed
using a syringe. Sample ports can be disinfected with alcohol and allowed to air-dry. A sterile syringe should
be used to aspirate at least 10 ml of dialysis fluid out of the sampling port. The filled syringe is discarded
and a fresh sample of dialysis fluid collected using a new sterile syringe. For sample ports consisting of a
simple septum penetrated with a needle, the use of a second syringe is not necessary. Alternatively, if the
dialysis machine permits, samples can be collected immediately before the dialyser by disconnecting the
inlet connector and aseptically collecting a “free/clean” catch sample after allowing dialysis fluid to run for
at least 60 s unless manufacturers’ instructions state otherwise.
Microbial analysis of any fluid sample should be conducted as soon as possible after collection to avoid
unpredictable changes in the microbial population. If samples cannot be analysed within 4 h of collection,
they should be stored at <10 °C without freezing and during transit to the laboratory. Sample storage for
more than 24 h should be avoided, and sample shipping should be in accordance with the laboratory’s
instructions.
ISO 23500-5:redline:2024(en)
5.2 Culture methods
Accurate microbiological surveillance is important in the indication of the microbial content of dialysis water
and dialysis fluid. Culture results obtained using the methods outlined in this document and summarized in
Table 1 are only a relative indicator of the bioburden and do not provide an absolute measure of the absolute
bacterial burden.
Total viable microbial counts (standard plate counts) shall be obtained using conventional microbiological
assay procedures (pour plate, spread plate, membrane filter techniques). The calibrated loop technique shall
not be used.
Preferred methods and sample volumes:
Standard dialysis fluid:
— spread plate, 0,1 ml to 0,3 ml;
— pour plate, typically 1 ml.
Ultrapure dialysis fluid:
— membrane filtration, 10 ml to 1 000 ml.
Substitution fluid:
— sterility cannot be proven by sampling.
Different media types and incubation periods can result in varying colony concentrations and types of
microorganisms recovered.
The use of Reasoner’s 2A agar (R2A) has been shown in previous studies to result in higher colony counts
[][] []
than tryptic soy agar (TSA) for water and dialysis fluids samples . In a more recent publication, 2016 , the
authors indicated that there were no significant differences for comparisons of bacterial burden of standard
dialysis water and standard dialysis fluid yielding colony counts ≥50 CFU/ml when assayed using R2A and
TSA at the conditions stated in Table 1.
Tryptone glucose extract agar (TGEA) incubated at 17 °C to 23 °C for a period of 7 days in previous studies
[]
also yielded higher colony counts than TSA . Maltais et al. in their comparison of this medium with TSA
showed that the proportion of standard dialysis water samples yielding colony counts ≥50 CFU/ml was
significantly different from that found using TSA at an incubation temperature of 35 °C to 37 °C and an
incubation time of 48 hours (p=0,001). The proportions of dialysis fluid samples in which microbial burden
[]
was ≥50 CFU/ml were not significantly different on the two media and incubation conditions .
The culture medium and incubation times selected should be based on the type of fluid to be analysed
e.g. standard dialysis fluid, water used in the preparation of standard dialysis fluid, ultrapure dialysis
fluid, water used for the preparation of ultrapure dialysis fluid or fluid used for on line therapies such as
haemodiafiltration. The method selected should be based on the analysis of the advantages, disadvantages
and sensitivity of each of the suggested methods. It should also ensure that patient safety is safeguarded and
allow for consideration of local laboratory working practices, and that local regulatory and reimbursement
requirements can be met.
Blood agar and chocolate agar shall not be used.
Table 1 — Culture techniques
Incubation
Culture medium Incubation time
temperature
Tryptone Glucose Extract Agar (TGEA) 17 °C to 23 °C 7 d
Reasoner's agar no. 2 (R2A) 17 °C to 23 °C 7 d
a
Tryptic Soy Agar (TSA) 35 °C to 37 °C 48 h
a
The use of TSA has been only validated for measurement of standard dialysis fluid.
ISO 23500-5:redline:2024(en)
Other medium, incubation conditions and colony counting times can be used provided it has been
demonstrated that such methods have been appropriately validated and are comparable to the cited
methods.
Currently there are no requirements for routine surveillance for the presence of fungi (i.e. yeasts and
filamentous fungi), however if quantification is required, membrane filtration is suggested as the method
for obtaining a sample suitable for analysis. For culture, Sabouraud or Malt Extract Agar (MEA) are
recommended.
The presence of endotoxins shall be determined by a Limulus amoebocyte lysate (LAL) assay or another
validated method.
Conformity with the microbial standards for ultrapure dialysis fluid and substitution fluid prepared online
with a validated system can be met by following the requirements and instructions of the manufacturer of
the dialysis fluid delivery system.
5.1 Microbiological requirements
5.1.1 Sampling
In some newer dialysis machines, dialysis fluid flow stops when the effluent line is disconnected from
the dialyser. In these instances, the machines are equipped with dialysis fluid sampling ports that can be
accessed using a syringe. Sample ports can be disinfected with alcohol and allowed to air-dry. A sterile
syringe should be used to aspirate at least 10 ml of dialysis fluid out of the sampling port. The filled syringe
is discarded and a fresh sample of dialysis fluid collected using a new sterile syringe. For sample ports
consisting of a simple septum penetrated with a needle, the use of a second syringe is not necessary. If no
sampling port is available and if the dialysis machine permits, samples can be collected immediately before
the dialyser by disconnecting the inlet connector and aseptically collecting a “free/clean” catch sample after
allowing dialysis fluid to run for at least 60 s unless manufacturers’ instructions state otherwise.
Microbial analysis of any fluid sample should be conducted as soon as possible after collection to avoid
unpredictable changes in the microbial population. If samples cannot be analysed within 4 h of collection,
they should be stored at <10 °C without freezing and during transit to the laboratory. Sample storage for
more than 24 h should be avoided and sample shipping should be according to the laboratory’s instructions.
5.1.2 Culture methods
Accurate microbiological surveillance is important in the indication of the microbial content of dialysis water
and dialysis fluid. Culture results obtained using the methods outlined in this document and summarized in
Table 1 are only a relative indicator of the bioburden and do not provide an absolute measure of the absolute
microbial burden.
Total viable microbial counts (standard plate counts) shall be obtained using conventional microbiological
assay procedures (pour plate, spread plate, membrane filter techniques). The calibrated loop technique shall
not be used.
Preferred methods and sample volumes are:
— for standard dialysis fluid:
— spread plate, 0,1 ml to 0,3 ml;
— pour plate, typically 1 ml;
— for ultrapure dialysis fluid: membrane filtration, 10 ml to 1 000 ml;
— for substitution fluid: sterility cannot be proven by sampling.
