ASTM F2129-01
(Test Method)Standard Test Method for Conducting Cyclic Potentiodynamic Polarization Measurements to Determine the Corrosion Susceptibility of Small Implant Devices
Standard Test Method for Conducting Cyclic Potentiodynamic Polarization Measurements to Determine the Corrosion Susceptibility of Small Implant Devices
SCOPE
1.1 This test method assesses the corrosion susceptibility of small, metallic, implant medical devices, or components thereof, using cyclic (forward and reverse) potentiodynamic polarization. Examples of device types, which may be evaluated by this test method include, but are not limited to, vascular stents, filters, support segments of endovascular grafts, cardiac occluders, aneurysm or ligation clips, staples, and so forth.
1.2 This test method is used to assess a device in its final form and finish, as it would be implanted. These small devices should be tested in their entirety. The upper limit on device size is dictated by the electrical current delivery capability of the test apparatus (see Section 6). It is assumed that test methods, such as Test Methods G 5 and G 61 have been used for material screening.
1.3 Because of the variety of configurations and sizes of implants, this test method provides a variety of specimen holder configurations.
1.4 This test method is intended for use on implantable devices made from metals with a relatively high resistance to corrosion.
1.5This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superceded and replaced by a new version or discontinued.
Contact ASTM International (www.astm.org) for the latest information.
Designation: F 2129 – 01
Standard Test Method for
Conducting Cyclic Potentiodynamic Polarization
Measurements to Determine the Corrosion Susceptibility of
Small Implant Devices
This standard is issued under the fixed designation F 2129; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (e) indicates an editorial change since the last revision or reapproval.
1. Scope G 61 Test Method for Conducting Cyclic Potentiodynamic
Polarization Measurements for Localized Corrosion Sus-
1.1 This test method assesses the corrosion susceptibility of
ceptibility of Iron-, Nickel-, or Cobalt-Based Alloys
small, metallic, implant medical devices, or components
G 102 Practice for Calculation of Corrosion Rates and
thereof, using cyclic (forward and reverse) potentiodynamic
Related Information from Electrochemical Measurements
polarization. Examples of device types, which may be evalu-
ated by this test method include, but are not limited to, vascular
3. Terminology
stents, filters, support segments of endovascular grafts, cardiac
3.1 Definitions:
occluders, aneurysm or ligation clips, staples, and so forth.
3.1.1 potentiostat, n—an instrument for automatically main-
1.2 This test method is used to assess a device in its final
taining an electrode in an electrolyte at a constant potential or
form and finish, as it would be implanted. These small devices
controlled potentials with respect to a suitable reference
should be tested in their entirety. The upper limit on device size
electrode (see Terminology G 15).
is dictated by the electrical current delivery capability of the
3.1.2 potentiodynamic cyclic polarization (forward and re-
test apparatus (see Section 6). It is assumed that test methods,
verse polarization), n—a technique in which the potential of
such as Test Methods G 5 and G 61 have been used for material
the test specimen is controlled and the corrosion current
screening.
measured by a potentiostat. The potential is scanned in the
1.3 Because of the variety of configurations and sizes of
positive or noble (forward) direction as defined in Practice G 3.
implants, this test method provides a variety of specimen
The potential scan is continued until a predetermined potential
holder configurations.
or current density is reached. Typically, the scan is run until the
1.4 This test method is intended for use on implantable
transpassive region is reached, and the specimen no longer
devices made from metals with a relatively high resistance to
demonstrates passivity, as defined in Practice G 3. The poten-
corrosion.
tial scan direction then is reversed until the specimen repassi-
1.5 This standard does not purport to address all of the
vates or the potential reaches a preset value.
safety concerns, if any, associated with its use. It is the
3.1.3 scan rate, n—the rate at which the controlling voltage
responsibility of the user of this standard to establish appro-
is changed.
priate safety and health practices and determine the applica-
3.2 Symbols:
bility of regulatory limitations prior to use.
3.2.1 E = Breakdown or Critical Pitting Potential—the
b
2. Referenced Documents least noble potential at which pitting or crevice corrosion or
both will initiate and propagate as defined in Terminology
2.1 ASTM Standards:
G 15. An increase in the resistance to pitting corrosion is
D 1193 Specification for Reagent Water
associated with an increase in E .