Different media types and incubation periods can result in varying colony concentrations and types of
microorganisms recovered.
ISO 23500-5:redline:2024(en)
The use of Reasoner’s 2A agar (R2A) has been shown in published studies to result in higher colony
[20][21]
counts than tryptic soy agar (TSA) for water and dialysis fluids samples . However, in a more recent
[22]
publication , the authors indicated that there were no significant differences for comparisons of bacterial
burden of standard dialysis water and standard dialysis fluid yielding colony counts ≥50 CFU/ml when
assayed using R2A and TSA at the conditions stated in Table 1.
Tryptone glucose extract agar (TGEA) incubated at 17 °C to 23 °C for a period of 7 d in previous studies also
yielded higher colony counts than TSA. In Reference [22], a comparison of this medium with TSA showed
that the proportion of standard dialysis water samples yielding colony counts ≥50 CFU/ml was significantly
different from that found using TSA at an incubation temperature of 35 °C to 37 °C and an incubation time of
48 h (p = 0,001). The proportions of dialysis fluid samples in which microbial burden was ≥50 CFU/ml were
not significantly different on the two media and incubation conditions.
The culture medium and incubation times selected should be based on the type of fluid to be analysed, for
example, standard dialysis fluid, water used in the preparation of standard dialysis fluid, ultrapure dialysis
fluid, water used for the preparation of ultrapure dialysis fluid or fluid used for on line therapies such as
haemodiafiltration. The method selected should be based on the analysis of the advantages, disadvantages and
sensitivity of each of the suggested methods. It should also ensure that patient safety is safeguarded and allow
for consideration of local laboratory working practices, and that reimbursement requirements can be met.
Blood agar and chocolate agar shall not be used.
Table 1 — Culture techniques
Culture medium Incubation temperature Incubation time
TGEA 17 °C to 23 °C 7 d
R2A 17 °C to 23 °C 7 d
a
TSA 35 °C to 37 °C 48 h
a [22]
The use of TSA has only been validated for dialysis water and standard dialysis fluid .
Other medium, incubation conditions and colony counting times can be used provided it has been
demonstrated that such methods have been appropriately validated and are comparable to the cited
methods.
Currently there are no requirements for routine surveillance for the presence of fungi (i.e. yeasts and
filamentous fungi), however if quantification is required, membrane filtration is suggested as the method
for obtaining a sample suitable for analysis. For culture, Sabouraud or malt extract agar (MEA) are
recommended.
The detection of bacterial endotoxins, which originate from gram-negative bacteria, is mainly carried out
using Limulus amoebocyte lysate (LAL), which is obtained from horseshoe crab blood (Limulus polyphemus
or Tachypleus tridentatus). The corresponding chapters have been harmonized between the European
[16] [13]
Pharmacopoeia ((EP) <2.6.14>), the Pharmacopoeia of the United States-National Formulary, (<85>)
[19]
and the Japanese Pharmacopoeia (<4.01>) .
The LAL test is based on the humoral coagulation cascade of the horseshoe crab Limulus polyphemus. The
first enzyme in this coagulation cascade reacts with endotoxin and is called Factor C. This factor is now
produced recombinantly (i.e. with biotechnology) and offered as the rFC test by several manufacturers for
the determination of bacterial endotoxins. Compared to the LAL test, the rFC test has proven to be at least
as sensitive and reliable, but less susceptible to certain interfering factors and batch fluctuations. Due to
biotechnological production, no live animals are required as blood donors.
[17]
This new method has been incorporated into the European Pharmacopoeia <2.6.32> and will also be
[14]
included into the USP-NF <1085.1> .
Conformity with the microbial standards for ultrapure dialysis fluid and substitution fluid prepared online
with a validated system can be met by following the requirements and instructions of the manufacturer of
the dialysis fluid delivery system.
ISO 23500-5:redline:2024(en)
5.2 Chemical requirements
Conformity with the requirements for the chemical contents of the dialysis fluid is determined by local
regulations or as recommended by the manufacturer of the dialysis fluid delivery system (continuous
surveillance for proportionating systems, see ISO 23500-1).
ISO 23500-5:redline:2024(en)
Annex A
(informative)
Rationale for the development and provisions of this document
A.1 Introduction
The information in this annex is intended to give the reader a historical perspective of the development of
the microbiological and chemical contaminant limits in this document.
A.1 2 Microbiological contaminants in dialysis fluid
NOTE The information in this clause is intended to give the reader a historical perspective of how the microbial
limits were developed for this document.
Pyrogenic reactions are caused by lipopolysaccharides or endotoxins that are associated with gram-negative
bacteria. Furthermore, gram-negative water bacteria have been shown to have the capability of multiplying
rapidly in a variety of hospital-associated fluids, including distilled, deionized, reverse osmosis and softened
water, all of which have been used in the past as supply water for haemodialysis systems. The dialysis fluid,
which is a balanced salt solution made with this water, likewise provides a very good growth medium
for these types of bacteria. Several studies have demonstrated that the incidence of pyrogenic reactions
can be related directly to the number of bacteria in dialysis fluid even at low levels of bacterialmicrobial
contamination, pyrogenic reactions have been reported when the source of endotoxin was exogenous to the
[10][11][12][13]
dialysis system (i.e. present in the community water supply) . The presence of non-tuberculous
mycobacteria has also been associated with outbreaks of infection in dialysis units.