G 3 Practice for Conventions Applicable to Electrochemical b
3.2.2 E or OCP—the potential of a corroding surface in
corr
Measurements in Corrosion Testing
an electrolyte relative to a reference electrode measured under
G 5 Reference Test Method for Making Potentiostatic and
open-circuit conditions, as defined in Terminology G 15.
Potentiodynamic Anodic Polarization Measurements
3.2.3 E = Final Potential—a preset potential at which the
f
G 15 Terminology Relating to Corrosion and Corrosion
scan is stopped.
Testing
3.2.4 E = Initial Potential—the potential at which the
i
potentiostat begins the controlled potentiodynamic scan.
This test method is under the jurisdiction of ASTM Committee F04 on Medical
3.2.5 E = Protection Potential—the potential at which the
p
and Surgical Materials and Devices and is the direct responsibility of Subcommittee
reverse scan intersects the forward scan at a value that is less
F04.15 on Material Test Methods.
noble than E . E cannot be determined if there is no
Current edition approved July 10, 2001. Published September 2001. b p
Annual Book of ASTM Standards, Vol 11.01.
breakdown. Whereas, pitting will occur on a pit-free surface
Annual Book of ASTM Standards, Vol 03.02.
Copyright © ASTM, 100 Barr Harbor Drive, West Conshohocken, PA 19428-2959, United States.
NOTICE: This standard has either been superceded and replaced by a new version or discontinued.
Contact ASTM International (www.astm.org) for the latest information.
F 2129
above E , it will occur only in the range of potentials between 6. Apparatus
b
E and E if the surface is already pitted. The severity of
p b
6.1 Potentiostat, capable of maintaining an electrode poten-
crevice corrosion susceptibility increases with increasing hys-
tial within 1 mV of a preset value over a wide range of
teresis of the polarization curve, the difference between E and
b
potentials, as described in Test Methods G 5 and G 61. The
E .
p
potential measuring circuit should have a high input imped-
3.2.6 E = Vertex Potential—a preset potential, at which the 11 14
v
ance, that is, on the order of 10 to 10 V. The current
scan direction is reversed.
measuring circuit should be capable of measuring current in the
3.2.7 i = Corrosion Current Density (mA/cm )—the 5
corr
range of 1.0 to 10 μA.
corrosion current density is extrapolated from the anodic and
6.2 Working Electrode, to be used as the test specimen. Its
cathodic Tafel regions to the OCP (in accordance with Practice
configuration and holder will depend on the type of specimen
G 102).
being tested, as described in Section 7. In all cases, the
3.2.8 i = Threshold Current Density (mA/cm )—a preset
t
metallurgical and surface condition of a specimen simulating a
current density, at which the scan direction is reversed.
device must be in the same condition as the device.
Typically, the scan is reversed when a current density two
6.2.1 An appropriate reference medical device in its final
decades higher than the current density at the breakdown
form and finish, as it would be implanted, should be used as a
potential (E ) is reached.
b
reference or control. Appropriate reference device shall consist
of a device, which is similar to the investigated device and has
4. Summary of Test Method
a history of good corrosion resistance in vivo, is used in a
4.1 The device is placed in an appropriate deaerated simu-
similar environment or location and is used to treat a similar
lated physiological solution and the corrosion potential (E )
corr
disease. Again, as for the working electrode, the configuration
is monitored for 1 h. The potentiodynamic scan is then started
and holder will depend on the type of reference specimen
at an initial potential (E ) 100 mV more negative than E , and
i corr
tested.
scanned in the positive or noble (forward) direction. The scan
6.3 Reference Electrode—A saturated calomel electrode
is reversed after the current density has reached a value
(SCE), as defined in Practice G 3, shall be used as a reference
approximately two decades greater than the current density
electrode.
measured at the breakdown potential. The reverse scan is
6.4 Salt Bridge, such as a Luggin probe, shall be used
stopped after the current has become less than that in the
between the working and reference electrode, such as the type
forward direction or the potential is 100 mV negative to E .
corr
shown in Test Method G 5.
The data is plotted with the current density in mA/cm on the
6.5 Auxiliary Electrodes:
x axis (logarithmic axis) versus the potential in mV on the y
axis (linear axis). Appropriate reference medical devices in 6.5.1 Two platinum auxiliary electrodes may be prepared
from high-purity rod stock. The surfaces may be platinized, as
their final form and finish, as they would be implanted, are used
as controls. per Test Method G 5.