Several investigators have shown that bacteria growing in dialysis fluid can produce products that
[14][15][23]-[25]
cross dialysis membranes . It has also been shown that gram-negative bacteria growing in
dialysis fluid produced endotoxins, that in turn stimulated the production of anti-endotoxin antibodies in
[16][17][25]
haemodialysis patients . These data suggest that endotoxins do indeed cross dialysis membranes,
either intact or as fragments. The use of the very permeable membranes known as high-flux membranes has
raised the possibility of a greater likelihood of passage of endotoxins into the blood path. Several studies
support this contention. Vanholder et al. observed Reference [24] notes an increase in plasma endotoxin
3 4
concentrations during dialysis against dialysis fluid containing 10 CFU/ml to 10 CFU/ml of Pseudomonas
[18]
species . In vitro studies using both radiolabelled lipopolysaccharide and biological assays have
demonstrated that biologically active substances derived from bacteria found in dialysis fluid can cross a
[19] to [25]
variety of dialysis membranes . Also, patients treated with high-flux membranes are reported to have
higher levels of anti-endotoxin antibodies than normal subjects or patients treated with conventional low-
[26]
flux membranes . Finally, it was reported that the use of high-flux dialysers is a significant risk factor for
[27]
pyrogenic reactions . Although other investigators have not been able to demonstrate endotoxin transfer
[28][29]
across dialysis membranes , the preponderance of reports now supports the ability of endotoxin
to transfer across at least some high-flux membranes under some operating conditions. Furthermore,
in a In a Japanese Society for Dialysis Therapy (JSDT) survey, the 1-year mortality rate was significantly
[30][31][26]
higher at facilities with a dialysis fluid endotoxin concentration of >0,100 EU/ml . Consequently,
it seemsseemed prudent to impose an upper limit on the endotoxin content of dialysis water and dialysis
fluid. A level of 2 EU/ml was chosen by AAMI in 2001 as the upper limit for endotoxin, since these levels
were easily achieved with contemporary water treatment systems using reverse osmosis, ultrafiltration, or
both. At the same time, the European Community chose to use 0,25 EU/ml as the maximum allowable level
of endotoxin in dialysis water. When ISO 13959 was revised in 2009, the 0,25 EU/ml limit for dialysis water
was included. In developingDuring the development of this document for dialysis fluid quality, the maximum
allowable level of endotoxin was set at 0,5 EU/ml analysed by the Limulus amebocyte lysate test. The level
is set higher than that for dialysis water in recognition that both the water and concentrates used in the
preparation of dialysis fluid can contribute endotoxins.
ISO 23500-5:redline:2024(en)
The level is set higher than that for dialysis water in recognition that both the water and concentrates used
in the preparation of dialysis fluid can contribute endotoxin.
In addition to the acute risk of pyrogenic reactions, there is increasing indirect evidence that chronic
exposure to low amounts of endotoxin mightcan play a role in some of the long-term complications of
haemodialysis therapy. Patients treated with ultrafilteredultrapure dialysis fluid have demonstrated a
decrease in serum β-microglobulin concentrations, a decrease in markers of an inflammatory response and
oxidant stress, and an increased responsiveness to erythropoietin. In longer term studies, use of ultrafiltered
dialysis fluid has been associated with a decreased incidence of β -microglobulin-associated amyloidosis,
better preservation of residual renal function, and, an improved nutritional status and a decline in renal
[27]-[29][14][17][25][32] to [44]
function .
These observations have led to the recommendation that dialysis fluid of a higher microbiological quality,
[45][29]
so-called “ultrapure” dialysis fluid, should be used for routine haemodialysis . Ultrapure dialysis fluid
is definedspecified as one having a bacterial content of less than 0,1 CFU/ml and an endotoxin content of less
[46]
than 0,03 EU/ml using sensitive assays . This definition is now widely accepted, particularly in Europe,
as the standard for dialysis fluid used to prepare substitution solution for online convective therapies. In
developing. During the development of this document, the desirability of using ultrapure dialysis fluid on a
routine basis was recognized, but it was accepted thatalthough obtaining this level of puritybacterial and
endotoxin content on a routine basis might not yet beis not always feasible in all dialysis settings.
As up to 7 d can elapse between sampling dialysis fluid for the determination of microbiological contamination
and the receipt of results depending on the analytical method used, and because bacterialmicrobial
proliferation can be rapid, action levels for microbial counts were introduced into this document. These
action levels allow the user to initiate corrective action before levels exceed the maximum levels established
byin this document.
In haemodialysis, the net movement of water is from the blood to the dialysis fluid, although within the
dialyser there can be movement of dialysis fluid to the blood due to the phenomenon of back-filtration,
[47]
particularly in dialysers with highly permeable membranes . In contrast, haemofiltration and
haemodiafiltration feature infusions of large volumes of electrolyte solution (20 l to more than 100 l) into the
blood. Increasingly, such solution is being prepared online from ultrapure dialysis fluid. The large volumes
of fluid infused in haemofiltration and haemodiafiltration, and concerns about the transfer of endotoxin and
endotoxin fragments across high-flux membranes, necessitate the use of such fluid to minimize patient risk.
A.2 Chemical contaminants in dialysis fluid
When this document was being developed, the need to include maximum levels for chemical contaminants in
dialysis fluid was discussed. It was proposed that the maximum allowable levels of chemical contaminants
in dialysis fluid should be the same as those in the water used to prepare the dialysis fluid since there
were no data supporting the need for lower levels. Dialysis fluid is prepared from water and concentrates,
meeting the requirements of ISO 23500-3:2019 and ISO 23500-4:2019, including the same requirements for
maximum levels of chemical contaminants that were proposed for inclusion in this document. Because the
water and concentrates are combined using individual dialysis machines or central dialysis fluid delivery
systems that are required to be constructed of materials that do not contribute chemical contaminants to
the dialysis fluid, it was concluded that including maximum allowable levels of chemical contaminants in the
dialysis fluid would be redundant and impose an unnecessary burden on dialysis facilities.
A.3 Tests for conformity with microbiological requirements
The original clinical observations showing a relationship between bacterial levels in dialysis fluid and
pyrogenic reactions were based on cultures performed with standard methods agar (SMA), a medium
[11]
containing relatively few nutrients . Later, the use of tryptic soy agar (TSA)TSA, a general-purpose
medium for isolating and cultivating fastidious organisms was recommended because it was thought more
appropriate for culturing bicarbonate-containing dialysis fluid.
Recommended methods for assaying fluid microbiological content are shown in Table 1. Such methods
provide only a relative indication of the bacterial bioburden rather than an absolute measure. Different media
...
Norme
internationale
ISO 23500-5
Deuxième édition
Préparation et management de la
2024-04
qualité des liquides d'hémodialyse
et de thérapies annexes —
Partie 5:
Qualité des liquides de dialyse
pour hémodialyse et thérapies
apparentées
Preparation and quality management of fluids for haemodialysis
and related therapies —
Part 5: Quality of dialysis fluid for haemodialysis and related
therapies
Numéro de référence
DOCUMENT PROTÉGÉ PAR COPYRIGHT
© ISO 2024
Tous droits réservés. Sauf prescription différente ou nécessité dans le contexte de sa mise en œuvre, aucune partie de cette
publication ne peut être reproduite ni utilisée sous quelque forme que ce soit et par aucun procédé, électronique ou mécanique,
y compris la photocopie, ou la diffusion sur l’internet ou sur un intranet, sans autorisation écrite préalable. Une autorisation peut
être demandée à l’ISO à l’adresse ci-après ou au comité membre de l’ISO dans le pays du demandeur.