6.5.2 Alternatively, high-purity graphite auxiliary electrodes
5. Significance and Use
may be used in accordance with Test Method G 5. Care should
5.1 Corrosion of implantable medical devices can have
be taken to insure that they do not get contaminated during a
deleterious effects on the device performance or may result in
test.
the release of corrosion products with harmful biological
6.5.3 The auxiliary electrode surface area should be at least
consequences; therefore, it is important to determine the
four times greater than the sample surface area. Use of
general corrosion behavior as well as the susceptibility of the
wire-mesh platinum might be more cost-effective than plati-
devices to localized corrosion.
num cylinders when testing larger specimens or whole devices.
5.2 The forming and finishing steps used to create an
6.6 Suitable Polarization Cell, with a volume of about 1000
implantable device may have significant effects on the corro-
cm , equivalent to or similar to that recommended in Test
sion resistance of the material out of which the device is
Method G 5.
fabricated. While testing the corrosion resistance of the mate-
6.7 Water Bath, or other heating appliance capable of
rials is essential in the process of selecting materials to be used,
maintaining the test solution temperature at 37 6 1°C.
it does not necessarily provide critical data regarding device
6.8 Purge Gas Delivery System, capable of delivering nitro-
performance.
gen gas at 150 cm /min.
5.3 To accommodate the wide variety of device shapes and
sizes encountered, a variety of holding devices can be used.
7. Specimen Holders
5.4 Note that the method is intentionally designed to reach
7.1 There are a variety of holders that may be used in this
conditions that are sufficiently severe to cause breakdown and
practice. Each is designed for a specific type or class of device.
deterioration of the medical devices and that these conditions
7.2 Short wire or coil specimens.
may not be necessarily encountered in vivo. The results of this
corrosion test conducted in artificial physiological electrolytes 7.2.1 Specimens can be held suspended from a clamping
can provide useful data for comparison of different device device. For example, the threaded end of a Test Method G 5
materials, designs, or manufacturing processes. However, note holder can be used to hold two stainless steel nuts. The wire
that this test method does not take into account the effects of test specimen is clamped between these nuts and bent so as to
cells, proteins, and so forth on the corrosion behavior in vivo. enter the test solution.
NOTICE: This standard has either been superceded and replaced by a new version or discontinued.
Contact ASTM International (www.astm.org) for the latest information.
F 2129
7.2.2 The surface area of the test specimen shall be calcu- the Committee on Analytical Reagents of the American Chemi-
cal Society.
lated based on the length of wire or coil immersed in the test
solution. 8.1.1 The water shall be distilled or deionized conforming
to the purity requirements of Specification D 1193, Type IV
7.2.3 This type of holder exposes the specimen to the
reagent water.
air-liquid interface, which is subject to localized crevice
8.1.2 The standard test solution should be prepared accord-
corrosion. Test specimens should be examined carefully after
ing to the specifications. As a reference, a list of common
testing to ensure that there is no localized corrosion at or just
physiological solutions and their composition is provided in
below the interface.
Appendix X2.
7.2.4 If specimens show evidence of localized corrosion at
8.1.3 The pH of the electrolyte should be adjusted based on
the air-liquid interface, then the portion of the specimen
the nature of the solution by the addition of NaOH or HCl.
passing across this interface shall be sealed with an impervious
8.1.4 High-purity nitrogen gas for purge should be used
coating.
when possible depending on the nature of the solution used.