ISO copyright office
Case postale 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Genève
Tél.: +41 22 749 01 11
E-mail: copyright@iso.org
Web: www.iso.org
Publié en Suisse
ii
Sommaire Page
Avant-propos .iv
Introduction .v
1 Domaine d’application . 1
2 Références normatives . 1
3 Termes et définitions . 2
4 Exigences . 2
4.1 Contaminants microbiologiques dans le liquide de dialyse .2
4.1.1 Généralités .2
4.1.2 Exigences microbiologiques relatives au liquide de dialyse standard .2
4.1.3 Exigences microbiologiques relatives au liquide de dialyse ultrapur .2
4.1.4 Exigences microbiologiques relatives au liquide de substitution préparé en ligne .3
4.2 Composition chimique du liquide de dialyse .3
4.3 Contaminants chimiques présents dans le liquide de dialyse.3
5 Essais de conformité . 3
5.1 Exigences microbiologiques .3
5.1.1 Échantillonnage.3
5.1.2 Méthodes de culture .4
5.2 Exigences chimiques .5
Annexe A (informative) Justification de l’élaboration et des dispositions du présent document . 6
Annexe B (informative) Tableaux de référence .10
Bibliographie .12
iii
Avant-propos
L'ISO (Organisation internationale de normalisation) est une fédération mondiale d'organismes nationaux
de normalisation (comités membres de l'ISO). L'élaboration des Normes internationales est en général
confiée aux comités techniques de l'ISO. Chaque comité membre intéressé par une étude a le droit de faire
partie du comité technique créé à cet effet. Les organisations internationales, gouvernementales et non
gouvernementales, en liaison avec l'ISO participent également aux travaux. L'ISO collabore étroitement avec
la Commission électrotechnique internationale (IEC) en ce qui concerne la normalisation électrotechnique.
Les procédures utilisées pour élaborer le présent document et celles destinées à sa mise à jour sont
décrites dans les Directives ISO/IEC, Partie 1. Il convient, en particulier, de prendre note des différents
critères d'approbation requis pour les différents types de documents ISO. Le présent document a
été rédigé conformément aux règles de rédaction données dans les Directives ISO/IEC, Partie 2 (voir
www.iso.org/directives).
L’ISO attire l’attention sur le fait que la mise en application du présent document peut entraîner l’utilisation
d’un ou de plusieurs brevets. L’ISO ne prend pas position quant à la preuve, à la validité et à l’applicabilité de
tout droit de brevet revendiqué à cet égard. À la date de publication du présent document, l’ISO n'avait pas
reçu notification qu’un ou plusieurs brevets pouvaient être nécessaires à sa mise en application. Toutefois,
il y a lieu d’avertir les responsables de la mise en application du présent document que des informations
plus récentes sont susceptibles de figurer dans la base de données de brevets, disponible à l'adresse
www.iso.org/brevets. L’ISO ne saurait être tenue pour responsable de ne pas avoir identifié tout ou partie de
tels droits de propriété.
Les appellations commerciales éventuellement mentionnées dans le présent document sont données pour
information, par souci de commodité, à l’intention des utilisateurs et ne sauraient constituer un engagement.
Pour une explication de la nature volontaire des normes, la signification des termes et expressions
spécifiques de l'ISO liés à l'évaluation de la conformité, ou pour toute information au sujet de l'adhésion de
l'ISO aux principes de l’Organisation mondiale du commerce (OMC) concernant les obstacles techniques au
commerce (OTC), voir www.iso.org/avant-propos.
Le présent document a été élaboré par le comité technique ISO/TC 150, Implants chirurgicaux, sous-comité
SC 2, Implants cardiovasculaires et circuits extra-corporels en collaboration avec le comité technique CEN/
TC 205, Dispositifs médicaux non actifs, du Comité européen de normalisation (CEN) conformément à l’Accord
de coopération technique entre l’ISO et le CEN (Accord de Vienne).
Cette deuxième annule et remplace la première édition (ISO 23500-5:2019) qui a fait l’objet d’une révision
technique.
Les principales modifications sont les suivantes: des alternatives aux méthodes d’analyse microbiennes
classiques [analyse des endotoxines au moyen de rFC (tp)] ont été intégrées.
Une liste de toutes les parties de la série ISO 23500 se trouve sur le site web de l’ISO.
Il convient que l’utilisateur adresse tout retour d’information ou toute question concernant le présent
document à l’organisme national de normalisation de son pays. Une liste exhaustive desdits organismes se
trouve à l’adresse www.iso.org/fr/members.html.
iv
Introduction
Les patients sous hémodialyse sont directement exposés à des volumes élevés de liquide de dialyse,
la membrane du dialyseur étant la seule barrière contre le transfert de contaminants dangereux entre le
liquide de dialyse et le patient. Il est connu depuis longtemps que des contaminants dangereux peuvent
être présents dans l’eau et les concentrés utilisés pour préparer le liquide de dialyse. Pour réduire ce risque
au minimum, l’ISO 23500-3 et l’ISO 23500-4 définissent des exigences de qualité applicables à l’eau et aux
concentrés utilisés pour préparer le liquide de dialyse. Cependant, si le liquide de dialyse n’est pas préparé
avec soin, il peut contenir des niveaux inacceptables de contaminants, même s’il est préparé à partir d’eau
et de concentrés conformes aux exigences de l’ISO 23500-3 et de l’ISO 23500-4. De plus, le liquide de dialyse
peut être utilisé comme matière première pour la préparation en ligne de liquides destinés à être injectés
au patient, par exemple dans le cadre de thérapies telles que l’hémodiafiltration en ligne. Pour ces raisons,
le présent document a été élaboré pour compléter les Normes internationales existantes relatives à l’eau et
aux concentrés, respectivement l’ISO 23500-3 et l’ISO 23500-4. L’ISO 23500-1 donne des lignes directrices
destinées à aider l’utilisateur à se conformer systématiquement aux exigences du présent document et à
l’ISO 23500-3.
Les techniques de mesurage en vigueur au moment de l’élaboration sont citées dans ces Normes
internationales. D’autres méthodes normalisées peuvent être utilisées, à condition d’avoir été validées de
manière appropriée et qu’elles soient comparables aux méthodes citées. La justification de l’élaboration du
présent document est fournie à l’Annexe A.
Le présent document reflète le travail consciencieux des professionnels de santé, des patients et des
fabricants de dispositifs médicaux pour développer des recommandations applicables à la qualité des
liquides de dialyse. Le présent document est applicable aux professionnels de santé chargés de gérer les
centres de dialyse et de soigner les patients traités dans les centres de dialyse, étant donné qu’ils sont
responsables de la préparation finale du liquide de dialyse.
Le présent document vise à protéger les patients sous hémodialyse contre les effets indésirables dus aux
contaminants chimiques et microbiologiques connus susceptibles d’être présents dans un liquide de dialyse
mal préparé. Toutefois, le médecin en charge de la dialyse a la responsabilité ultime de s’assurer que le
liquide de dialyse est correctement formulé et qu’il est conforme aux normes de qualité en vigueur.
Il convient de ne pas considérer les concepts inclus dans le présent document comme inflexibles ou
immuables. Il convient de relire régulièrement les exigences et recommandations énoncées dans le présent
document afin de comprendre que le rôle de la pureté du liquide de dialyse est important eu égard aux
résultats médicaux du patient et aux développements technologiques.
v
Norme internationale ISO 23500-5:2024(fr)
Préparation et management de la qualité des liquides
d'hémodialyse et de thérapies annexes —
Partie 5:
Qualité des liquides de dialyse pour hémodialyse et thérapies
apparentées
1 Domaine d’application
Le présent document spécifie les exigences minimales de qualité chimique et microbiologique pour les
liquides de dialyse dans le cadre d’hémodialyses et de thérapies apparentées.
Le présent document s’applique à ce qui suit:
— les liquides de dialyse utilisés à des fins d’hémodialyse et d’hémodiafiltration;
— le liquide de substitution produit en ligne à des fins d’hémodiafiltration et d’hémofiltration sur la base du
liquide de dialyse.
Le présent document ne s’applique pas à ce qui suit:
— l’eau et les concentrés utilisés pour préparer le liquide de dialyse ou l’équipement permettant de produire
du liquide de dialyse;
— les systèmes de régénération de liquide de dialyse à base de sorbants qui régénèrent et recyclent de
petites quantités de liquide de dialyse;
— les systèmes d’épuration extrarénale continue qui utilisent des solutions prêtes à l’emploi; et
— les systèmes et solutions utilisés en dialyse péritonéale.
La fourniture et la surveillance de la composition du liquide de dialyse et ses écarts admis par rapport aux
points de consigne sont régis par des systèmes de protection définis dans l’IEC 60601-2-16.
2 Références normatives
Les documents suivants sont cités dans le texte de sorte qu’ils constituent, pour tout ou partie de leur
contenu, des exigences du présent document. Pour les références datées, seule l’édition citée s’applique. Pour
les références non datées, la dernière édition du document de référence s’applique (y compris les éventuels
amendements).
ISO 23500-1, Préparation et management de la qualité des liquides d’hémodialyse et de thérapies annexes —
Partie 1: Exigences générales
ISO 23500-3, Préparation et management de la qualité des liquides d’hémodialyse et de thérapies annexes —
Partie 3: Eau pour hémodialyse et thérapies apparentées
ISO 23500-4, Préparation et management de la qualité des liquides d’hémodialyse et de thérapies annexes —
Partie 4: Concentrés pour hémodialyse et thérapies apparentées
3 Termes et définitions
Pour les besoins du présent document, les termes et définitions de l’ISO 23500-1 s’appliquent.
L’ISO et l’IEC tiennent à jour des bases de données terminologiques destinées à être utilisées en normalisation,
consultables aux adresses suivantes:
— ISO Online browsing platform: disponible à l’adresse https:// www .iso .org/ obp
— IEC Electropedia: disponible à l’adresse https:// www .electropedia .org/
4 Exigences
4.1 Contaminants microbiologiques dans le liquide de dialyse
4.1.1 Généralités
Les exigences contenues dans l’Article 4 s’appliquent à un échantillon de liquide de dialyse recueilli à l’entrée
du dialyseur ou au point de réinjection.
4.1.2 Exigences microbiologiques relatives au liquide de dialyse standard
Le liquide de dialyse standard doit contenir un nombre total de microbes viables de moins de 100 UFC/ml
(lorsque soumis à essai conformément à l’Article 5) et doit présenter une concentration d’endotoxines de
moins de 0,5 UE/ml (lorsque soumis à essai conformément à l’Article 5).
Il convient que les niveaux d’action applicables au nombre total de microbes viables et à la concentration
d’endotoxines dans le liquide de dialyse soient également fixés selon les dynamiques microbiennes du
système. Généralement, les niveaux d’action sont fixés à 50 % des niveaux maximaux admissibles pour le
nombre total de microbes viables et pour la concentration d’endotoxines; d’autres niveaux peuvent être
définis.
Si le nombre de microbes dépasse les niveaux d’action dans le liquide de dialyse, il convient de prendre
rapidement des mesures correctives telles qu’une désinfection et un nouvel essai pour réduire les niveaux.
Il existe une possibilité de présence de champignons (levures et champignons filamenteux) associée à la
présence de bactéries et d’endotoxines dans le liquide de dialyse.
Des essais portant sur la croissance microbienne et les endotoxines ne sont pas exigés si le circuit de liquide
du dialyseur est équipé d’un filtre de rétention de bactéries et d’endotoxines de capacité appropriée validé
par le fabricant et utilisé et examiné conformément aux instructions du fabricant, sauf si le fabricant exige
de réaliser ces essais dans les instructions d’utilisation.
4.1.3 Exigences microbiologiques relatives au liquide de dialyse ultrapur
Le liquide de dialyse ultrapur doit contenir un nombre total de microbes viables de moins de 0,1 UFC/ml
(lorsque soumis à essai conformément à l’Article 5) et doit présenter une concentration d’endotoxines de
moins de 0,03 UE/ml (lorsque soumis à essai conformément à l’Article 5). Si ces limites sont dépassées dans
le liquide de dialyse ultrapur, il convient de prendre des mesures correctives pour réduire les niveaux à
un niveau acceptable. L’utilisateur est responsable de l’examen de la bactériologie du liquide de dialyse du
système après l’installation. Il lui incombe d’établir une surveillance de routine régulière.
Des essais portant sur la croissance microbienne et les endotoxines ne sont pas exigés si le circuit de liquide
du dialyseur est équipé d’un filtre de rétention de bactéries et d’endotoxines de capacité appropriée validé
par le fabricant et utilisé et examiné conformément aux instructions du fabricant, sauf si le fabricant exige
de réaliser ces essais dans les instructions d’utilisation.
4.1.4 Exigences microbiologiques relatives au liquide de substitution préparé en ligne
Les exigences contenues dans le présent paragraphe s’appliquent au liquide préparé en ligne destiné à être
injecté au patient lorsqu’il entre dans le sang du patient.