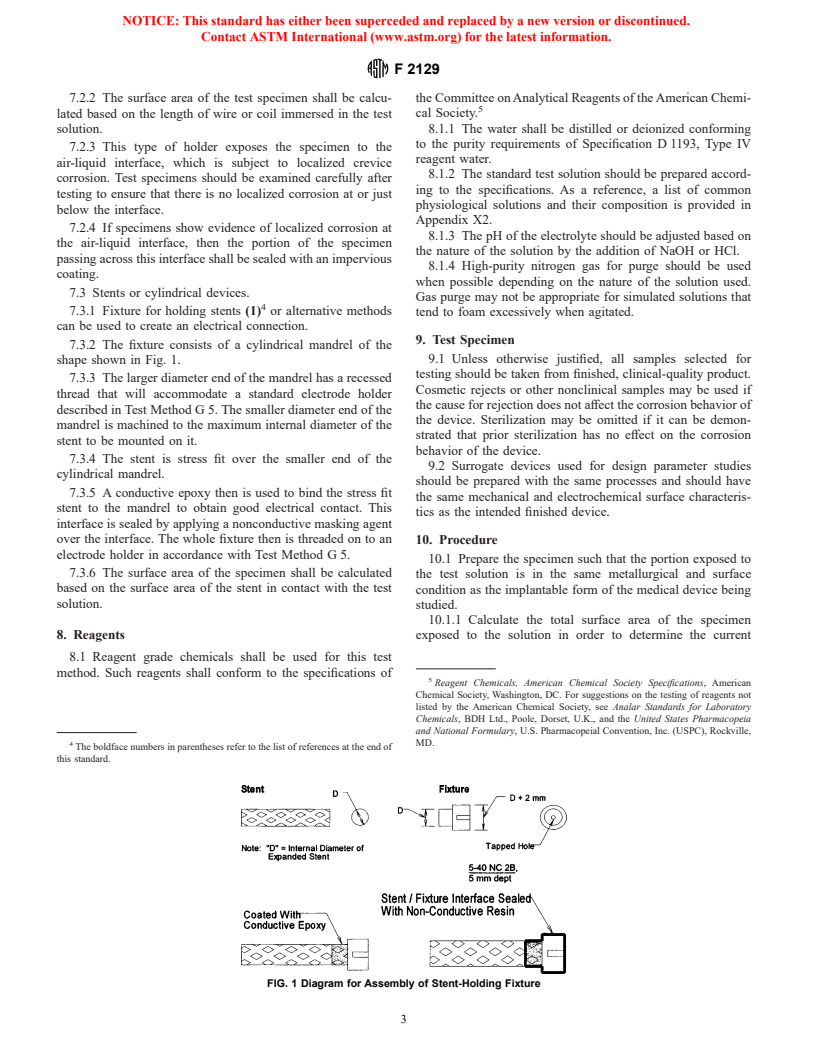
7.3 Stents or cylindrical devices.
Gas purge may not be appropriate for simulated solutions that
7.3.1 Fixture for holding stents (1) or alternative methods
tend to foam excessively when agitated.
can be used to create an electrical connection.
9. Test Specimen
7.3.2 The fixture consists of a cylindrical mandrel of the
9.1 Unless otherwise justified, all samples selected for
shape shown in Fig. 1.
testing should be taken from finished, clinical-quality product.
7.3.3 The larger diameter end of the mandrel has a recessed
Cosmetic rejects or other nonclinical samples may be used if
thread that will accommodate a standard electrode holder
the cause for rejection does not affect the corrosion behavior of
described in Test Method G 5. The smaller diameter end of the
the device. Sterilization may be omitted if it can be demon-
mandrel is machined to the maximum internal diameter of the
strated that prior sterilization has no effect on the corrosion
stent to be mounted on it.
behavior of the device.
7.3.4 The stent is stress fit over the smaller end of the
9.2 Surrogate devices used for design parameter studies
cylindrical mandrel.
should be prepared with the same processes and should have
7.3.5 A conductive epoxy then is used to bind the stress fit
the same mechanical and electrochemical surface characteris-
stent to the mandrel to obtain good electrical contact. This
tics as the intended finished device.
interface is sealed by applying a nonconductive masking agent
over the interface. The whole fixture then is threaded on to an 10. Procedure
electrode holder in accordance with Test Method G 5.
10.1 Prepare the specimen such that the portion exposed to
7.3.6 The surface area of the specimen shall be calculated
the test solution is in the same metallurgical and surface
based on the surface area of the stent in contact with the test
condition as the implantable form of the medical device being
solution.
studied.
10.1.1 Calculate the total surface area of the specimen
8. Reagents exposed to the solution in order to determine the current
8.1 Reagent grade chemicals shall be used for this test
method. Such reagents shall conform to the specifications of
Reagent Chemicals, American Chemical Society Specifications, American
Chemical Society, Washington, DC. For sugge
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.