Ce liquide doit être stérile et apyrogène.
Un liquide de substitution pour thérapies convectives, notamment l’hémodiafiltration et l’hémofiltration,
peut être produit en ligne par un procédé d’ultrafiltration avec des filtres de rétention des bactéries et des
endotoxines. Ce procédé en ligne doit être validé pour produire un liquide stérile et apyrogène.
La conformité du liquide produit en ligne aux exigences du présent document ne peut pas être démontrée
avec des modes opératoires d’essai classiques. Pour cette raison, la conformité au présent document doit
être garantie par le bon fonctionnement d’un système validé, vérifiée conformément aux instructions du
fabricant au moment de l’installation et confirmée par l’utilisateur à l’aide d’un programme de surveillance
et de maintenance régulier. L’utilisateur doit respecter les instructions d’utilisation du fabricant du système
validé et le programme de surveillance et de maintenance de l’utilisateur doit être conçu pour confirmer que
l’eau et les concentrés utilisés pour préparer le liquide de substitution répondent toujours aux exigences de
l’ISO 23500-3 et l’ISO 23500-4.
4.2 Composition chimique du liquide de dialyse
Le liquide de dialyse doit être préparé à partir d’eau satisfaisant aux exigences de l’ISO 23500-3 et à partir
de concentrés acide et bicarbonate conformes aux exigences de l’ISO 23500-4. L’eau et les concentrés
doivent être combinés conformément aux instructions de dilution du fabricant du concentré en utilisant des
systèmes de distribution de liquide de dialyse individuels, tels que spécifiés dans l’IEC 60601-2-16, ou un
système de distribution de liquide de dialyse centralisé.
4.3 Contaminants chimiques présents dans le liquide de dialyse
L’eau et les concentrés doivent être combinés en utilisant des systèmes individuels de distribution de liquide
de dialyse ou un système de distribution de liquide de dialyse centralisé fabriqué avec des matériaux qui ne
contribuent pas à la contamination chimique du liquide de dialyse final.
Les niveaux maximaux de contaminants chimiques autorisés dans l’eau utilisée pour préparer le liquide et
les concentrés de dialyse sont donnés dans l’ISO 23500-3 et sont également présentés à l’Annexe B (voir
les Tableaux B.1 et B.2), aux côtés des méthodes de détermination (voir le Tableau B.3). D’autres méthodes
d’analyse équivalentes peuvent être utilisées. Si les analyses des éléments traces répertoriés dans le
Tableau B.2 ne sont pas disponibles, une analyse des métaux lourds totaux peut être utilisée avec un niveau
maximal admissible de 0,1 mg/l.
5 Essais de conformité
5.1 Exigences microbiologiques
5.1.1 Échantillonnage
Dans certains dialyseurs plus récents, l’écoulement du liquide de dialyse s’arrête lorsque la conduite
d’évacuation est débranchée du dialyseur. Dans ce cas, les appareils sont équipés de ports d’échantillonnage
du liquide de dialyse accessibles avec une seringue. Les ports d’échantillonnage peuvent être désinfectés
avec de l’alcool et séchés à l’air. Il convient d’utiliser une seringue stérile pour extraire au moins 10 ml de
liquide de dialyse du port d’échantillonnage. La seringue remplie est mise au rebut et un échantillon frais
de liquide de dialyse est prélevé à l’aide d’une nouvelle seringue stérile. Pour les ports d’échantillonnage
constitués d’un septum simple pénétré par une aiguille, il n’est pas nécessaire d’utiliser une seconde
seringue. En l’absence de port d’échantillonnage et si le dialyseur le permet, des échantillons peuvent aussi
être prélevés immédiatement avant le dialyseur en débranchant le raccord d’entrée et en prélevant de façon
aseptique un échantillon ponctuel «libre/propre» après avoir laissé le liquide de dialyse circuler pendant au
moins 60 s, sauf indication contraire dans les instructions du fabricant.
Il convient de réaliser l’analyse de tout échantillon de liquide aussi rapidement que possible après le
prélèvement pour éviter toute modification imprévisible de la population microbienne. Si les échantillons ne
peuvent pas être analysés dans les 4 h suivant leur prélèvement, il convient de les conserver à <10 °C sans les
congeler pendant le transfert vers le laboratoire. Il convient d’éviter de stocker les échantillons pendant plus
de 24 h et de les expédier conformément aux instructions du laboratoire.
5.1.2 Méthodes de culture
Une surveillance microbienne précise est importante dans le cadre de la détermination de la teneur
microbienne de l’eau et du liquide de dialyse. Les résultats de culture obtenus en utilisant les méthodes
décrites dans le présent document et récapitulées dans le Tableau 1 ne constituent qu’un indicateur relatif
de la biocharge et ne fournissent pas une mesure de la charge microbienne absolue.
Le nombre total de microbes viables (dénombrements sur boîtes normalisés) doit être obtenu en utilisant
des modes opératoires d’essai microbiologique conventionnels (boîte d’ensemencement en profondeur, boîte
d’ensemencement en surface, membrane filtrante). La technique de l’anse étalonnée ne doit pas être utilisée.
Les méthodes et volumes de prélèvement privilégiés sont les suivants:
— pour du liquide de dialyse standard:
— dénombrement en surface, de 0,1 ml à 0,3 ml;
— boîte d’ensemencement en profondeur, généralement 1 ml;
— pour du liquide de dialyse ultrapur: filtration sur membrane, de 10 ml à 1 000 ml;
— pour du liquide de substitution: la stérilité ne peut pas être prouvée par échantillonnage.
Les différents types de milieux et périodes d’incubation peuvent donner lieu à des concentrations dans les
colonies et à des types de micro-organismes récupérés variables.
Des études publiées ont montré que l’utilisation de gélose R2A (Reasoner 2A) donnait lieu à des
dénombrements de colonies plus élevés qu’avec la gélose trypticase soja (TSA) pour la culture d’échantillons
[20][21] [22]
d’eau et de liquides de dialyse. Cependant, dans une publication plus récente, les auteurs ont
indiqué que les comparaisons de la charge bactérienne de l’eau de dialyse standard et du liquide de dialyse
standard n’occasionnaient pas de différence significative et qu’ils produisaient des dénombrements
de colonies ≥ 50 UFC/ml lorsqu’ils sont soumis à essai sur gélose R2A et gélose TSA dans les conditions
indiquées dans le Tableau 1.
La gélose de tryptone, glucose et levure (TGEA) incubée entre 17 °C et 23 °C pendant 7 jours dans des
études antérieures a également donné des dénombrements de colonies plus élevés que la TSA. Dans la
Référence [22], une comparaison de ce milieu avec la TSA a montré que la proportion d’échantillons d’eau de
dialyse standard produisant des dénombrements de colonies ≥ 50 UFC/ml était significativement différente
de celle trouvée avec la TSA soumise à une température d’incubation de 35 °C à 37 °C pendant 48 h (p = 0,001).
Les proportions d’échantillons de liquide de dialyse dans lesquels la charge microbienne était ≥ 50 UFC/ml
n’ont pas présenté de différence significative sur les deux milieux et dans les deux conditions d’incubation
respectives.
Il convient de choisir le milieu de culture et les temps d’incubation selon le type de liquide à analyser, par
exemple liquide de dialyse standard, eau utilisée pour la préparation du liquide de dialyse standard, liquide
de dialyse ultrapur, eau utilisée pour la préparation du liquide de dialyse ultrapur ou liquide utilisé pour les
thérapies en ligne telles que l’hémodiafiltration. Il convient de choisir la méthode en s’appuyant sur l’analyse
des avantages, des inconvénients et de la sensibilité de chacune des méthodes suggérées. Il convient
également de s’assurer que la sécurité des patients est garantie tout en permettant la prise en compte des
pratiques de travail du laboratoire local et que les exigences de remboursement peuvent être respectées.
Les géloses au sang et au chocolat ne doivent pas être utilisées.
Tableau 1 — Techniques de culture
Milieu de culture Température d’incubation Temps d’incubation
TGEA 17 °C à 23 °C 7 jours
R2A 17 °C à 23 °C 7 jours
a
TSA 35 °C à 37 °C 48 h
a [22]
L’utilisation de TSA n’a été validée que pour l’eau de dialyse et le liquide de dialyse standard .
D’autres milieux, conditions d’incubation et temps de dénombrement de colonies peuvent être utilisés
à condition qu’il ait été prouvé que ces méthodes ont été validées de manière appropriée et qu’elles sont
comparables aux méthodes citées.
Il n’existe actuellement aucune exigence relative à la surveillance de routine de la présence de champignons
(à savoir levures et champignons filamenteux); toutefois, si leur quantification est exigée, la filtration sur
membrane est suggérée comme méthode pour obtenir un échantillon approprié pour l’analyse. De la gélose
de Sabouraud ou de la gélose à l’extrait de malt (MEA) sont recommandées pour la culture.
La détection des endotoxines bactériennes, provenant de bactéries à Gram négatif, s’effectue principalement
à l’aide du lysat d’amébocytes de limule (LAL), obtenu à partir de sang de limule (Limulus polyphemus ou
Tachypleus tridentatus). Les chapitres correspondants ont été harmonisés entre la Pharmacopée européenne
[16] [13]
((EP) <2.6.14Y>), la Pharmacopée américaine et le States-National Formulary (<85>) et la Pharmacopée
[19]
japonaise (<4.01>) .
Le test LAL est fondé sur la cascade de coagulation humorale du limule Limulus polyphemus. La première
enzyme de cette cascade de coagulation réagit avec l’endotoxine et est appelée facteur C. Ce facteur est
désormais produit par recombinaison (biotechnologiquement) et est proposé comme essai rFC par plusieurs
fabricants pour la détermination des endotoxines bactériennes. L’essai par la méthode rFC est au moins
aussi sensible et fiable que le test LAL, mais est moins sensible à certains facteurs interférents et aux
fluctuations entre lots. En raison de la production biotechnologique, aucun animal vivant n’est requis en tant
que donneurs de sang.
[17]
Cette nouvelle méthode a été intégrée à la Pharmacopée européenne <2.6.32> et sera également incluse
[14]
dans l’USP-NF <1085.1> .
La conformité aux normes microbiennes pour le liquide de dialyse ultrapur et le liquide de substitution
préparés en ligne avec un système validé peut être vérifiée en respectant les exigences et les instructions du
fabricant du système de distribution de liquide de dialyse.
5.2 Exigences chimiques
La conformité aux exig
...
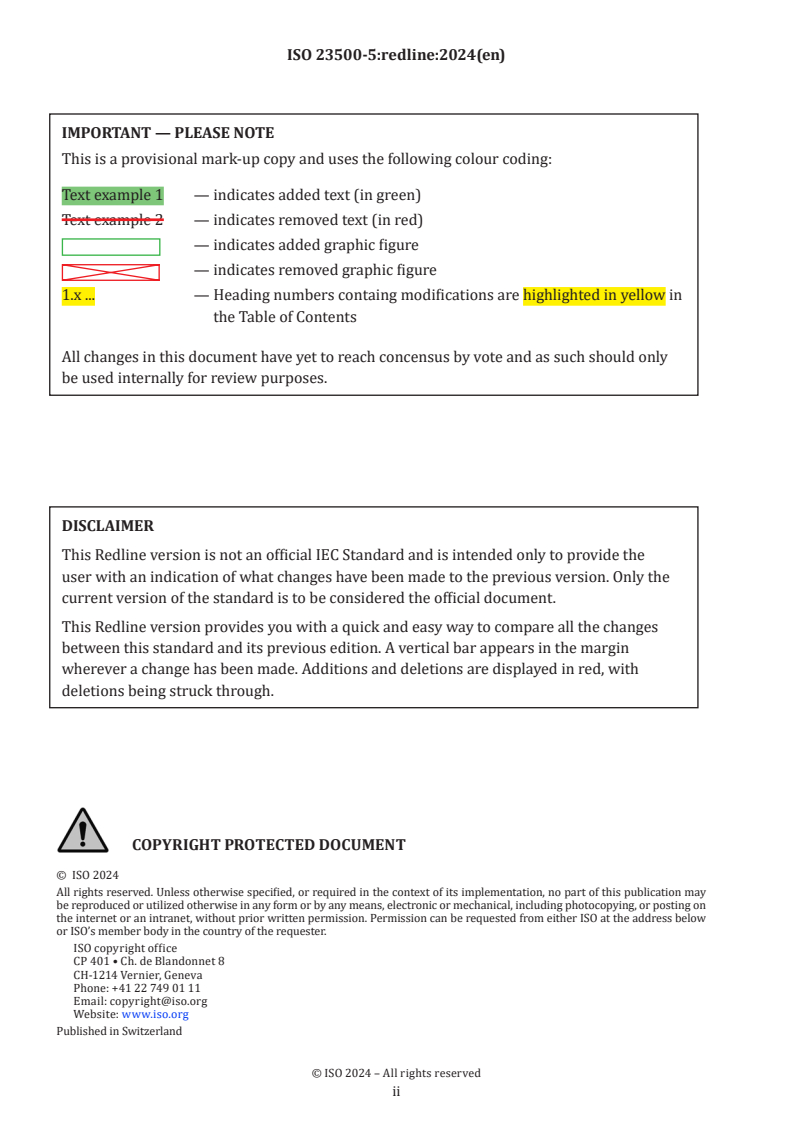
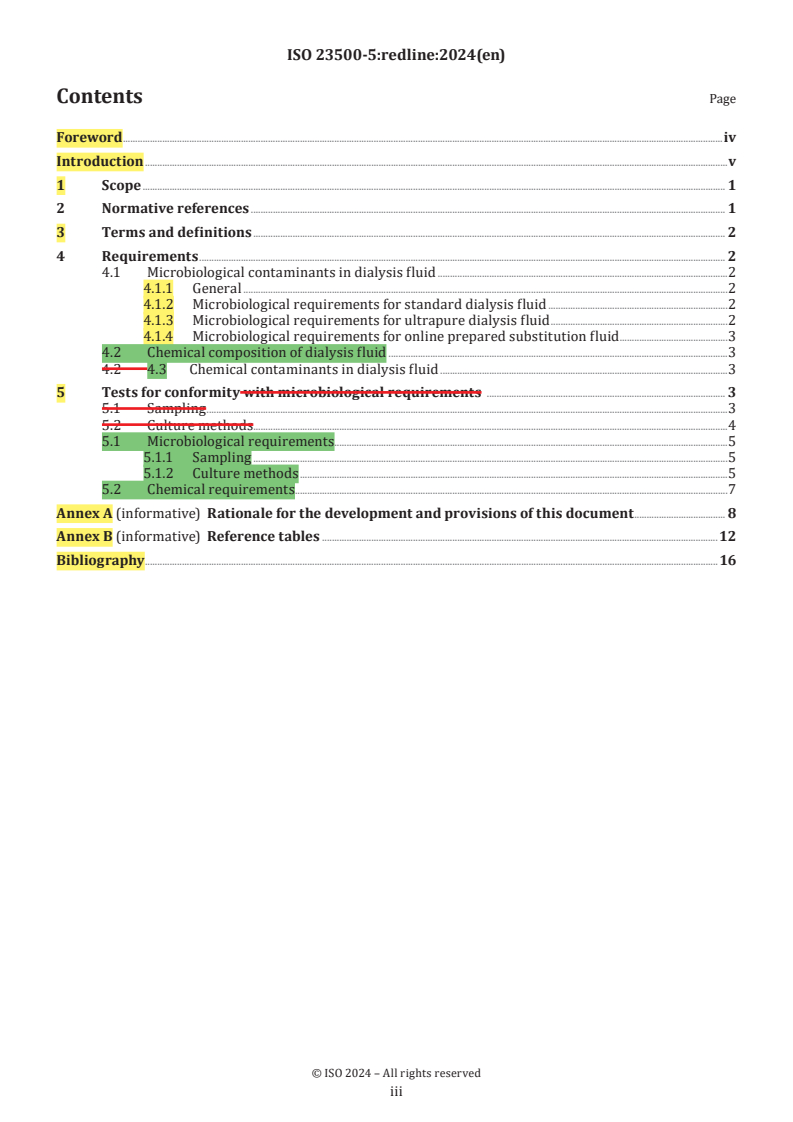
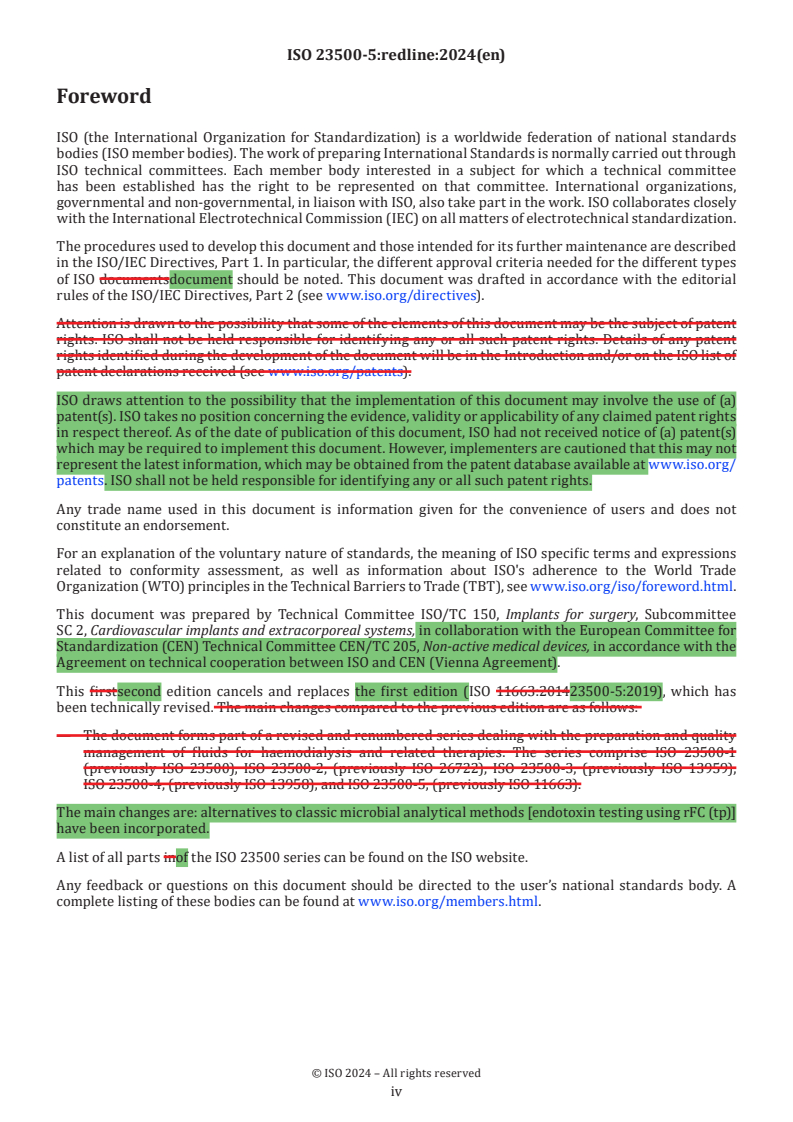
Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...